Schizophrenia is one of the most complex and misunderstood mental health disorders, affecting approximately 1% of the global population. Despite decades of research, the precise causes remain elusive. In this comprehensive blog post, we will delve deep into the etiology of schizophrenia—unraveling the intricate web of genetic, neurobiological, environmental, and psychosocial factors that contribute to its development. Whether you’re a student, a mental health professional, or simply a curious reader, this guide will equip you with a clear understanding of the subject and highlight why it matters today.
Introduction
Imagine being faced with a condition that disrupts the very fabric of one’s thoughts, perceptions, and emotional experiences—a condition that affects not only the individual but also ripples through families and communities. This is the reality of schizophrenia. Despite its relatively low prevalence, the etiology of schizophrenia has captivated scientists and clinicians alike due to its complexity and the profound implications for treatment and recovery.
In today’s post, we’ll explore:
- What exactly is meant by the etiology of schizophrenia?
- The evolution of our understanding from early theories to cutting-edge research.
- The interplay between genetics, brain chemistry, prenatal influences, and social environments.
By the end, you’ll appreciate why understanding the causes of schizophrenia isn’t just an academic exercise—it’s key to improving lives, guiding treatment strategies, and reducing the stigma associated with mental illness.
What Is Schizophrenia?
Schizophrenia is a chronic, severe mental disorder that affects how a person thinks, feels, and behaves. It is often characterized by a combination of hallucinations, delusions, disorganized speech, and impaired cognitive abilities. While the condition is sometimes sensationalized in popular media, the day-to-day reality for those with schizophrenia involves significant challenges in maintaining relationships, employment, and self-care.
Key points include:
- Disruption in Thought Processes: Individuals may experience a breakdown in the ability to think clearly or logically.
- Altered Perceptions: Hallucinations, especially auditory ones, are common.
- Emotional Dysregulation: Emotional responses might seem blunted or inappropriate to the situation.
- Social Withdrawal: The disorder often leads to isolation and difficulties in social interaction.
Understanding the etiology of schizophrenia is essential, as it provides insights into why these symptoms occur and how various factors interact to give rise to the disorder.
Defining the Etiology of Schizophrenia
At its core, the term etiology of schizophrenia refers to the study of the origins and causes of schizophrenia. Unlike conditions with a single causative agent, schizophrenia is recognized as a multifactorial disorder. This means that no one single factor is responsible; instead, a complex interplay of multiple elements—ranging from genetics to environmental stressors—contributes to its onset.
Key Characteristics of Its Etiology:
- Multifactorial Nature: Involves genetic predisposition, neurochemical imbalances, and environmental triggers.
- Interdisciplinary Focus: Studies span across fields such as psychiatry, neurology, genetics, immunology, and sociology.
- Dynamic Interactions: Factors often do not work in isolation; instead, they interact dynamically over a person’s lifespan.
This comprehensive perspective is crucial for developing effective treatments and prevention strategies. By appreciating the varied components that contribute to schizophrenia, researchers and clinicians can better tailor interventions to individual needs.
Historical and Contextual Background
Early Theories and Milestones
The journey to understanding the etiology of schizophrenia is a tale of evolving ideas. In the early 20th century, the condition was often attributed to psychological conflicts or even moral failings. Psychoanalytic theories, for example, once posited that dysfunctional family dynamics or “schizophrenogenic mothers” were to blame—a notion that has long been debunked.
Shift to Biological Explanations
The mid-20th century marked a pivotal shift toward biological explanations:
- Discovery of Neurotransmitter Imbalances: Early research began linking symptoms of schizophrenia to disruptions in brain chemistry, particularly dopamine.
- Advances in Brain Imaging: Techniques such as CT and MRI scans provided visual evidence of structural brain abnormalities in patients with schizophrenia.
- Genetic Studies: Twin, family, and adoption studies reinforced the idea that genetics played a significant role in susceptibility.
Notable Historical Anecdotes
- The Dopamine Hypothesis: This theory emerged from observations that antipsychotic medications, which primarily block dopamine receptors, alleviate psychotic symptoms. It laid the groundwork for understanding the neurochemical underpinnings of schizophrenia.
- The Neurodevelopmental Hypothesis: Emerging research in the late 20th century suggested that disruptions in brain development during prenatal or early life stages could predispose individuals to schizophrenia later in life.
Today, the etiology of schizophrenia is recognized as a mosaic of factors—a perspective that continues to evolve with new research and technological advances.
In-Depth Exploration of Contributing Factors
Understanding the etiology of schizophrenia requires an examination of several interrelated components. Here, we break down the main contributing factors:
Genetic Factors
The Role of Heredity
Genetic predisposition is one of the most well-documented contributors to schizophrenia. Research has consistently shown that the disorder tends to run in families. Key insights include:
- Twin Studies: Identical twins show a higher concordance rate for schizophrenia compared to fraternal twins. If one identical twin develops schizophrenia, the likelihood of the other doing so is significantly higher—though not 100%, indicating that genes are a major risk factor but not the sole determinant.
- Family Studies: Individuals with a first-degree relative (parent or sibling) diagnosed with schizophrenia are at a greater risk.
- Genome-Wide Association Studies (GWAS): These studies have identified numerous genetic variants associated with an increased risk, though each variant contributes only a small amount to overall susceptibility.
Gene-Environment Interactions
Genetic predisposition often interacts with environmental factors. For instance, a person with a genetic vulnerability might never develop schizophrenia unless exposed to specific stressors or adverse conditions. This interplay underscores the multifactorial nature of the disorder.
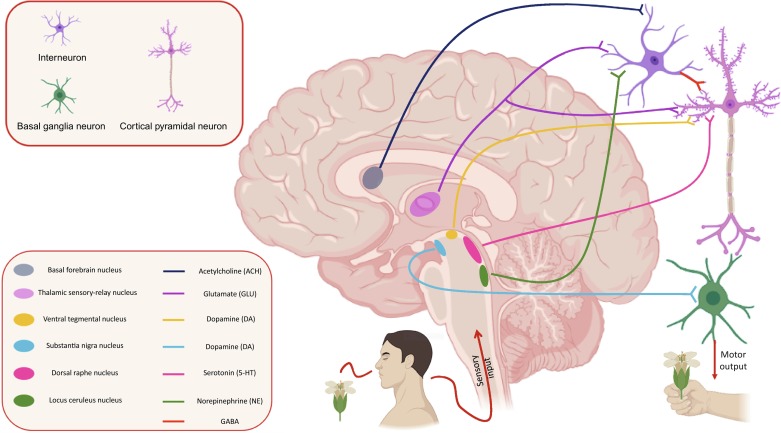
Neurobiological Underpinnings
Dopamine Hypothesis
One of the earliest and most influential theories in the study of schizophrenia is the dopamine hypothesis. It posits that an overactivity of dopamine neurotransmission in certain brain regions leads to the characteristic symptoms of schizophrenia, such as hallucinations and delusions.
- Evidence from Antipsychotics: Many antipsychotic drugs work by blocking dopamine receptors, which can help reduce psychotic symptoms.
- Limitations: However, the dopamine hypothesis does not explain all aspects of the disorder, and some patients do not respond to these medications as expected.
Glutamate and Other Neurotransmitters
Beyond dopamine, other neurotransmitters, particularly glutamate, are gaining attention:
- Glutamate Hypothesis: Some researchers suggest that hypofunction (reduced activity) of glutamate receptors, particularly the N-methyl-D-aspartate (NMDA) receptors, may play a role in schizophrenia.
- Serotonin and GABA: Imbalances in these neurotransmitter systems are also under investigation, highlighting that the neurobiology of schizophrenia is complex and involves multiple signaling pathways.
Brain Structure and Function
Advancements in neuroimaging have revealed several structural and functional brain abnormalities in individuals with schizophrenia:
- Enlarged Ventricles: Many patients show enlarged fluid-filled spaces in the brain, which may reflect loss of brain tissue.
- Cortical Thinning: Reductions in the thickness of the cerebral cortex have been observed, potentially linked to cognitive deficits.
- Abnormal Connectivity: Disruptions in the way different parts of the brain communicate with each other have also been documented.
Environmental and Prenatal Influences
Prenatal and Perinatal Factors
The environment in which a person develops—even before birth—can significantly impact the risk of developing schizophrenia:
- Maternal Infections: Infections during pregnancy, such as influenza, have been associated with an increased risk. The hypothesis is that maternal immune activation might affect fetal brain development.
- Nutritional Deficiencies: Lack of essential nutrients during pregnancy, like folic acid, may also contribute to abnormal brain development.
- Birth Complications: Obstetric complications, such as hypoxia (lack of oxygen) during birth, have been linked to later development of schizophrenia.
Childhood and Adolescence
Postnatal factors play a crucial role as well:
- Early-Life Stress: Childhood trauma, abuse, or neglect may interact with genetic predisposition to trigger the onset of schizophrenia.
- Substance Use: Early exposure to substances like cannabis, especially during adolescence—a critical period for brain development—has been implicated as a risk factor.
Psychosocial and Socioeconomic Factors
Social Isolation and Urban Upbringing
The social environment is another key piece of the puzzle:
- Urbanicity: Growing up or living in densely populated urban areas has been associated with a higher incidence of schizophrenia, potentially due to increased stress, social isolation, or exposure to environmental toxins.
- Family Dynamics and Stress: High levels of stress within the family or community, such as chronic poverty or social exclusion, can exacerbate underlying vulnerabilities.
Cultural Influences
Cultural perceptions and stigma around mental illness can also affect the course of schizophrenia. Misunderstandings about the condition may lead to delayed treatment, social ostracism, or even worsen the prognosis.
Immune System and Inflammatory Theories
Recent research has shed light on the potential role of the immune system in the etiology of schizophrenia:
- Neuroinflammation: There is growing evidence that chronic, low-grade inflammation in the brain might contribute to the development or exacerbation of symptoms.
- Autoimmune Hypotheses: Some studies have found a correlation between autoimmune disorders and schizophrenia, suggesting that an overactive immune response may play a role.
- Cytokine Imbalance: Elevated levels of pro-inflammatory cytokines have been observed in some patients, which might affect brain function and development.
Emerging Theories: Epigenetics and the Gut-Brain Axis
Epigenetics
Epigenetic mechanisms offer a promising explanation for how environmental factors can alter gene expression without changing the underlying DNA sequence:
- DNA Methylation: Changes in DNA methylation patterns have been observed in patients with schizophrenia, potentially affecting genes involved in brain development and neurotransmission.
- Histone Modification: Alterations in histone proteins can also influence gene expression, adding another layer of complexity to the genetic architecture of schizophrenia.
The Gut-Brain Axis
A burgeoning area of research is the connection between the gut microbiome and brain health:
- Microbial Imbalance: Some studies suggest that imbalances in gut bacteria may influence inflammation and neurotransmitter production, thereby impacting mental health.
- Immune Modulation: The gut-brain axis plays a role in immune regulation, potentially linking gastrointestinal health to the onset or progression of schizophrenia.
Real-World Examples and Case Studies
To bring these concepts to life, let’s consider some real-world scenarios and research case studies that illustrate the multifactorial nature of schizophrenia.
Case Study 1: Genetic Predisposition and Family History
Consider the case of two siblings raised in the same household. One sibling develops schizophrenia during late adolescence, while the other remains unaffected. Studies of similar cases have demonstrated that even with a shared genetic background, additional factors—such as environmental stress or prenatal complications—can determine whether the disorder manifests. This underscores the importance of looking at both genetic vulnerability and environmental triggers in the etiology of schizophrenia.
Case Study 2: Neuroimaging Insights
In a groundbreaking study using functional MRI (fMRI), researchers identified abnormal connectivity in the prefrontal cortex of patients with schizophrenia. These findings support the neurodevelopmental hypothesis, suggesting that early disruptions in brain development can lead to persistent functional impairments. The study further highlights how neuroimaging can serve as a valuable tool in unraveling the etiology of schizophrenia by revealing hidden abnormalities in brain structure and function.
Case Study 3: The Impact of Prenatal Exposure
Research following children born during influenza epidemics has revealed a higher incidence of schizophrenia in later life. In these cases, maternal infection during pregnancy appears to disrupt normal brain development, lending strong support to the role of prenatal factors in the etiology of schizophrenia. Such findings have significant implications for public health policies, emphasizing the need for preventative measures during pregnancy.
Case Study 4: Integrative Approaches
Modern research is increasingly taking an integrative approach—combining genetic studies, neuroimaging, and environmental assessments. For instance, a longitudinal study tracking high-risk individuals (those with a family history of schizophrenia) found that early interventions, such as stress management and nutritional support, could delay or even mitigate the onset of symptoms. This holistic view reinforces that the etiology of schizophrenia is not confined to one domain but is a result of multiple converging influences.
Importance and Applications
Understanding the etiology of schizophrenia is not merely an academic pursuit; it has profound implications for clinical practice, public policy, and societal attitudes toward mental health.
Advancing Treatment Strategies
- Personalized Medicine: By identifying genetic markers and environmental risk factors, clinicians can tailor interventions to an individual’s unique profile. This may include early intervention strategies, targeted pharmacological treatments, and cognitive therapies.
- Preventative Measures: Recognizing prenatal and early-life risk factors allows for the development of preventative strategies, such as improving maternal health and reducing exposure to environmental stressors.
- Improved Diagnostic Tools: Insights into neurobiological and inflammatory markers pave the way for more accurate and early diagnosis, which is crucial for effective management.
Informing Public Health Policy
- Early Screening Programs: Public health initiatives can incorporate screening for high-risk individuals based on family history and early-life factors, potentially reducing the long-term impact of schizophrenia.
- Education and Awareness: A nuanced understanding of the etiology of schizophrenia can help dispel myths and reduce stigma, fostering a more supportive environment for those affected.
Enhancing Research and Innovation
- Interdisciplinary Collaboration: Research into schizophrenia’s etiology encourages collaboration between geneticists, neuroscientists, psychologists, and sociologists. This cross-disciplinary approach is essential for tackling the multifaceted challenges posed by the disorder.
- Funding and Support: A deeper grasp of the underlying causes can drive investment in research, leading to novel therapeutic approaches and better overall outcomes for patients.
Social and Cultural Benefits
- Reducing Stigma: Public understanding of the complex origins of schizophrenia helps combat the stigma that often accompanies mental illness. Recognizing that multiple factors—many beyond an individual’s control—contribute to the condition can foster empathy and support.
- Empowering Patients and Families: Knowledge empowers those affected by schizophrenia to seek help early and to engage in treatment decisions that are informed by the latest scientific findings.
Common Misconceptions and FAQs
With a topic as multifaceted as the etiology of schizophrenia, several myths and misconceptions have taken root over time. Below, we address some common questions:
FAQs
Q: Is schizophrenia caused solely by genetics?
A: No. Although genetic factors significantly contribute to the risk, environmental, neurobiological, and psychosocial factors also play crucial roles in the development of schizophrenia.
Q: Can poor parenting or a dysfunctional family environment cause schizophrenia?
A: No. Early theories wrongly blamed family dynamics for schizophrenia. Modern research shows that while stress and social factors can exacerbate symptoms, they do not directly cause the disorder.
Q: Does the dopamine hypothesis explain all symptoms of schizophrenia?
A: Not entirely. While dopamine dysregulation is a key aspect, other neurotransmitter systems such as glutamate, as well as structural brain abnormalities, contribute to the disorder’s complexity.
Q: Can schizophrenia be prevented?
A: Prevention is challenging due to its multifactorial nature. However, early intervention and reducing exposure to known risk factors—such as managing maternal health and mitigating childhood stress—can potentially delay or reduce symptom severity.
Q: Are current treatments effective?
A: Treatments like antipsychotic medications and cognitive therapies help manage symptoms, but they do not cure schizophrenia. Advances in our understanding of the etiology of schizophrenia continue to pave the way for more targeted and effective therapies.
Q: What role does inflammation play in schizophrenia?
A: Emerging research indicates that chronic, low-grade inflammation in the brain may contribute to the disorder. Elevated inflammatory markers have been observed in some patients, suggesting an immune component in its etiology.
Modern Relevance and Current Trends
The study of the etiology of schizophrenia is an ever-evolving field, with recent trends offering promising avenues for improved understanding and treatment.
Precision Medicine and Biomarkers
Researchers are increasingly focused on identifying biomarkers—measurable indicators of disease—that can predict the onset or progression of schizophrenia. Biomarkers may include:
- Genetic Variants: Specific gene mutations or polymorphisms that increase susceptibility.
- Neuroimaging Markers: Structural or functional brain changes observable through MRI or PET scans.
- Inflammatory Indicators: Levels of cytokines or other inflammatory markers that correlate with disease activity.
These advancements could revolutionize treatment by allowing for earlier diagnosis and more personalized interventions.
Advances in Neuroimaging
Modern neuroimaging techniques are shedding light on the complex brain changes associated with schizophrenia. Researchers are using:
- Functional MRI (fMRI): To track brain activity in real time, offering insights into how different brain regions communicate.
- Diffusion Tensor Imaging (DTI): To map the integrity of white matter tracts, which can be disrupted in schizophrenia.
- Positron Emission Tomography (PET): To study neurotransmitter activity, particularly in relation to the dopamine and glutamate systems.
The Role of Technology and Big Data
The integration of big data analytics and machine learning into psychiatric research is opening new doors. By analyzing large datasets from diverse populations, scientists are:
- Identifying Patterns: Uncovering subtle genetic and environmental interactions that might otherwise be overlooked.
- Predicting Outcomes: Developing predictive models that can forecast the risk of developing schizophrenia based on a combination of factors.
Global and Cultural Perspectives
The etiology of schizophrenia is also being studied in diverse cultural and socioeconomic contexts. Research across different populations is revealing:
- Variations in Incidence: How urbanicity, social stress, and cultural attitudes impact the prevalence and expression of schizophrenia.
- Tailored Interventions: The need for culturally sensitive treatment strategies that account for differing social determinants of health.
The Future of Schizophrenia Research
As our understanding deepens, several promising areas are emerging:
- Neurodevelopmental Interventions: Early childhood programs designed to support healthy brain development in at-risk populations.
- Immunomodulatory Treatments: Investigating drugs that target inflammation or immune dysregulation as adjunctive therapies.
- Epigenetic Therapies: Exploring ways to modify gene expression through environmental or pharmacological means.
These developments underscore that the field is moving toward a more nuanced and integrated model of the etiology of schizophrenia.
Conclusion
The journey to decipher the etiology of schizophrenia is far from over, but each discovery brings us closer to understanding this perplexing disorder. We have explored the multifactorial causes of schizophrenia—from genetics and neurobiology to prenatal influences, psychosocial factors, and emerging theories such as epigenetics and the gut-brain axis.
Key Takeaways:
- Multifactorial Nature: Schizophrenia arises from a complex interplay of genetic, neurobiological, environmental, and psychosocial factors.
- Importance of Early Intervention: Understanding the etiology paves the way for early diagnosis and targeted treatment, which can significantly improve outcomes.
- Ongoing Research: Advancements in neuroimaging, precision medicine, and big data analytics are reshaping our understanding and opening new avenues for intervention.
- Reducing Stigma: Dispelling myths and embracing a nuanced view of schizophrenia’s origins can help reduce the stigma and foster greater empathy and support.
By appreciating the rich tapestry of influences that contribute to schizophrenia, we not only gain scientific insights but also enhance our collective ability to support those affected by this challenging condition.
Call to Action
If you found this post informative, consider sharing it with friends, family, or anyone interested in mental health. For further reading, explore reputable sources such as the National Institute of Mental Health and recent publications in peer-reviewed journals. Your continued engagement helps spread awareness and contributes to a deeper understanding of the etiology of schizophrenia.
Additional Resources
- Books and Publications: Look for texts by experts in psychiatry and neuroscience for an in-depth understanding.
- Support Organizations: Groups like the Schizophrenia and Related Disorders Alliance of America (SARDAA) offer valuable information and community support.
- Online Courses: Many universities offer free or low-cost courses on mental health and neuroscience that can further your knowledge.
Final Thoughts
The etiology of schizophrenia is a testament to the complexity of human biology and the intricate interplay between our genes, brains, and environments. While we have made significant strides in unraveling its mysteries, the road ahead is filled with promise as innovative research continues to refine our understanding.
Remember, every piece of research, every clinical trial, and every breakthrough in neuroimaging contributes to a future where schizophrenia is not only better understood but also more effectively managed. As we advance, let us remain committed to compassion, scientific curiosity, and the relentless pursuit of knowledge.
Thank you for joining us on this comprehensive exploration. We invite you to leave your comments, ask questions, or share your insights below. Together, we can continue to build a more informed, empathetic, and supportive community for everyone touched by schizophrenia.
By exploring the multifaceted etiology of schizophrenia, we hope to empower you with the knowledge needed to understand this complex disorder and inspire further learning and dialogue. Stay curious, stay informed, and remember that every new discovery is a step toward better mental health for all.

 4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all
4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all


