About Addison’s disease
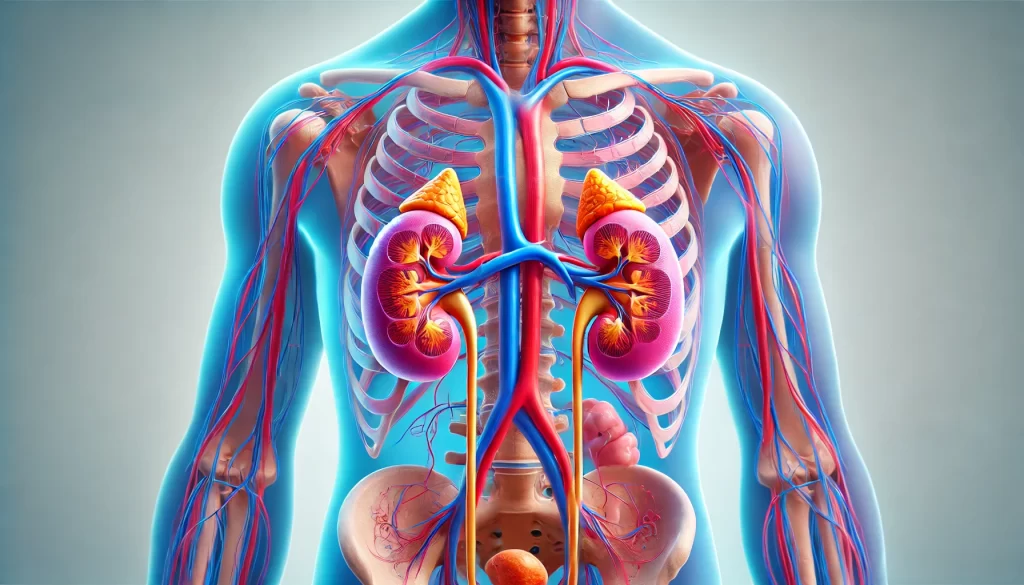
Addison’s disease, also known as primary adrenal insufficiency or hypoadrenalism, is a rare disorder that affects the adrenal glands, which are small organs located on top of each kidney. These glands are crucial for producing the hormones cortisol, aldosterone, and adrenaline, which regulate various bodily functions including metabolism, blood pressure, and response to stress.
Overview of Addison’s Disease
- Prevalence: It affects about 8,400 people in the UK and can occur at any age but is most commonly diagnosed between the ages of 30 and 50.
- Gender Disparity: The condition is more prevalent in women than men.
Symptoms
Initial symptoms of Addison’s disease are often nonspecific and can be mistaken for other conditions like flu or depression. These include:
- Fatigue and lack of energy or motivation
- Muscle weakness
- Low mood or depression
- Loss of appetite and unintentional weight loss
- Increased thirst
As the disease progresses, more severe symptoms may develop:
- Dizziness or fainting
- Muscle cramps
- Extreme exhaustion
- Darkened skin, especially in areas of friction, scars, or gums
Causes
- Autoimmune Response: In most cases (70% to 90% in the UK), Addison’s disease is autoimmune, where the immune system mistakenly attacks the adrenal cortex.
- Other Causes: Less common causes include infections like tuberculosis, which can damage the adrenal glands.
Diagnosis
Due to its subtle onset and general symptoms, diagnosing Addison’s disease can be challenging. If Addison’s disease is suspected based on symptoms, doctors will perform tests to measure cortisol and aldosterone levels and may conduct ACTH stimulation tests to assess adrenal function.
Treatment
Addison’s disease requires lifelong hormone replacement therapy to manage symptoms and maintain normal bodily functions. Treatments typically involve:
- Oral corticosteroids to replace cortisol
- Fludrocortisone for aldosterone replacement
Living with Addison’s Disease
With proper treatment, most individuals with Addison’s disease can lead active lives with a normal lifespan. However, they must manage potential bouts of fatigue and may have other associated autoimmune conditions such as diabetes or hypothyroidism.
Emergency Situations: Adrenal Crisis
An adrenal crisis is a life-threatening emergency that occurs when cortisol levels drop drastically, often triggered by stress, illness, or missed medication. Symptoms include severe nausea, vomiting, headache, confusion, and weakness. Immediate medical treatment with intravenous injections of hydrocortisone is necessary.
Monitoring and Research
Patients with Addison’s disease may have their details added to the National Congenital Anomaly and Rare Diseases Registration Service (NCARDRS) to help improve understanding and treatments. Participation is voluntary and individuals can opt out at any time.
Proper education about managing the disease and understanding when to seek emergency medical attention are vital for anyone diagnosed with Addison’s disease.
Symptoms of Addison’s disease
The symptoms of Addison’s disease often develop slowly and can be vague, which may cause them to be mistaken for other conditions. Here’s a detailed look at the progression and symptoms of Addison’s disease:
Early Symptoms
- Fatigue and Lethargy: A profound sense of energy loss and unusual tiredness that doesn’t improve with sleep.
- Muscle Weakness: Difficulty in performing everyday activities that were once easy.
- Low Mood and Irritability: Emotional changes including mild depression or increased irritability.
- Appetite Loss and Weight Loss: Significant decrease in appetite leading to weight loss without trying.
- Increased Thirst and Urination: Constant thirst and frequent need to urinate, reflecting changes in metabolism.
- Salt Craving: An unusual desire for salty foods due to sodium imbalance.
Dehydration
As a direct effect of decreased aldosterone, dehydration can occur, marked by:
- Dry skin and mucous membranes
- Dizziness or lightheadedness
- Extreme thirst
Later Symptoms
These may develop if the condition progresses without adequate treatment:
- Hypotension: Low blood pressure that can cause fainting or dizziness upon standing.
- Gastrointestinal Distress: Nausea, vomiting, and diarrhea, which can exacerbate dehydration.
- Pain: Occurrence of abdominal, joint, or back pain.
- Skin Changes: Development of a tan or darkening of the skin, especially noticeable in scars, skin folds, and gums.
- Sexual Dysfunction: Reduced sexual drive or interest, and in women, irregular or absent menstrual periods.
Acute Addisonian Crisis
An adrenal crisis represents a sudden worsening of symptoms, potentially leading to:
- Severe dehydration
- Low blood pressure and rapid heart rate
- Severe weakness and fatigue
- Mental status changes, including confusion or coma
Importance of Timely Treatment
Early recognition and treatment of Addison’s disease are crucial. Treatment typically involves hormone replacement therapy to correct the levels of steroid hormones the body isn’t producing. Ongoing management of the disease includes regular follow-up care to adjust medication as needed and monitoring for potential complications.
Emergency Response
An adrenal crisis is a medical emergency. If you suspect someone is experiencing such a crisis, immediate action to seek emergency medical services is critical to prevent potentially life-threatening complications.
Understanding these symptoms and their progression is vital for timely diagnosis and to prevent acute crises, ensuring those with Addison’s disease can manage their condition effectively.
Causes of Addison’s disease
Addison’s disease, or primary adrenal insufficiency, arises when the adrenal glands, located above each kidney, fail to produce sufficient amounts of hormones such as cortisol and aldosterone. Here are the various factors that can cause this condition:
1. Autoimmune Disorders
The most common cause in industrialized nations is autoimmune disorders, which account for 70% to 90% of cases in the UK. In these cases, the body’s immune system mistakenly attacks and destroys the adrenal cortex. This autoimmune assault prevents the adrenal glands from producing critical hormones.
2. Genetic Factors
There’s a genetic predisposition that can increase the likelihood of developing autoimmune disorders, including Addison’s disease. People with certain genetic backgrounds are more prone to these conditions, especially if they or close family members have other autoimmune diseases such as type 1 diabetes, vitiligo, or autoimmune thyroid disease.
3. Infections
Globally, tuberculosis (TB) is a significant infectious cause of Addison’s disease, particularly in less developed countries. Although less common in the UK, TB can severely damage the adrenal glands if it spreads beyond the lungs. Other infections that might lead to Addison’s include fungal infections and HIV/AIDS, which compromise the immune system and can affect the adrenal glands.
4. Hemorrhage or Bleeding
Bleeding into the adrenal glands, known as adrenal hemorrhage, can lead to Addison’s disease. This can occur in the context of severe infections like meningococcal meningitis or sepsis, where blood clotting becomes abnormal.
5. Cancer
Cancer cells that metastasize from other parts of the body to the adrenal glands can impair adrenal function, although this is a less common cause.
6. Amyloidosis
In this condition, abnormal protein deposits (amyloid) accumulate in the adrenal glands, disrupting their function.
7. Surgical Removal
Removal of the adrenal glands (bilateral adrenalectomy) due to cancer or other diseases eliminates the source of cortisol and aldosterone production, resulting in Addison’s disease.
8. Genetic Diseases
Certain rare genetic disorders like adrenoleukodystrophy (ALD), which typically affects young boys, disrupt the function of the adrenal glands as well as the nervous system.
9. Medications
Long-term use of certain steroids can suppress adrenal function, which can lead to Addison’s disease if the medications are stopped abruptly.
10. Treatment for Other Conditions
Treatments intended to manage other health issues, like Cushing’s syndrome, may involve medications or procedures that impair adrenal gland function.
Understanding these causes is essential for diagnosing and managing Addison’s disease effectively. Early recognition and treatment can significantly improve quality of life and prevent serious complications such as adrenal crisis.
Diagnosing Addison’s disease
Diagnosing Addison’s disease involves several steps and various types of tests because its symptoms can be similar to those of many other health conditions. Here’s a detailed look at the diagnostic process:
Initial Consultation
Your GP will discuss your symptoms and medical history with you, particularly looking for signs of autoimmune disorders, which are common in families with Addison’s disease. During the physical exam, the GP will look for signs of hyperpigmentation, which is a common symptom of Addison’s disease but is not present in all cases. This discoloration typically appears in skin folds, on scars, and on the lips and gums.
Blood Pressure Test
A key physical test involves checking for low blood pressure, particularly postural or orthostatic hypotension, which occurs when your blood pressure drops as you stand up from lying down.
Blood Tests
Blood tests are crucial for measuring levels of sodium, potassium, and cortisol. Addison’s disease may be indicated by:
- Low sodium levels
- High potassium levels
- Low cortisol levels
Further tests will check for:
- Low aldosterone levels
- High levels of adrenocorticotrophic hormone (ACTH)
- Low glucose levels
- Presence of adrenal antibodies
Synacthen Stimulation Test
If initial blood tests suggest Addison’s disease, or if your symptoms are particularly indicative of the condition, you may undergo a Synacthen stimulation test. This test assesses adrenal gland function by measuring how your cortisol levels change in response to synthetic ACTH. Cortisol levels are measured before and after an ACTH injection, typically at 30 and 60 minutes after administration. Poor response or low cortisol despite high ACTH levels typically confirms Addison’s disease.
Thyroid Function Test
Because autoimmune disorders can affect multiple glands, thyroid function tests may also be performed to check for concurrent conditions like hypothyroidism, which often occurs alongside Addison’s disease.
Imaging Tests
CT or MRI scans of the adrenal glands might be conducted to look for physical damage or other abnormalities that could explain hormone deficiencies.
Diagnosis During an Adrenal Crisis
In severe cases, particularly during an adrenal crisis, immediate treatment is prioritized over a formal diagnosis. Blood samples may still be taken to check cortisol levels and other indicators. However, treatment with steroid injections and IV fluids typically begins immediately to address the critical condition.
Reporting to Authorities
After diagnosis, individuals with certain professional driving licenses must report their condition to the relevant licensing authorities, as Addison’s disease can affect the ability to operate vehicles safely.
This comprehensive approach helps ensure an accurate diagnosis of Addison’s disease, facilitating timely and effective treatment to manage the condition.
Treating Addison’s disease
Treating Addison’s disease involves lifelong hormone replacement therapy to manage symptoms and prevent potentially life-threatening adrenal crises. Here’s an overview of the treatment approaches and considerations for managing Addison’s disease effectively:
Medication
Addison’s disease is primarily treated through hormone replacement therapy to compensate for the insufficient production of cortisol and aldosterone by the adrenal glands:
- Hydrocortisone is commonly prescribed to replace cortisol and is usually taken in tablet form two or three times a day.
- Fludrocortisone is used to replace aldosterone, which helps regulate the balance of salt and water in the body.
Lifestyle Adjustments
Patients may need to adjust their salt intake based on their medication levels and bodily needs, especially under the guidance of a healthcare provider.
Monitoring Medication Side Effects
While generally safe, corticosteroid therapy can cause side effects if doses are too high, including osteoporosis, mood swings, and insomnia. Regular follow-ups with healthcare providers are crucial to adjust doses and minimize side effects.
Managing Fatigue
Many with Addison’s manage bouts of fatigue. Learning personal limits and adjusting activities can help balance energy levels.
Emergency Preparedness
Patients should be prepared for adrenal crises, which require immediate medical treatment:
- Emergency Injection: Patients are often advised to carry an emergency hydrocortisone injection kit, especially when traveling or unable to take oral medications.
- Medical Alert Identification: Wearing a medical alert bracelet is crucial to alert medical personnel of the need for immediate cortisol replacement in emergencies.
Regular Medical Care
Regular check-ups with an endocrinologist are necessary to monitor the condition and adjust treatment as needed. Patients should also educate family and close contacts about how to recognize and respond to signs of an adrenal crisis.
Adjusting Doses During Stress
Patients may need to increase medication doses during periods of physical stress, such as illness, surgery, or severe emotional distress, to mimic the body’s natural response of increasing cortisol production.
Avoiding Triggers
Patients should avoid factors that could exacerbate their condition, such as infections, dehydration, and excessive physical stress. Preventive measures, such as flu vaccines and regular hand-washing, can help reduce health risks.
Comprehensive Support
Counseling and support groups can help patients and families cope with the emotional and physical challenges of living with Addison’s disease.
By adhering to a treatment plan and working closely with healthcare professionals, most people with Addison’s disease can lead active, normal lives despite the need for continuous medication.