About bladder cancer
Bladder cancer occurs when a growth of abnormal tissue, known as a tumor, develops within the bladder lining. In more severe cases, the tumor may spread into the surrounding muscles.
Recognizing the Symptoms of Bladder Cancer
The most common and often earliest symptom of bladder cancer is blood in the urine (hematuria). It is typically painless but may appear intermittently. If you notice blood in your urine, even if it comes and goes, it is essential to speak with a healthcare provider to determine the underlying cause.
[Read more about bladder cancer symptoms.]
Types of Bladder Cancer
Bladder cancer is classified based on how far it has spread:
- Non-Muscle-Invasive Bladder Cancer (NMIBC): This is the most common type, where cancerous cells remain within the bladder’s lining. It accounts for roughly 70% of all cases. Most patients with NMIBC have a good prognosis and do not face life-threatening complications.
- Muscle-Invasive Bladder Cancer (MIBC): When cancer spreads into the surrounding bladder muscles, it is considered muscle-invasive. While less common, it carries a higher risk of spreading to other parts of the body and may be more challenging to treat.
- Locally Advanced or Metastatic Bladder Cancer: If cancer cells spread to other parts of the body, the condition is referred to as locally advanced or metastatic bladder cancer.
[Learn more about bladder cancer diagnosis.]
Causes of Bladder Cancer
Most bladder cancer cases are linked to prolonged exposure to harmful substances. Over time, these substances can lead to abnormal changes in bladder cells. Key risk factors include:
- Smoking: Tobacco smoke is the leading cause, responsible for around half of all bladder cancer cases.
- Chemical Exposure: Contact with certain chemicals, historically used in manufacturing, can elevate the risk of bladder cancer. Fortunately, many of these substances have since been banned.
[Explore the causes and prevention of bladder cancer.]
Treatment Options for Bladder Cancer
Treatment varies based on the cancer type and stage:
- Non-Muscle-Invasive Bladder Cancer: Typically treated by removing cancerous cells through a procedure called transurethral resection of a bladder tumor (TURBT). Chemotherapy medication is often administered directly into the bladder afterward to prevent recurrence. High-risk cases may also require Bacillus Calmette-Guérin (BCG) therapy.
- Muscle-Invasive Bladder Cancer: Treatment may involve a cystectomy (surgical removal of the bladder). Following a cystectomy, alternative methods for collecting urine, such as an external bag or a reconstructed bladder from a section of the bowel, are provided.
- Radiotherapy and Chemotherapy: If bladder removal is not feasible or preferred, a combination of radiotherapy and chemotherapy may be recommended. In some instances, chemotherapy may be used alone before surgery or combined with radiotherapy.
Follow-Up Care
Regular follow-up tests are crucial after treatment to monitor for any signs of recurrence.
[Read more about bladder cancer treatments.]
Who is at Risk?
Bladder cancer predominantly affects older adults, with over half of all new cases diagnosed in individuals aged 75 and older. Men are statistically more prone to bladder cancer compared to women, potentially due to higher smoking rates and greater historical exposure to manufacturing-related chemicals.
Symptoms of Bladder Cancer
The most common symptom of bladder cancer is blood in the urine, a condition known medically as haematuria. While it is usually painless, you may notice streaks of blood or a change in your urine color to brown. Sometimes, blood in the urine may not be visibly noticeable and can appear intermittently.
Additional Symptoms of Bladder Cancer
Apart from blood in the urine, bladder cancer may present with other, less common symptoms, such as:
- Frequent urination: An increased need to urinate more often than usual.
- Sudden urges to urinate: Feeling an immediate need to pass urine.
- Burning sensation during urination: Experiencing discomfort or pain when passing urine.
Advanced Stage Symptoms
If bladder cancer progresses to an advanced stage and spreads to other parts of the body, symptoms may include:
- Pelvic pain
- Bone pain
- Unintentional weight loss
- Swelling of the legs
When to Seek Medical Advice
If you notice blood in your urine, even if it comes and goes, it is important to consult with your GP for an evaluation. While blood in the urine may be alarming, it does not always indicate bladder cancer. There are other, more common causes, including:
- Urinary tract infections (UTIs), such as cystitis
- Kidney infections
- Kidney stones
- Urethritis (inflammation of the urethra)
- Enlarged prostate gland (in men)
Early detection and prompt medical attention can lead to a better prognosis, so always take symptoms seriously.
Causes and Risk Factors of Bladder Cancer
Bladder cancer arises when changes occur in the cells of the bladder, often due to exposure to certain chemicals. However, in many cases, the exact cause remains unclear.
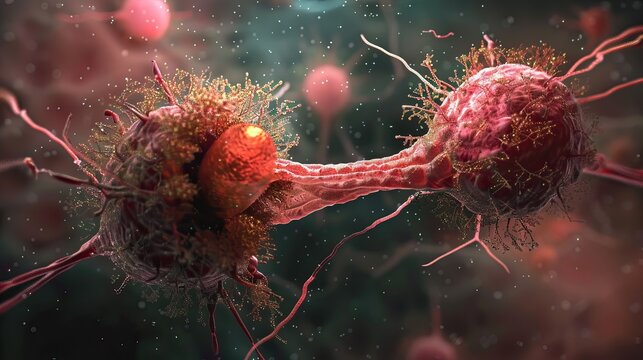
What is Cancer?
Cancer begins with a change, or mutation, in the DNA structure of cells. This mutation affects how cells grow and divide, leading to uncontrolled cell reproduction and the formation of a mass called a tumor.
Key Risk Factors for Bladder Cancer
1. Smoking
Smoking is the leading risk factor for bladder cancer. Tobacco contains carcinogenic (cancer-causing) chemicals, which, when inhaled, enter the bloodstream and are filtered through the kidneys into the urine. This process exposes the bladder lining to these harmful chemicals repeatedly, increasing the likelihood of mutations and cancer development.
- It is estimated that smoking accounts for over one-third of all bladder cancer cases.
- Smokers may be up to four times more likely to develop bladder cancer compared to non-smokers.
2. Chemical Exposure
Exposure to certain industrial chemicals is another major risk factor, contributing to around 25% of bladder cancer cases. Occupational exposure to the following chemicals increases risk:
- Aniline dyes
- 2-Naphthylamine
- 4-Aminobiphenyl
- Xenylamine
- Benzidine
- O-Toluidine
Jobs involving dyes, textiles, rubber, paint, plastic manufacturing, and leather tanning carry a higher risk due to chemical exposure. Non-manufacturing jobs, such as taxi and bus drivers exposed to diesel fumes, may also be at risk.
This occupational link was first identified in the 1950s and 1960s. While regulations have since become more stringent, bladder cancer cases may still emerge years later, as it can take decades for symptoms to appear.
3. Additional Risk Factors
Other factors that may increase bladder cancer risk include:
- Previous Radiation Therapy: Radiotherapy for cancers near the bladder, such as bowel cancer, can increase the risk.
- Certain Chemotherapy Medications: Treatments such as cyclophosphamide and cisplatin have been linked to bladder cancer.
- Previous Prostate Surgery: Partial prostate removal for benign enlargement may elevate risk.
- Diabetes: Certain medications used for type 2 diabetes have been associated with bladder cancer.
- Indwelling Catheters: Long-term use of bladder catheters, especially when used due to nerve-related paralysis, can be a risk factor.
- Chronic Urinary Tract Infections (UTIs) and Bladder Stones: Prolonged or repeated infections may contribute to risk.
- Early Menopause: Women who experience menopause before age 42 may be at a higher risk.
- Schistosomiasis: This infection, caused by a freshwater parasite, is a rare risk factor in some regions.
How Does Bladder Cancer Spread?
Bladder cancer typically originates in the cells lining the bladder. In some cases, it may spread into the surrounding bladder muscle and beyond through the lymphatic system. If the cancer extends to other parts of the body, such as organs, it is classified as metastatic bladder cancer.
Diagnosing Bladder Cancer: Tests, Procedures, and What to Expect
If you experience symptoms of bladder cancer, such as blood in your urine (haematuria), it is important to speak with your GP. Your doctor may ask about your symptoms, family history, and any exposure to potential bladder cancer risk factors, such as smoking.
Initial Diagnosis by Your GP
- Urine Tests: Your GP may request a urine sample to test for traces of blood, bacteria, or abnormal cells.
- Physical Examination: Your doctor may perform a physical examination of the rectum and vagina to check for any noticeable lumps caused by bladder cancer.
If bladder cancer is suspected, you will be referred to a hospital for further testing.
Hospital Tests and Procedures
Specialist Clinics
Some hospitals offer dedicated clinics for patients with haematuria, while others have specialized urology departments for diagnosing urinary tract issues.
Cystoscopy
A cystoscopy is often the first procedure recommended for diagnosing bladder cancer. It involves using a thin tube with a camera and light, called a cystoscope, which is passed through the urethra to examine the inside of the bladder. A local anaesthetic gel is applied to the urethra for comfort, and the procedure typically takes about 5 minutes.
Imaging Scans
- CT or MRI Scans: These scans provide detailed images of the bladder and may be recommended if further assessment is needed.
- Intravenous Urogram (IVU): This test involves injecting dye into the bloodstream, followed by X-rays to trace the dye through the urinary system, providing a comprehensive view.
Transurethral Resection of a Bladder Tumour (TURBT)
If any abnormalities are found during the cystoscopy, a TURBT operation may be conducted to remove and analyze tissue samples for cancer. This procedure is done under general anaesthetic. In some cases, a second operation may be required within six weeks to check if cancer has spread to the bladder muscle. Following TURBT, a dose of chemotherapy may be offered to reduce the risk of recurrence.
[Read more about the TURBT procedure and bladder cancer treatment.]
Staging and Grading of Bladder Cancer
After testing, your healthcare team will determine the stage and grade of your cancer.
Staging
Staging assesses how far the cancer has spread, with lower-stage cancers being smaller and more treatable:
- T Stages:
- TIS or CIS (Carcinoma in Situ): A very early high-grade cancer confined to the innermost bladder lining.
- Ta: Cancer limited to the innermost layer of the bladder lining.
- T1: Cancer cells have grown into the connective tissue beyond the bladder lining.
- T2: Cancer has grown into the bladder muscle.
- T3: Cancer has spread through the bladder muscle into surrounding fat.
- T4: Advanced cancer that has spread outside the bladder to nearby organs.
N Stages (Lymph Node Involvement)
- N0: No cancerous cells in lymph nodes.
- N1: Cancerous cells in one pelvic lymph node.
- N2: Cancerous cells in two or more pelvic lymph nodes.
- N3: Cancerous cells in lymph nodes deep in the groin (common iliac nodes).
M Stages (Metastasis)
- M0: Cancer has not spread to other parts of the body.
- M1: Cancer has spread to other parts of the body (e.g., bones, lungs, or liver).
The TNM system may seem complex, so don’t hesitate to ask your healthcare team questions about your results and how they impact your treatment plan and prognosis.
Treating Bladder Cancer: Options, Procedures, and What to Expect
The treatment for bladder cancer depends largely on its stage and whether it is non-muscle-invasive or muscle-invasive. Treatment decisions are guided by a multidisciplinary team (MDT) of specialists, including urologists, oncologists, pathologists, and radiologists.
Multidisciplinary Teams (MDTs)
Your MDT works together to determine the best treatment plan. Team members include:
- Urologist: A surgeon specializing in urinary tract conditions.
- Clinical Oncologist: A chemotherapy and radiotherapy specialist.
- Pathologist: An expert in diseased tissue.
- Radiologist: A specialist in imaging techniques.
You will also have a clinical nurse specialist as your main point of contact, who can address your questions and offer support throughout your treatment journey.
Non-Muscle-Invasive Bladder Cancer Treatment
For non-muscle-invasive bladder cancer (stages CIS, Ta, T1), treatment depends on the risk of recurrence or progression. Factors include the number of tumors, their size, and whether you have had bladder cancer before.
Low-Risk Cases
- TURBT Procedure: Transurethral resection of a bladder tumor (TURBT) removes tumors using a cystoscope. After surgery, a single dose of chemotherapy may be delivered directly into the bladder to reduce recurrence risk.
- Follow-Up: Follow-up cystoscopy appointments are scheduled at 3 and 9 months to monitor for recurrence.
Intermediate-Risk Cases
- Chemotherapy: A course of six doses of chemotherapy delivered directly into the bladder is typically recommended.
- Follow-Up: Cystoscopy follow-ups occur at 3, 9, 18 months, and then yearly to monitor recurrence.
High-Risk Cases
- Second TURBT: A follow-up TURBT may be performed within six weeks of the first.
- BCG Treatment or Cystectomy: Treatment may involve Bacillus Calmette-Guérin (BCG) therapy or bladder removal (cystectomy).
Muscle-Invasive Bladder Cancer Treatment
For muscle-invasive bladder cancer (stages T2 and T3), treatment aims to cure or control the disease:
- Cystectomy: Complete removal of the bladder.
- Radiotherapy with a Radiosensitiser: Enhances the effect of radiotherapy on cancer cells.
Radiotherapy Considerations
- Side Effects: Diarrhea, bladder inflammation, erectile dysfunction, vaginal tightening, infertility, and fatigue are possible side effects. Most subside after treatment ends.
- Follow-Up: Regular follow-up appointments with cystoscopy and periodic CT scans.
Chemotherapy Options
- Intravenous Chemotherapy: Administered through a vein, used before surgery or radiotherapy to shrink tumors, or as a standalone treatment for advanced cancer.
- Side Effects: Nausea, vomiting, hair loss, immune suppression, and increased infection risk.
Locally Advanced or Metastatic Bladder Cancer
Treatment focuses on symptom relief and may include:
- Chemotherapy: To manage cancer spread.
- Radiotherapy and Other Symptom-Relief Treatments: To address pain and urinary issues.
Palliative Care
If the cancer is incurable, palliative care focuses on comfort and symptom management.
Complications of Bladder Cancer: Emotional and Physical Challenges
A diagnosis of bladder cancer and its treatments can bring significant changes to your life, affecting both your emotional and physical well-being. Understanding the potential complications can help you prepare and seek appropriate support.
Emotional Impact of Bladder Cancer
Living with bladder cancer often triggers a range of emotions, described by many as a “rollercoaster” of feelings. It’s common to feel a mix of hope and despair, from the initial diagnosis to the after-effects of treatment.
Recognizing Signs of Depression
Bladder cancer can lead to depression, characterized by:
- Continuous feelings of sadness or hopelessness
- Loss of interest in activities you once enjoyed
If you suspect you are experiencing depression, consult your GP. Treatment options may include antidepressants or cognitive behavioural therapy (CBT).
[Read more about coping with cancer.]
Urinary Diversion After Bladder Removal
If your bladder is surgically removed, a urinary diversion procedure will create an alternative way to pass urine. There are different types of urinary diversion:
1. Urostomy
- A urostomy involves creating a stoma (opening) on the abdomen using a small section of the bowel. A stoma bag collects urine, and a specialized nurse will teach you how to care for it.
2. Continent Urinary Diversion
- Similar to a urostomy, but without an external bag. A pouch inside the body stores urine, which is emptied using a catheter through an opening with a valve to prevent leaks.
3. Bladder Reconstruction (Neobladder)
- In some cases, a neobladder (a new bladder made from bowel tissue) can be created. It connects to the urethra, allowing for urination. However, this method requires learning to empty the neobladder through muscle control, and it may lead to incontinence, especially at night.
Sexual Complications from Bladder Cancer Treatment
Erectile Dysfunction
Erectile dysfunction is a possible side effect after a radical cystectomy. Treatment options include:
- Phosphodiesterase type 5 inhibitors (PDE5): These medications increase blood flow to the penis.
- Vacuum Pump Therapy: This device helps create and maintain an erection by drawing blood into the penis.
[Read more about treating erectile dysfunction.]
Narrowing of the Vagina
Radiotherapy and cystectomy may lead to vaginal shortening and narrowing, causing painful or difficult intercourse. Treatment options include:
- Hormonal Creams: To increase vaginal moisture.
- Vaginal Dilators: Cone-shaped devices used to gently stretch the vagina over time.
Open conversations with your specialist cancer nurse can provide additional support and guidance on using these treatments.
Preventing Bladder Cancer: Reducing Your Risk
While it may not always be possible to fully prevent bladder cancer, certain risk factors have been identified that can increase your risk of developing the condition. Here are some actionable steps to lower your risk.
Quit Smoking
Smoking is a major risk factor for bladder cancer. Quitting smoking is one of the most effective ways to reduce your risk of developing or experiencing a recurrence of bladder cancer.
- Get Support: Consider contacting services like Quit Your Way Scotland (0800 84 84 84) for free expert advice and encouragement.
- Medical Assistance: Your GP can prescribe treatments to manage withdrawal symptoms if you prefer not to be referred to a smoking cessation service.
For more resources and tips, explore stop smoking treatments and related support pages.
Workplace Safety Measures
Certain jobs, particularly those in manufacturing industries, may increase the risk of bladder cancer due to chemical exposure. At-risk occupations include work with:
- Rubber
- Dyes
- Textiles
- Plastic
- Leather Tanning
- Diesel Fumes
Rigorous safety protocols have been established to minimize exposure to these chemicals. If you are uncertain about workplace safety procedures, talk to your line manager or health and safety representative. If you suspect that safety recommendations are being ignored, contact the Health and Safety Executive for guidance.
Dietary Considerations
A diet rich in fruits and vegetables and low in fat may help reduce the risk of bladder cancer. Although the evidence is limited, adopting this type of healthy eating pattern offers numerous health benefits, including reducing the risk of other cancers, high blood pressure, stroke, and heart disease.
Tips for a Healthy Diet:
- High-Fibre, Low-Fat Diet: Focus on whole grains, fresh fruits, and vegetables (aim for at least five portions per day).
- Limit Salt Intake: Try to consume no more than 6g (0.2oz) of salt per day (about one teaspoon) to help maintain healthy blood pressure levels.
- Avoid Saturated Fat: Reduce consumption of foods high in saturated fat, such as:
- Meat pies and sausages
- Fatty cuts of meat
- Butter and lard
- Cream and hard cheese
- Cakes, biscuits, and foods containing coconut or palm oil
Include Unsaturated Fats
A balanced diet should contain some unsaturated fats to help control cholesterol. Foods high in unsaturated fats include:
- Oily fish
- Avocados
- Nuts and seeds
- Sunflower, rapeseed, olive, and vegetable oils