Bacterial vaginosis
Bacterial vaginosis (BV) is a common condition that occurs when the natural balance of bacteria in the vagina becomes disrupted, leading to an overgrowth of certain bacteria. While it is not classified as a sexually transmitted infection (STI), it is more likely to occur in sexually active individuals and can cause bothersome symptoms.
Symptoms of Bacterial Vaginosis
Many women with BV may not experience any noticeable symptoms. When symptoms do occur, they can include:
- Abnormal Vaginal Discharge: The discharge associated with BV is often white or gray in color and may have a thin, watery consistency.
- Fishy Odor: One of the hallmark signs of BV is a strong, fishy odor that may become more pronounced after sexual intercourse or during menstruation.
- Lack of Irritation: Unlike yeast infections, BV typically does not cause itching, burning, or inflammation around the vulva or vagina.
What to Do If You Suspect Bacterial Vaginosis
If you think you may have BV, there are several steps you can take:
- Consider Possible Triggers: Certain habits or products may disrupt the natural balance of bacteria in the vagina. These include:
- Using scented soaps, bubble baths, or vaginal sprays
- Douching or using vaginal washes
- Using strong detergents to wash underwear
- Try Over-the-Counter Treatments: Non-antibiotic treatments are available at pharmacies and may help alleviate symptoms.
- Seek Medical Advice: If symptoms persist, worsen, or recur frequently, contact your GP or visit a local sexual health clinic for diagnosis and appropriate treatment.
Testing and Diagnosis of Bacterial Vaginosis
Diagnosis of BV typically involves a medical assessment and may include:
- Symptom-Based Diagnosis: In many cases, healthcare providers can diagnose BV based on the appearance of the discharge and reported symptoms.
- Internal Examination: If necessary, your healthcare provider may perform an internal examination using a speculum to observe the vagina and collect a sample of discharge using a swab.
- Laboratory Testing: In some cases, the swab sample may be sent to a lab for further analysis to confirm the diagnosis and rule out other infections, such as STIs.
Treatment for Bacterial Vaginosis
BV is generally treated with antibiotics, which can include:
- Oral Antibiotics: Medications like metronidazole tablets are commonly prescribed to be taken by mouth.
- Topical Antibiotics: In some cases, an antibiotic cream or gel (such as metronidazole gel or clindamycin cream) may be recommended for insertion into the vagina.
Important Considerations During Treatment:
- Inform Your Healthcare Provider: If you are pregnant, suspect you might be pregnant, or are breastfeeding, inform your healthcare provider, as this may influence the type of treatment prescribed.
- Sexual Activity: While BV is not sexually transmitted, antibiotics and topical treatments may affect the effectiveness of condoms and diaphragms. Your healthcare provider or pharmacist can provide further guidance on this.
Causes of Bacterial Vaginosis
The vagina naturally contains a mix of “good” and “bad” bacteria, with lactobacilli being the primary type of bacteria that help maintain a healthy vaginal environment. BV occurs when the balance is disrupted, leading to a decrease in lactobacilli and an overgrowth of other bacteria. While the exact cause of this imbalance is not fully understood, several factors can increase the risk of developing BV:
- New or Multiple Sexual Partners: While not considered an STI, having a new or multiple sexual partners can increase the likelihood of developing BV.
- Douching: Washing or cleaning out the vagina with water or other fluids can disrupt the natural balance of bacteria.
- Use of Scented Products: Perfumed soaps, vaginal sprays, and bubble baths can irritate the vaginal area and disrupt its natural environment.
- Smoking: Cigarette smoking has been linked to an increased risk of developing BV.
- Certain Sexual Practices: Receiving oral sex has been associated with BV in some cases.
Prevention of Bacterial Vaginosis
Although it may not be possible to completely prevent BV, there are steps you can take to reduce your risk:
- Avoid Douching: Douching can upset the natural balance of bacteria in the vagina and is not recommended for routine vaginal hygiene.
- Limit Use of Scented Products: Use mild, unscented soaps and avoid scented bubble baths, vaginal sprays, and deodorants.
- Practice Good Genital Hygiene: Wash the external genital area with plain water or a mild, unscented cleanser. Avoid scrubbing the area harshly.
- Wear Breathable Clothing: Opt for cotton underwear and avoid tight-fitting clothes that can trap moisture and create an environment conducive to bacterial imbalance.
When to Seek Medical Advice
Contact your GP or visit a sexual health clinic if:
- You experience changes in your vaginal discharge, such as a fishy odor or a change in color or consistency.
- You have symptoms that persist or worsen despite home care measures.
- You experience recurrent episodes of BV.
Potential Complications of Untreated BV
While BV itself is not usually serious, untreated BV can lead to complications, such as:
- Increased Risk of STIs: BV can make you more susceptible to certain sexually transmitted infections.
- Pregnancy Complications: Pregnant women with untreated BV may be at increased risk for preterm birth or low birth weight.
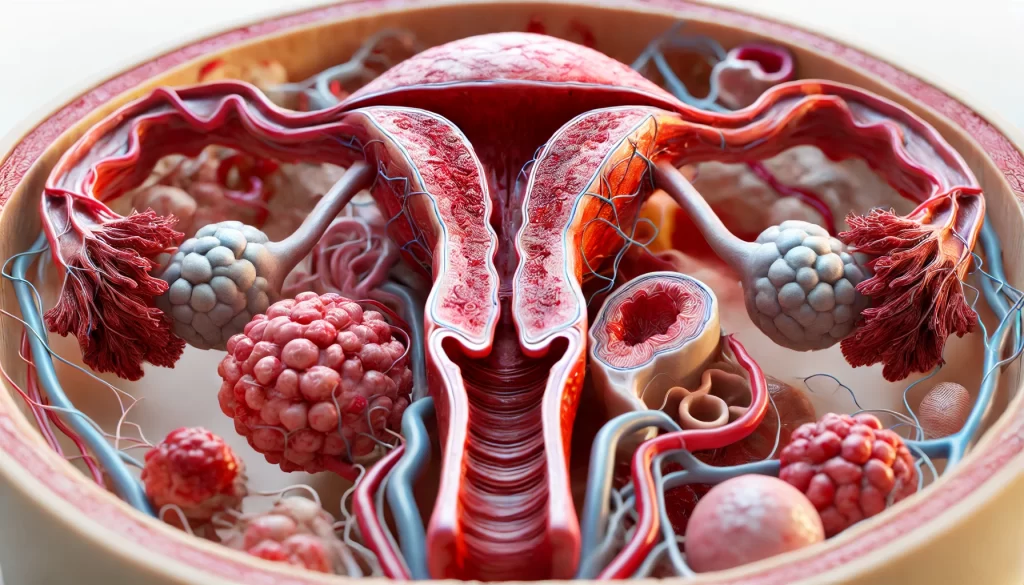
- Pelvic Inflammatory Disease (PID): In rare cases, BV can lead to PID, a serious infection of the female reproductive organs.
Recurrence of Bacterial Vaginosis
BV can recur after treatment, sometimes within a few weeks or months. If this happens, consult with your healthcare provider to discuss long-term treatment strategies or lifestyle changes that may help prevent recurrence.
By maintaining good hygiene and being aware of potential triggers, you can manage and reduce the risk of bacterial vaginosis. If symptoms occur, prompt treatment and medical advice can ensure effective management and prevent complications.