Benign prostate enlargement
Benign prostate enlargement (BPE), also known as benign prostatic hyperplasia (BPH), is a non-cancerous enlargement of the prostate gland that commonly affects older men and individuals with a prostate. While it can lead to bothersome urinary symptoms, it is generally not considered a serious threat to health and is not linked to an increased risk of prostate cancer.
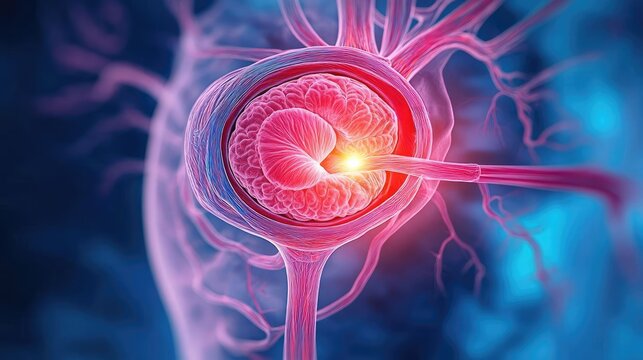
Understanding the Prostate Gland
The prostate is a small, walnut-sized gland located between the bladder and the penis. It surrounds the urethra, the tube through which urine passes. The prostate plays a key role in the male reproductive system by producing a thick, white fluid that becomes a component of semen. This fluid is converted into a thinner liquid by a protein called prostate-specific antigen (PSA), which mixes with sperm from the testicles to create semen.
Symptoms of Benign Prostate Enlargement
As the prostate enlarges, it can exert pressure on the bladder and urethra, leading to various urinary symptoms. These symptoms can vary in severity and include:
- Difficulty starting urination: Experiencing a delay or difficulty in beginning to urinate.
- Frequent need to urinate: Needing to urinate more often, especially at night (nocturia).
- Difficulty fully emptying the bladder: Feeling that the bladder is not completely empty after urination.
- Weak urine flow: A decrease in the force of the urine stream.
- Dribbling of urine: Leakage or dribbling after finishing urination.
- Urgency to urinate: A sudden, strong need to urinate.
For some individuals, these symptoms are mild and manageable, while for others, they can significantly impact quality of life.
Causes of Benign Prostate Enlargement
The exact cause of benign prostate enlargement is not fully understood, but it is believed to be related to hormonal changes as a person ages. Specifically, changes in the levels of male hormones, such as dihydrotestosterone (DHT), may contribute to the enlargement of the prostate.
Diagnosing Benign Prostate Enlargement
Diagnosis typically begins with a visit to your GP, who will evaluate your symptoms and medical history. You may be asked to complete a questionnaire that scores the severity of your symptoms. Additional diagnostic tests may include:
- Urine tests: To check for signs of infection or other conditions.
- Blood tests: To measure prostate-specific antigen (PSA) levels, which can help rule out prostate cancer and assess prostate health.
- Digital rectal examination (DRE): A physical exam to assess the size and condition of the prostate.
- Ultrasound: In some cases, an ultrasound scan of the prostate and bladder may be performed.
Treatment Options for Benign Prostate Enlargement
The treatment approach depends on the severity of symptoms. Options include:
1. Lifestyle Changes
For mild to moderate symptoms, lifestyle adjustments may be recommended, such as:
- Reducing intake of caffeine and alcohol, which can irritate the bladder.
- Regular exercise to promote overall health.
- Avoiding drinking fluids before bedtime to reduce nighttime urination.
2. Medications
- Alpha-blockers: Medications like tamsulosin and alfuzosin relax the muscles in the prostate and bladder neck, making it easier to urinate.
- 5-alpha reductase inhibitors: Drugs such as finasteride and dutasteride reduce the size of the prostate by blocking the effects of DHT.
3. Surgery
Surgical intervention is considered for moderate to severe symptoms that do not respond to medication. Surgical options include:
- Transurethral resection of the prostate (TURP): The most common procedure, involving the removal of part of the prostate to relieve pressure on the urethra.
- Laser therapy: Uses focused light to remove or shrink prostate tissue.
- Prostatic urethral lift (PUL): A minimally invasive procedure that lifts and holds the enlarged prostate tissue away from the urethra.
Potential Complications of Benign Prostate Enlargement
In some cases, untreated benign prostate enlargement can lead to complications, such as:
- Urinary tract infections (UTIs): Caused by incomplete emptying of the bladder, leading to bacterial growth.
- Acute urinary retention: Sudden inability to urinate, which can be painful and may require emergency treatment.
- Bladder stones: Formed as a result of stagnant urine in the bladder.
- Bladder damage: Due to chronic urinary retention and pressure.
- Kidney damage: In rare cases, backflow of urine can lead to kidney damage.
Prevalence of Benign Prostate Enlargement
Benign prostate enlargement is common in men and individuals with a prostate as they age, with symptoms typically appearing after the age of 50. It is estimated that more than half of men over 50 experience some symptoms of BPH, and the prevalence increases with age.
Managing and Living with Benign Prostate Enlargement
Managing benign prostate enlargement involves regular monitoring, lifestyle modifications, and adherence to prescribed treatments. Individuals are encouraged to maintain regular follow-up appointments with their healthcare provider to ensure their condition is managed effectively and to address any new or worsening symptoms.
By understanding and managing the symptoms of benign prostate enlargement, many individuals can maintain a good quality of life and reduce the impact of the condition on daily activities. If you experience any concerning symptoms, it is important to seek medical advice promptly.
Symptoms of benign prostate enlargement
Benign prostate enlargement (BPE), also known as benign prostatic hyperplasia (BPH), can lead to various urinary symptoms as the enlarged prostate puts pressure on the bladder and urethra. These symptoms can range from mild to severe and significantly impact daily life.
Common Symptoms of Benign Prostate Enlargement
Difficulty Starting Urination:
- A delay or hesitancy in beginning the flow of urine.
- Straining to initiate urination.
Weak Urine Flow:
- A decrease in the force of the urine stream.
- ‘Stop-start’ urination, where the flow may be interrupted.
Frequent Urination:
- The need to urinate more often, particularly during the night (nocturia).
Sudden Urgency to Urinate:
- A sudden, strong urge to urinate, which can sometimes lead to involuntary leakage of urine (urinary incontinence) if you cannot reach a toilet in time.
Incomplete Emptying of the Bladder:
- Feeling like the bladder is not completely emptied after urination.
- Dribbling or leaking urine even after finishing.
Blood in the Urine (Haematuria):
- In some cases, BPE may cause blood to appear in the urine, which requires prompt medical attention.
Potential Complications of Advanced Benign Prostate Enlargement
In more severe cases, untreated BPE may lead to complications such as:
- Urine Retention: Inability to completely or partially empty the bladder, which may require medical intervention to relieve.
- Bladder Stones: Resulting from residual urine in the bladder, these can cause pain, infection, and further urinary problems.
- Bladder Infections: Frequent or chronic infections due to incomplete emptying of the bladder.
- Kidney Damage: Increased pressure in the bladder due to urine retention can lead to kidney damage over time if not properly managed.
When to Seek Medical Advice
- Changes in Urination: If you experience any changes in your usual urinary patterns or have difficulty urinating, it is important to consult a GP.
- Blood in Urine: Even if symptoms are mild, the presence of blood in the urine requires immediate medical attention to rule out serious conditions.
- Worsening Symptoms: If you find your symptoms worsening or interfering with your daily life, a healthcare provider can offer options for management and treatment.
Importance of Early Intervention
Early diagnosis and management of benign prostate enlargement can help prevent complications and improve quality of life. Treatment options range from lifestyle adjustments and medications to surgical procedures, depending on the severity of symptoms and their impact on daily activities. Regular follow-ups with a healthcare provider are essential to monitor the condition and adjust treatment as necessary.
Causes of benign prostate enlargement
Benign prostate enlargement (BPE), or benign prostatic hyperplasia (BPH), is a common condition affecting older individuals with a prostate. Although the exact cause remains unclear, several factors, primarily hormonal changes, have been identified as likely contributors to the development of the condition.
Hormonal Factors Involved in Benign Prostate Enlargement
Dihydrotestosterone (DHT) Theory:
- DHT is a hormone derived from testosterone and plays a role in prostate development and growth. Research suggests that as men age, levels of DHT increase within the prostate tissue, which may trigger the enlargement of the prostate. High levels of DHT are thought to continue stimulating the growth of prostate cells, contributing to the condition.
Testosterone and Oestrogen Balance:
- Typically, younger men produce higher levels of testosterone compared to oestrogen. As men age, testosterone levels naturally decline, leading to a relatively higher proportion of oestrogen in the body.
- It is hypothesized that the relative increase in oestrogen may promote prostate cell growth and contribute to benign prostate enlargement.
Risk Factors for Benign Prostate Enlargement
Age:
- Age is the most significant risk factor. Benign prostate enlargement is rare in men under 40 but becomes increasingly common with age, particularly in those over 50 years old.
Hormonal Imbalance:
- As mentioned, the hormonal shifts in testosterone and oestrogen levels may play a role in the condition’s development as individuals age.
Genetics:
- A family history of prostate issues may increase the likelihood of developing benign prostate enlargement, suggesting a genetic component.
Lifestyle Factors:
- While lifestyle factors alone are not definitive causes, they can contribute to the risk. For instance, obesity and a sedentary lifestyle may indirectly influence hormone levels and prostate health.
Medical Conditions:
- Some studies have linked benign prostate enlargement to conditions such as:
- High Blood Pressure (Hypertension): The condition has been associated with higher rates of BPE, although it may also be linked to the aging process.
- Diabetes: Research shows a correlation between diabetes and an increased risk of BPE. However, it is unclear whether diabetes directly influences prostate growth or if it is a result of the common aging process shared by both conditions.
- Some studies have linked benign prostate enlargement to conditions such as:
Other Considerations
- Diet and Lifestyle: Although no specific foods or lifestyle habits have been conclusively shown to cause BPE, some evidence suggests that maintaining a balanced diet and regular exercise may support prostate health.
- Inflammation: Chronic inflammation of the prostate may contribute to its enlargement, although the exact role of inflammation in BPE remains under investigation.
Importance of Monitoring Hormonal Health
Understanding the hormonal factors and risk factors associated with benign prostate enlargement is crucial. While the condition is generally not life-threatening, managing symptoms and monitoring prostate health can significantly improve the quality of life. Regular check-ups with healthcare professionals can help in early detection and appropriate management of prostate-related concerns.
Diagnosing benign prostate enlargement
To diagnose benign prostate enlargement (BPE) or benign prostatic hyperplasia (BPH), a series of tests and assessments are used by healthcare professionals to evaluate symptoms, rule out other conditions, and determine the severity of the enlargement. Here is a detailed explanation of the diagnostic process:
1. Initial Assessment by a General Practitioner (GP)
Symptom Inquiry: Your GP will begin by asking questions about your symptoms, such as how often you urinate, if you experience difficulty starting urination, or if you have a weak urine stream.
International Prostate Symptom Score (IPSS): You may be asked to complete a questionnaire to assess the severity of your symptoms. Each question in the IPSS carries a score, and the total score helps determine whether your symptoms are mild, moderate, or severe.
Questions in the IPSS include:
- Sensation of not completely emptying your bladder
- Frequency of needing to urinate soon after a previous urination
- Intermittent urination or stopping and starting
- Difficulty delaying urination
- Weak urine stream
- Straining to start urinating
- Frequency of getting up during the night to urinate
2. Ruling Out Other Conditions
The symptoms of benign prostate enlargement can be similar to those caused by other conditions, such as prostate cancer. Therefore, your GP may perform additional tests to rule out other causes.
- Urine Tests: These can identify infections in the urinary system, such as bladder or kidney infections, which can cause symptoms similar to BPE.
- Rectal Examination: Your GP may perform a rectal examination to check the prostate gland for abnormalities, such as hard or bumpy areas that may indicate prostate cancer. This involves the GP inserting a lubricated, gloved finger into the rectum to feel the prostate.
- Prostate-Specific Antigen (PSA) Test: A blood test measures the amount of PSA protein produced by the prostate. Elevated PSA levels may suggest prostate enlargement or, in some cases, prostate cancer, but it is not definitive.
3. Specialized Tests by a Urologist
If necessary, you may be referred to a urologist for more specialized testing.
- Transrectal Ultrasound (TRUS): An ultrasound probe inserted into the rectum uses sound waves to create detailed images of the prostate and surrounding tissues, helping measure prostate size and check for cancer.
- CT Urogram: This imaging test uses a special dye injected into the bloodstream to help visualize the urinary tract (bladder, ureters, and urethra). It can detect blockages, such as kidney or bladder stones, that could be causing urinary symptoms.
- Voiding Charts: You may be asked to keep a diary of your urination patterns, including frequency, volume, and any difficulties during urination.
- Uroflowmetry: This test measures how quickly and effectively urine flows from the bladder. It involves the insertion of a small tube (catheter) into the bladder to monitor bladder pressure while it fills and empties.
- Bladder Pressure Testing: A catheter may be used to fill the bladder with water while pressure sensors measure the response of the bladder muscles.
4. Diagnostic Outcomes
After these tests, your GP or urologist will analyze the results to confirm whether you have benign prostate enlargement and determine its severity. This helps guide the appropriate treatment plan, whether it involves lifestyle changes, medication, or, in some cases, surgery.
This comprehensive approach ensures that benign prostate enlargement is accurately diagnosed and effectively managed while ruling out other potential causes of similar symptoms.
Treating benign prostate enlargement
Treating benign prostate enlargement (BPE), or benign prostatic hyperplasia (BPH), focuses on relieving symptoms and managing complications caused by the enlarged prostate. Treatment depends on the severity of symptoms and how they impact daily life. Here are the primary treatment options in detail:
1. Lifestyle Changes
- Monitor Fluid Intake: Avoid drinking liquids, particularly those with caffeine and alcohol, a few hours before bedtime to reduce nighttime urination (nocturia).
- Timed Medication: Adjusting the time when you take any prescribed medications can also help, particularly if nocturia is a problem.
- Limit Caffeine and Alcohol: These substances can irritate the bladder, worsening symptoms.
- Regular Exercise: Moderate exercise, like walking for 30–60 minutes per day, has been shown to improve symptoms of BPE.
- Bladder Training: Techniques to improve bladder control, such as delaying urination for longer periods, can help increase bladder capacity. This should be done under medical guidance.
2. Bladder Training
- Bladder Diary: Keeping track of urination frequency and volume can help identify patterns.
- Pelvic Floor Exercises: These can strengthen the pelvic muscles and improve bladder control.
3. Medications
- 5-Alpha Reductase Inhibitors (Finasteride, Dutasteride):
- Function: These medications reduce the size of the prostate by blocking the hormone dihydrotestosterone (DHT).
- Onset of Effects: Improvement is gradual, and it may take six months or more to see maximum benefits.
- Side Effects: These may include reduced libido, erectile dysfunction, and reduced sperm count. Men taking these medications should use condoms, as they may have adverse effects on sperm.
- Alpha Blockers (Tamsulosin, Alfuzosin):
- Function: Relax the muscles in the bladder and prostate, making it easier to urinate.
- Immediate Effects: Provide faster symptom relief than 5-alpha reductase inhibitors.
- Side Effects: Potential dizziness, headaches, or low blood pressure, particularly when starting the medication.
- Combination Therapy: In some cases, both alpha blockers and 5-alpha reductase inhibitors may be used together to provide better symptom control.
4. Surgery
Surgery is generally recommended for moderate to severe symptoms that have not improved with medication or are causing significant issues such as urinary retention.
- Transurethral Resection of the Prostate (TURP):
- Procedure: A resectoscope is inserted through the urethra to remove parts of the prostate using an electric loop.
- Recovery: Most patients leave the hospital after 2–3 days.
- Complications: Retrograde ejaculation (semen flows into the bladder instead of out of the penis) is a common side effect.
- Bladder Neck Incision (TUIP):
- Procedure: Small cuts are made at the bladder neck and prostate to widen the urethra, improving urine flow.
- Less Risk: TUIP has a lower risk of retrograde ejaculation than TURP.
- Holmium Laser Enucleation of the Prostate (HoLEP):
- Procedure: Excess tissue is removed using a laser.
- Advantages: Similar benefits as TURP with potentially fewer complications.
- Insertion of Prostatic Urethral Lift Implants:
- Procedure: Small implants are placed to hold the prostate away from the urethra.
- Benefits: Less impact on sexual function compared to TURP or TUIP.
- Greenlight Laser Surgery (Photoselective Vaporization):
- Procedure: A laser is used to destroy excess prostate tissue.
- Benefits: Shorter hospital stay and quicker recovery compared to TURP.
- Open Prostatectomy:
- Procedure: Involves making an incision in the abdomen to remove part of the prostate. Rarely used today due to the development of minimally invasive options.
- Risks: Higher risk of complications, such as erectile dysfunction and incontinence.
5. Minimally Invasive Procedures
- Transurethral Vaporization of the Prostate (TUVP): This is similar to TURP but uses heat to vaporize prostate tissue instead of removing it.
- Prostatic Artery Embolization: This is an emerging, minimally invasive option that shrinks the prostate by blocking its blood supply.
6. Managing Complications
- Urinary Tract Infections (UTIs): If BPE causes recurrent UTIs, antibiotics or more invasive management may be recommended.
- Urinary Retention: Catheterization may be necessary for short-term relief.
Note: Regular follow-up with your healthcare provider is essential to monitor symptoms and make adjustments to the treatment plan as needed. Discussing potential side effects and risks of each treatment option is crucial for making an informed decision tailored to your specific needs and health status.
Complications of benign prostate enlargement
Benign prostate enlargement (BPE), or benign prostatic hyperplasia (BPH), can lead to various complications if left untreated. Here is a detailed overview of these complications and their associated symptoms and treatments:
1. Urinary Tract Infections (UTIs)
- Cause: When the enlarged prostate prevents the bladder from emptying fully, bacteria may remain in the urinary system and multiply, leading to an infection.
- Symptoms:
- Cloudy, bloody, or foul-smelling urine
- Pain or discomfort in the lower abdomen (tummy area)
- Nausea and vomiting
- Chills and shaking (rigors)
- A high temperature of 38°C (100.4°F) or higher
- Treatment:
- Antibiotics: UTIs are treated with antibiotics to clear the infection.
- Long-term Management: If you experience repeated UTIs, your healthcare provider may consider surgical intervention to relieve the obstruction caused by the enlarged prostate.
- Complications:
- Kidney Damage: If left untreated, repeated UTIs can lead to kidney infections and possible kidney damage.
- Bladder Damage: Chronic infections can damage the bladder’s ability to contract and empty properly.
2. Acute Urinary Retention (AUR)
- Description: AUR is a sudden and complete inability to pass urine, which can be extremely painful and requires immediate medical attention.
- Symptoms:
- Sudden inability to urinate despite the urge to do so
- Severe pain or pressure in the lower abdomen
- Swelling or distension of the bladder, which can sometimes be felt as a firm lump in the lower abdomen
- Emergency Response:
- Seek Immediate Help: AUR is a medical emergency. Call 999 (or your local emergency number) and request an ambulance if you or someone else has these symptoms.
- Treatment:
- Catheterization: A thin, flexible tube called a catheter is inserted through the urethra into the bladder to drain the urine. This provides immediate relief from the painful symptoms of retention.
- Surgery: In severe cases, surgical intervention may be necessary to remove excess prostate tissue and prevent future episodes of urinary retention.
- Complications of AUR:
- Kidney Damage: If urine backs up into the kidneys due to untreated urinary retention, it can cause serious kidney damage.
- Bladder Damage: Prolonged retention can weaken the bladder muscles and reduce their ability to contract and empty normally, leading to chronic urinary retention.
3. Bladder Stones
- Cause: Incomplete emptying of the bladder can lead to the formation of bladder stones, as minerals in the urine crystallize.
- Symptoms:
- Painful urination
- Blood in the urine
- Difficulty starting urination
- Frequent urination, especially at night
- Intermittent urine stream or sudden stopping of the urine stream
- Treatment:
- Removal: Bladder stones may need to be removed through a surgical procedure, such as cystolitholapaxy, where the stones are broken up and removed through the urethra.
- Prevention: Treating the underlying cause, such as the enlarged prostate, can help prevent future stone formation.
4. Chronic Urinary Retention
- Description: Unlike acute urinary retention, chronic retention develops slowly over time, leading to incomplete emptying of the bladder and potential complications.
- Symptoms:
- Weak urine stream
- Dribbling after urination
- A feeling that the bladder is never completely empty
- Frequent urinary tract infections
- Treatment:
- Catheterization: In some cases, a long-term catheter may be needed to help empty the bladder.
- Surgery: Procedures to reduce the size of the prostate may be recommended to improve urine flow and relieve retention.
5. Bladder Damage
- Cause: Long-term pressure from an enlarged prostate can weaken the bladder wall and affect its ability to contract and empty fully.
- Symptoms:
- Difficulty starting urination
- Inability to fully empty the bladder
- Treatment: Addressing the underlying cause, such as reducing prostate size, may help prevent further damage.
6. Kidney Damage
- Cause: Chronic or severe urinary retention can cause urine to back up into the kidneys, potentially leading to hydronephrosis (swelling of the kidneys) and impaired kidney function.
- Symptoms:
- General symptoms of kidney dysfunction, such as fatigue, swelling in the ankles, or changes in urination frequency
- Treatment: Immediate relief of urinary retention and addressing the underlying prostate condition are crucial to prevent irreversible kidney damage.
Prevention and Monitoring
- Regular Check-ups: Men with an enlarged prostate should have regular follow-ups to monitor symptoms and detect any complications early.
- Lifestyle Changes: Staying hydrated, reducing caffeine and alcohol intake, and maintaining a healthy weight may help manage symptoms and prevent complications.
If you have any symptoms of benign prostate enlargement, speak with your healthcare provider for a comprehensive evaluation and appropriate management plan to avoid potential complications.