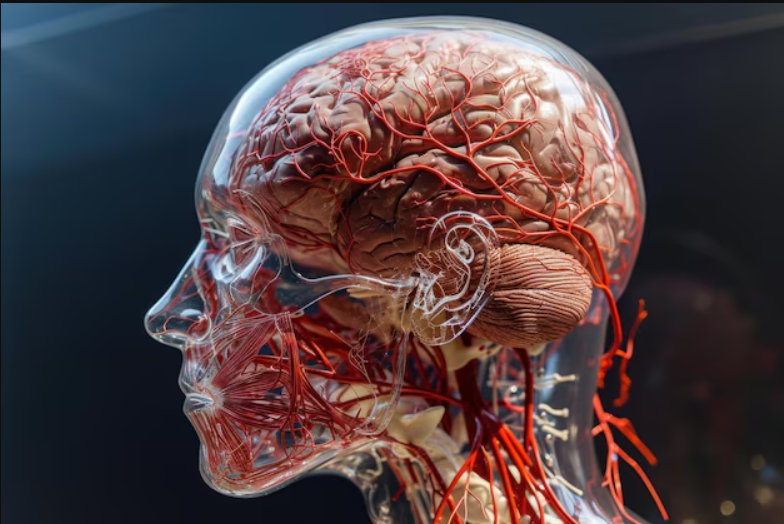
Understanding Brain Stem Death
Brain stem death occurs when the brain stem no longer functions, leading to a permanent loss of consciousness and the inability to breathe independently. In such cases, a ventilator may keep the person’s heart beating and oxygen circulating, but there is no possibility of recovery or consciousness.
When a person’s brain stem is permanently damaged and no longer functioning, medical professionals can confirm that the individual is dead.
Confirming Death
In the past, confirming death was simpler; it was identified when the heart stopped beating and a person was unresponsive with no signs of breathing. The absence of blood flow and oxygen would lead to permanent brain stem function loss within minutes. However, modern medical advances have made this process more complex, as ventilators can keep the heart beating and oxygen flowing even after the brain stem has ceased functioning. Despite this, once brain stem function has permanently stopped, the heart will inevitably stop beating, even with artificial support.
To spare families from unnecessary suffering, once there is undeniable evidence of brain death, doctors will disconnect the person from the ventilator.
The Role of the Brain Stem
The brain stem is the lower part of the brain, connecting it to the spinal cord and controlling essential functions necessary for life, including:
- Breathing
- Heartbeat regulation
- Blood pressure management
- Swallowing
The brain stem also facilitates communication between the brain and the rest of the body, contributing to core functions such as consciousness, movement, and awareness. Once brain death occurs, it is impossible for the person to regain consciousness or any level of independent function.
Causes of Brain Death
Brain death can result from:
- Lack of blood or oxygen supply to the brain, caused by:
- Cardiac arrest (heart stops beating)
- Heart attack (blocked blood supply to the heart)
- Stroke (blocked or interrupted blood supply to the brain)
- Blood clot blocking circulation
- Other causes:
- Severe head injury
- Brain haemorrhage (bleeding in the brain)
- Brain infections such as encephalitis
- Brain tumors
Difference Between Brain Death and a Vegetative State
It is important to differentiate brain death from a vegetative state. In a vegetative state, a person may exhibit signs of wakefulness (e.g., opening their eyes) but cannot respond meaningfully to their surroundings. Unlike brain death, a vegetative state often involves a functioning brain stem, enabling:
- Some degree of consciousness
- Independent breathing
- A slim possibility of recovery
In contrast, a person who is brain dead has no chance of recovery, as their body cannot function without artificial support.
Confirming Brain Death
Diagnosing brain death requires careful testing to rule out other factors and confirm irreversible brain stem failure. Certain conditions, such as drug overdoses (e.g., barbiturates) and severe hypothermia (body temperature below 28°C), can mimic brain death symptoms. To ensure accurate diagnosis, a series of tests are conducted, including:
Initial Assessment
Doctors will ensure symptoms are not caused by:
- Drug overdose (including illegal drugs, poisons, and tranquilizers)
- Low body temperature (hypothermia)
- Severe thyroid gland underactivity
Tests to Confirm Brain Death
The diagnosis is made by two senior doctors, neither of whom can be part of the hospital’s transplant team. They conduct a series of tests twice to ensure accuracy, including:
- Shining a torch into the eyes to check for light response.
- Stroking the cornea (outer eye layer) with a tissue or cotton wool to test for a reaction.
- Applying pressure to the forehead and pinching the nose to observe any response.
- Introducing ice-cold water into the ears to check for eye movement.
- Placing a thin tube into the trachea to test for gagging or coughing reflex.
- Disconnecting the ventilator temporarily to see if there is any attempt to breathe independently.
Brain death is confirmed if the individual shows no response to all these tests.
Reflex Movements After Brain Death
Occasionally, reflex movements of the limbs or torso may be observed after brain death is diagnosed. These movements originate from the spinal cord, not the brain, and do not affect the diagnosis.
Organ and Tissue Donation
After brain death is confirmed, it may be possible to donate organs and tissues to save or improve the lives of others. Organ donation is rare, with only 1% of people dying in a manner that allows it. Specialist nurses discuss donation possibilities with families, considering the individual’s wishes and checking the NHS Organ Donor Register if applicable.