About cellulitis
Cellulitis is an infection of the deeper layers of skin and underlying tissue that develops suddenly and can spread quickly through the body if not treated promptly. Most cases are successfully treated with antibiotics, but severe infections may require hospitalization.
Symptoms of Cellulitis
Common symptoms include:
- Red, hot, swollen, painful, and tender skin in the affected area.
- Fever (temperature of 38°C/100.4°F or above), shaking chills (rigors), nausea and vomiting, dizziness, or confusion in severe cases. It most commonly affects the lower legs but can appear anywhere on the body.

When to Seek Help
Pharmacy First Scotland: Adults 18+ with cellulitis symptoms, especially linked to insect bites, can consult a pharmacist for advice and treatment, or they may be referred to a GP.
Urgent Medical Attention: Call 999 or visit A&E if:
- The face or area around the eye is affected.
- Symptoms rapidly worsen.
- Fever or vomiting accompanies the skin changes.
- You have a weakened immune system or severe lymphoedema.
- Young children or the elderly are affected.
Treatment for Cellulitis
- Antibiotics: Usually given as tablets for mild cases, with a typical five-day course. Severe infections may require antibiotics via injection or a drip in hospital.
- Treatment Monitoring: Symptoms should improve within a few days. Contact your GP if they worsen or do not improve after a week.
Outlook and Potential Complications
Most people make a full recovery with prompt antibiotic treatment. However, untreated cellulitis can cause serious complications, such as:
- Blood poisoning (sepsis)
- Kidney damage
- Leg ulcers These require immediate hospital care.
Causes of Cellulitis
Cellulitis is typically caused by bacterial infections entering a break in the skin, such as:
- Bruises, cuts, or grazes
- Animal or insect bites
- Leg ulcers
- Dry, cracked skin (from eczema or athlete’s foot)
Prevention Tips
To reduce your risk of developing cellulitis:
- Keep skin moisturized to prevent dryness and cracking.
- Manage conditions like eczema, athlete’s foot, and leg ulcers effectively.
- Maintain good hygiene, especially for wounds.
- Consider long-term antibiotics if cellulitis recurs frequently.
With prompt treatment and proper care, cellulitis can be managed effectively to avoid complications and achieve a full recovery.
Symptoms of cellulitis
Cellulitis is a sudden bacterial infection of the deeper layers of the skin and underlying tissues. It can progress quickly and may become life-threatening if not treated promptly. Here is an overview of the symptoms and when to seek medical attention.
Skin Symptoms
Cellulitis causes the affected skin to become:
- Red
- Hot
- Swollen
- Painful
- Tender In some cases, there may also be:
- Breaks in the skin
- Pus or blood-filled blisters
Common areas affected include the lower legs, feet, arms, hands, and sometimes the face, particularly around the eyes.
If you notice sudden redness, pain, and warmth in any area of your skin, contact your GP or visit a minor injuries unit immediately.

Additional Symptoms
Before or along with skin changes, you may experience:
- General unwellness
- Nausea
- Shivering or chills
Serious Symptoms Indicating Infection Spread
In some cases, cellulitis can spread deeper and cause serious, life-threatening symptoms, such as:
- High fever (temperature of 38°C/100.4°F or above)
- Rapid heartbeat or breathing
- Nausea or vomiting
- Diarrhoea
- Dizziness or fainting
- Confusion or disorientation
- Cold, clammy, pale skin
- Unresponsiveness or loss of consciousness
If you experience any of these symptoms along with skin changes, call 999 or go to the nearest A&E department immediately.
Prompt medical attention and treatment, usually involving antibiotics, are critical for managing cellulitis effectively and preventing complications.
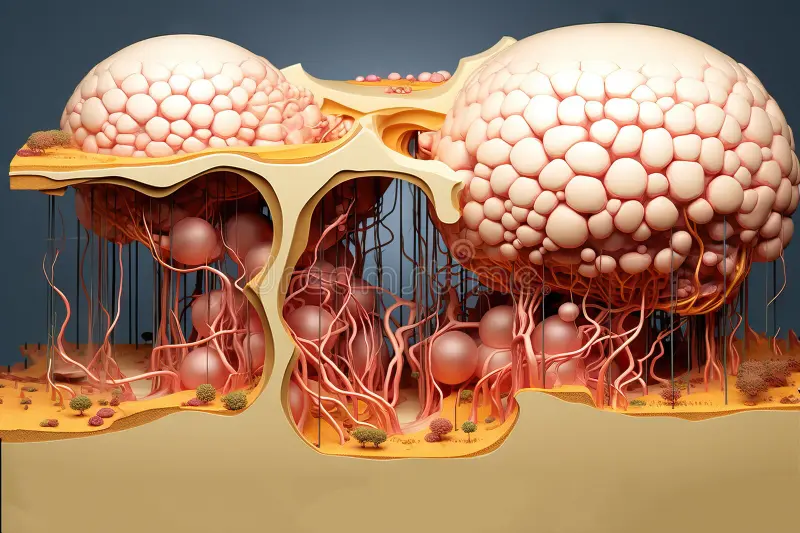
Causes of cellulitis
Cellulitis is a bacterial infection that affects the deeper layers of the skin and underlying tissue, typically caused by bacteria such as Streptococcus or Staphylococcus. Here’s a closer look at how and why it occurs, as well as risk factors associated with the condition.
How the Infection Occurs
The bacteria responsible for cellulitis often live harmlessly on the skin’s surface. However, they can enter deeper layers of skin through breaks, resulting in infection. The break in the skin may be so small that it goes unnoticed. Common entry points include:
- Cuts or grazes
- Burns
- Animal or human bites
- Insect bites
- Puncture wounds
- Leg ulcers
- Dry, cracked skin caused by conditions like eczema or athlete’s foot
Spread and Contagion
Cellulitis usually occurs deep within the skin layers, so it isn’t normally spread from person to person. The infection primarily results from bacteria that are already present on or around the skin’s surface.
Factors that Increase Risk
While anyone can develop cellulitis, your risk may be higher if you have:
- Obesity – Excess weight may contribute to swelling and decreased circulation.
- Poor circulation in the arms, legs, hands, or feet – This can slow the body’s ability to fight infection.
- Weakened immune system – Conditions like HIV, certain medications, or chemotherapy treatment can impair the immune system.
- Lymphoedema – This condition, which causes a build-up of fluid under the skin, can lead to swelling and increase the risk of infection.
- Poorly controlled diabetes – High blood sugar levels can impair immune response and increase the risk of skin infections.
- Previous cellulitis – If you have had cellulitis before, you may be more likely to experience it again.
- Injected drug use – Sharing needles or injecting drugs can increase the risk of introducing bacteria to the body.
Prevention Tips
Managing the underlying health conditions mentioned above and practicing proper hygiene can help reduce the risk of cellulitis. This may involve:
- Keeping skin clean and moisturized to prevent dryness and cracking.
- Promptly cleaning and covering cuts, grazes, and wounds.
- Managing conditions like diabetes and lymphedema with appropriate medical care.
- Seeking timely medical attention for wounds or infections.
Understanding these causes and risk factors can aid in preventing cellulitis and catching it early if it develops.
Treating cellulitis
Treating Cellulitis involves the use of antibiotics, which can often be managed at home. However, severe cases may require hospital care. Here’s how it is treated and managed:
Treatment at Home
1. Antibiotics
- Prescription: You’ll typically be prescribed antibiotic tablets to take two to four times daily for about a week.
- Duration: If symptoms don’t improve within a week or if you have an underlying condition (like lymphoedema) making treatment more challenging, you may need a longer course of antibiotics.
- Common antibiotics: These include flucloxacillin and clarithromycin.
- Side effects: Potential side effects can include an upset stomach or diarrhoea.
- Symptoms worsening: Your symptoms might worsen during the first 48 hours of treatment but should start improving soon afterward.
- Complete the course: It’s crucial to finish the full antibiotic course as prescribed, even if you start feeling better.
2. Self-Care During Recovery To help ease symptoms and promote recovery:
- Pain relief: Take paracetamol or ibuprofen to relieve pain.
- Reduce swelling: Elevate the affected body part (e.g., resting your leg on pillows if it’s affected).
- Movement: Regularly move the joint near the affected area (e.g., wrist, ankle) to prevent stiffness.
- Stay hydrated: Drink plenty of fluids to prevent dehydration.
- Compression stockings: If you usually wear them (e.g., for lymphoedema), avoid use until you’ve recovered.
When to Seek Further Medical Advice
Contact your GP immediately if:
- Your symptoms worsen within 48 hours of starting treatment.
- Your symptoms haven’t improved after a week.
- You develop additional symptoms, such as a fever or vomiting.
Treatment in Hospital
In severe cases:
- Intravenous antibiotics: You may need antibiotics delivered directly into your vein through an injection or a drip.
- Continuing care: Once your symptoms improve, you can often transition to antibiotic injections or tablets at home or in an outpatient setting, reducing the need for hospital stays.
Prompt treatment and adherence to prescribed care are essential to effectively manage cellulitis and prevent complications.