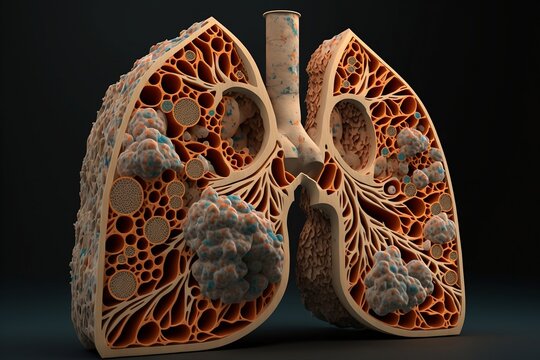
What is Bronchiectasis?
Bronchiectasis is a chronic lung condition where the airways become abnormally widened. This widening leads to the accumulation of mucus, which can make it easier for infections to develop. It can affect individuals of any age, but symptoms often become noticeable later in life, usually in middle age.
Symptoms of Bronchiectasis
The symptoms of bronchiectasis can vary but may include:
- Persistent Cough: Usually accompanied by mucus (phlegm) production.
- Recurrent Chest Infections: Frequent infections that may be harder to treat.
- Fatigue: Constant tiredness, which may be due to infections and inflammation.
Symptoms often worsen when there is a lung infection.
When to Seek Medical Advice
- Emergency: Dial emergency services or 111 (UK) if you experience:
- Blue-tinged skin or lips (a sign of low oxygen).
- Confusion or disorientation.
- High fever (38°C/100.4°F or above).
- Rapid breathing (more than 25 breaths per minute).
- Severe chest pain that makes it difficult to cough.
- Non-Emergency: Speak to a GP if you have a cough lasting more than three weeks.
Diagnosis of Bronchiectasis
Diagnosis involves:
- Initial GP Consultation: Your doctor will:
- Ask about your symptoms and history.
- Examine your lungs using a stethoscope (widened airways often produce a crackling noise).
- Conduct an X-ray to rule out other lung conditions.
- Collect a mucus sample for bacterial analysis if a lung infection is suspected.
- Specialist Referral: Additional tests may include:
- CT Scan: To assess airway widening and chronic infection.
- Blood Tests: To evaluate immune function.
- Mucus (Sputum) Test: To identify bacteria or fungi.
- Throat Swab: To detect viruses.
- Genetic Screening Test: For conditions like cystic fibrosis.
- Lung Function Tests: Measure airflow and lung capacity.
- Bronchoscopy: Inserting a camera-equipped tube to examine the lungs and collect samples.
Treatment of Bronchiectasis
The lung damage caused by bronchiectasis is irreversible, but treatment can alleviate symptoms and prevent further damage:
- Airway Clearance Techniques and Devices:
- Active Cycle of Breathing Techniques (ACBT): Includes cycles of breathing, deep breathing, and controlled coughing to clear mucus.
- Postural Drainage: Changing positions to encourage mucus clearance.
- Handheld Devices: Examples include Flutter, RC Cornet, Acapella, and Aerobika devices that use vibrations and air pressure to loosen mucus.
- Medications:
- Bronchodilators: Inhaled drugs that relax airway muscles to improve breathing.
- Examples: Salbutamol, Formoterol, Tiotropium.
- Antibiotics: Used to treat lung infections.
- Oral antibiotics may be prescribed for two weeks. Hospitalization may be required for severe infections needing IV antibiotics.
- Long-term antibiotics may be used for frequent infections.
- Nebulised Medications: Used to deliver medication directly to the lungs, such as saltwater solutions to thin mucus.
- Bronchodilators: Inhaled drugs that relax airway muscles to improve breathing.
Lifestyle and Preventative Measures
- Quit Smoking: Essential to prevent further lung damage.
- Vaccinations: Annual flu vaccine, pneumococcal vaccine, and COVID-19 vaccine.
- Exercise and Hydration: Regular physical activity and maintaining hydration help keep mucus thin and easier to clear.
- Healthy Weight Management: Supports overall lung health.
Surgical Treatment
- Rarely Recommended: Surgery may be considered if other treatments fail, and the lung damage is limited to one lobe.
Causes of Bronchiectasis
- Previous Infections: Such as pneumonia or whooping cough.
- Immune System Disorders: Problems with immune function can lead to persistent infections.
- Chronic Lung Conditions: Such as Chronic Obstructive Pulmonary Disease (COPD).
- Allergic Bronchopulmonary Aspergillosis (ABPA): A condition caused by an allergic reaction to fungal spores.
- Idiopathic Cases: In many cases, no specific cause is found.