Introduction to Acute Lymphoblastic Leukaemia (ALL) for Teenagers and Young Adults
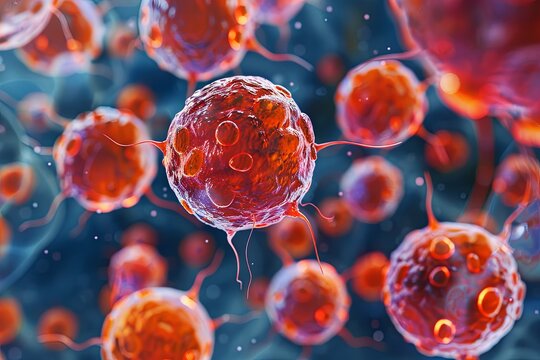
Acute lymphoblastic leukaemia (ALL) is a type of cancer that affects white blood cells and can develop rapidly. While ALL is more common in children, it also affects teenagers and young adults. Another main type of leukaemia that can occur in this age group is acute myeloid leukaemia (AML).
If you are looking for information about ALL in people of all ages, please refer to our general ALL section.
What is Leukaemia?
Leukaemia is a cancer of the white blood cells. Normally, white blood cells develop, mature, and reproduce in an orderly manner in the bone marrow—the soft tissue inside bones where blood cells are produced. In leukaemia, the process becomes uncontrolled, leading to the continuous production of immature white blood cells called blasts. These immature cells accumulate in the bone marrow, crowding out healthy cells and reducing the body’s ability to:
- Fight infection with healthy white blood cells.
- Carry oxygen throughout the body with red blood cells.
- Clot blood and prevent excessive bleeding with platelets.
Symptoms of Acute Lymphoblastic Leukaemia (ALL)
Many of the symptoms of ALL result from a reduction in healthy blood cells. Symptoms can vary but may include:
- Pale Skin and Fatigue: Due to anaemia (low red blood cell count), leading to feelings of exhaustion.
- Easy Bruising and Prolonged Bleeding: Caused by a lower-than-normal number of platelets.
- Frequent Infections: Caused by a lack of mature white blood cells to fight infections.
- Bone and Joint Pain: Caused by overcrowding of leukaemia cells in the bone marrow.
- Swollen Lymph Nodes: Particularly in the neck, underarm, or groin.
- General Feeling of Unwellness: Including persistent tiredness and feeling run down.
- Fever and Sweats: High temperature without a clear cause, such as an infection.
- Headaches and Visual Disturbance.
It is important to remember that these symptoms can be caused by conditions other than ALL. However, if you are concerned, it is important to speak to your GP. They will conduct an examination and, if necessary, refer you to a specialist for further tests.
Causes of Acute Lymphoblastic Leukaemia (ALL)
The exact cause of ALL is unknown, but ongoing research aims to identify potential factors. Certain genetic conditions can increase the risk of developing ALL. These include:
- Down’s Syndrome
- Li-Fraumeni Syndrome
These are genetic conditions present from birth. However, most cases of ALL do not have a known specific cause.
What to Do If You’re Worried About ALL
If you think you may have symptoms of ALL, speak to your GP. They can discuss your concerns, perform an examination, and arrange any necessary tests.
Leukaemia, Blood Tests, and Bone Marrow: An Overview
Understanding leukaemia involves knowing how blood and bone marrow function. Leukaemia is a cancer that affects the white blood cells produced in the bone marrow.
The Role of Bone Marrow and Blood Cells
Bone marrow is a spongy tissue found inside bones that acts as a blood cell factory. It produces millions of blood cells daily through a process that starts with stem cells. Stem cells can develop into different types of blood cells, depending on the body’s needs.
The Three Main Types of Blood Cells
White Blood Cells (WBCs):
These cells are vital for fighting infections and keeping the immune system strong.Red Blood Cells (RBCs):
RBCs transport oxygen from the lungs throughout the body, supplying energy and promoting proper organ function.Platelets:
Platelets help clot blood, preventing excessive bleeding from cuts and injuries.
Blood Cell Development Process
The bone marrow produces new blood cells, initially in an immature state known as blasts. The main role of blast cells is to multiply and create more blood cells. However, blast cells cannot carry oxygen, fight infection, or clot blood until they mature.
Once the blood cells are fully developed, they leave the bone marrow and enter the bloodstream to perform their specific functions.
How Leukaemia Develops
In leukaemia, the process of creating new white blood cells becomes uncontrolled. Immature white blood cells (blasts) continue to multiply rapidly. As these leukaemia cells accumulate, they crowd out the healthy white cells, red cells, and platelets in the bone marrow. This imbalance prevents the bone marrow from making healthy blood cells, leading to symptoms such as fatigue, infection, and easy bruising.
Types of Leukaemia
Leukaemia is classified based on the type of white blood cell affected:
- Lymphoblasts: These make lymphocytes, a type of white blood cell.
- Myeloid Cells (Myeloblasts): These produce other white blood cells, such as neutrophils.
Common Types of Leukaemia in Teenagers and Young Adults
Acute Myeloid Leukaemia (AML):
AML originates from abnormal myeloid cells.Acute Lymphoblastic Leukaemia (ALL):
ALL develops from abnormal lymphoblasts.
Chronic leukaemias are more commonly found in older adults.
Related Topics for Further Reading
If you are interested in more detailed information about acute lymphoblastic leukaemia (ALL), explore our dedicated sections on:
- Symptoms and Causes of ALL
- Diagnostic Tests for ALL
- Treatment Options for ALL
For a broader perspective on ALL that applies to people of all ages, refer to our general ALL section.
Tests for Acute Lymphoblastic Leukaemia (ALL)
If you have symptoms that may be related to acute lymphoblastic leukaemia (ALL), it’s essential to consult your GP (General Practitioner). While symptoms of ALL can be caused by many different conditions, a medical evaluation is important to determine the cause and to arrange for any necessary tests.
Visiting Your GP
During your appointment, your GP will:
- Examine you: Your doctor will check for signs that could be related to ALL or other health issues.
- Order blood tests: Blood tests are used to help diagnose ALL. If leukaemia cells are found, you will be referred to a haematologist, a doctor who specializes in blood disorders.
At the Hospital: Specialist Consultation
The haematologist will:
- Examine you: They will review your symptoms and recent illnesses.
- Arrange further tests: Additional testing is necessary to confirm the diagnosis and determine the best treatment options.
Tests You May Need
1. Blood Tests
Even if you have already had initial blood tests, further testing may be required to:
- Assess changes in leukaemia cells.
- Help the doctors decide on the most effective treatment plan.
2. Bone Marrow Test
- Purpose: To count the number of leukaemia cells in the bone marrow.
- Procedure: A small sample of bone marrow is taken (usually from the hip bone) using a needle. It may be slightly uncomfortable but is typically performed under local anaesthetic.
- Testing: The sample is used for cytogenetic and immunophenotyping tests to provide detailed information about the type of leukaemia.
3. Lumbar Puncture
- Purpose: To check if leukaemia cells have spread to the fluid surrounding the brain and spinal cord.
- Procedure: A needle is used to remove a small sample of cerebrospinal fluid (CSF) from the lower back.
4. Chest X-Ray
- Purpose: To check for any swollen lymph nodes (glands) in the chest.
Additional Tests
If you are diagnosed with ALL, further tests may be required to assess how your body is functioning. These may include:
- Blood Tests: To evaluate liver, kidney, and overall health.
- Ultrasound Scan: Used to check the liver, spleen, and kidneys.
- Echocardiogram: An ultrasound of the heart to assess its function.
Why These Tests Are Important
While this may seem like a lot of tests, they provide critical information to guide your treatment. Accurate diagnosis and monitoring help doctors develop the most effective treatment plan tailored to your needs.
Treating Acute Lymphoblastic Leukaemia (ALL)
The primary treatment for acute lymphoblastic leukaemia (ALL) is chemotherapy. This involves the use of anti-cancer drugs to eliminate leukaemia cells, often in combination with steroids to enhance the effectiveness of the chemotherapy.
ALL treatment can be intensive at times and may cause side effects. Hospital staff are always available to support you during difficult moments. It’s important to communicate openly with your doctors and nurses about how you’re feeling. They can provide medications and support to help manage side effects and keep you strong throughout treatment.
Phases of ALL Treatment
ALL is typically treated in three phases:
- Remission Induction: The goal is to eliminate as many leukaemia cells as possible and achieve remission (no signs of leukaemia in the blood or bone marrow).
- Consolidation and Delayed Intensification: This phase ensures that remaining leukaemia cells are eradicated.
- Maintenance Therapy: Long-term treatment designed to prevent relapse by keeping leukaemia cells away.
Starting Chemotherapy
Chemotherapy usually begins soon after diagnosis and is administered in a hospital setting to closely monitor your health. Patients aged 18 or younger will be treated at a Principal Treatment Centre (PTC) for teenagers and young adults (TYA). Patients aged 19 or older have the option of treatment at the PTC or a TYA-designated hospital closer to home.
How Chemotherapy Is Administered
- Tablets, Injections, and Intravenous (IV) Treatment: Chemotherapy may be given orally, via injections, or through an IV line directly into the bloodstream.
- Central Nervous System (CNS) Therapy (Intrathecal Therapy): Chemotherapy is delivered into the fluid around the spinal cord to target any hidden leukaemia cells. This involves injecting chemotherapy into the cerebrospinal fluid (CSF) using a method similar to a lumbar puncture.
Remission Induction
The initial phase focuses on eliminating as many leukaemia cells as possible. Achieving remission means there is no detectable sign of leukaemia cells in your blood or bone marrow.
Treatment Components
- Chemotherapy: Administered to kill leukaemia cells, including CNS therapy.
- Steroids: Used to enhance the effectiveness of chemotherapy.
- Protective Drugs: Medications like allopurinol or rasburicase protect the kidneys during treatment, and tablets like ranitidine or lansoprazole prevent indigestion and ulcers.
This phase usually takes about 5 weeks but may vary. During this time, you will stay in the hospital to closely monitor your progress.
CNS Therapy
Since traditional chemotherapy may not effectively reach the brain or spinal cord, intrathecal therapy is administered. Methotrexate is injected into the cerebrospinal fluid (CSF) to target hidden leukaemia cells in the CNS.
Possible Side Effects of Intrathecal Therapy
Most people do not experience significant side effects, but potential reactions include:
- Headaches, dizziness, tiredness, or blurry vision.
- Rarely, symptoms such as seizures, weakness, or changes in alertness may occur but usually resolve completely.
Consolidation and Delayed Intensification
After achieving remission, further treatment is needed to eliminate any remaining leukaemia cells. This phase involves using various chemotherapy drugs to prevent drug resistance. Treatment lasts about 5 to 6 months and may involve outpatient visits or short hospital stays.
Common Drugs Used
- Cyclophosphamide
- Cytarabine (Ara-C)
- Mercaptopurine
- Methotrexate
- Vincristine
- Asparaginase
- Doxorubicin
Maintenance Therapy
Maintenance therapy is aimed at preventing relapse by using low doses of chemotherapy over a longer period. Most of this treatment is conducted on an outpatient basis, allowing you to continue with daily activities. Maintenance therapy typically lasts just over 3 years for boys and just over 2 years for girls.
Maintenance Cycle (12 Weeks)
- Daily Mercaptopurine Tablets
- Weekly Methotrexate Tablets
- Steroid Tablets for 5 days every 4 weeks
- Vincristine Chemotherapy every 4 weeks
- Methotrexate (CNS therapy) every 12 weeks
Regular check-ups, usually every week or two, are essential to monitor progress, adjust drug doses, and address any concerns.
Coping with Treatment
Treatment can be challenging, and side effects may include:
- Fatigue, nausea, and hair loss
- Risk of infection and anaemia
- Mood changes and irritability (due to steroids)
Talking to friends, family, doctors, nurses, or support groups can make it easier to manage the emotional and physical challenges.