Male Reproductive System
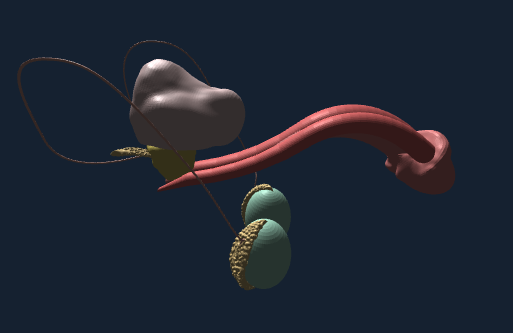
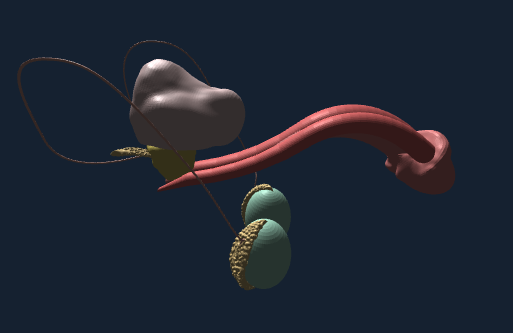
Male Reproductive System diagram
Male Reproductive System
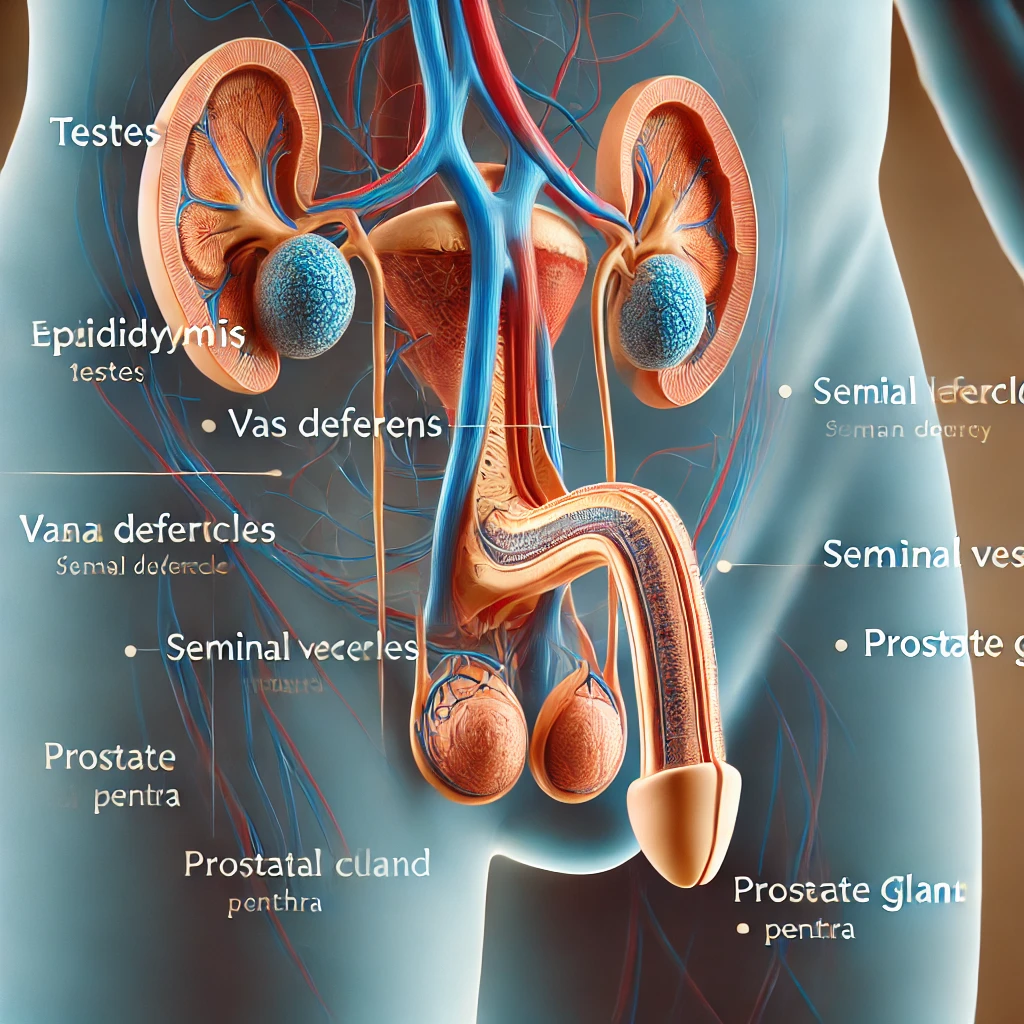
The male reproductive system is composed of several structures that work together to produce, mature, store, and transport sperm.
Below is a detailed, step-by-step explanation of each part and its function.
1. Testes in “Male Reproductive System”
- Location: The testes are located in the scrotum, a pouch of skin outside the abdominal cavity.
- Function: The primary function of the testes is to produce sperm (spermatogenesis) and secrete testosterone, the male sex hormone.
- Structure: Each testis contains seminiferous tubules where spermatogenesis occurs. Interstitial cells (Leydig cells) located between the tubules produce testosterone.
2. Epididymis in “Male Reproductive System”
- Location: The epididymis is a long, coiled tube attached to the back of each testis.
- Function: It stores and matures sperm. Sperm gain motility and the ability to fertilize an egg during their time in the epididymis.
3. Vas Deferens in “Male Reproductive System”
- Location: The vas deferens is a muscular tube that extends from the epididymis to the pelvic cavity.
- Function: It transports mature sperm from the epididymis to the urethra in preparation for ejaculation.
4. Ejaculatory Ducts in “Male Reproductive System”
- Location: Formed by the fusion of the vas deferens and the seminal vesicles, the ejaculatory ducts are located within the prostate gland.
- Function: They mix sperm with fluids from the seminal vesicles and transport the mixture to the urethra.
5. Urethra in “Male Reproductive System”
- Location: The urethra runs from the bladder through the penis.
- Function: It serves a dual purpose: it conveys both urine and semen (but not simultaneously) out of the body.
6. Accessory Glands in “Male Reproductive System”
These glands produce seminal fluid, which nourishes and protects sperm.
- Seminal Vesicles:
- Location: Behind the bladder.
- Function: Produce a viscous fluid rich in fructose, which provides energy for the sperm.
- Prostate Gland:
- Location: Below the bladder and surrounding the urethra.
- Function: Secretes a slightly alkaline fluid that helps to neutralize the acidic environment of the female reproductive tract.
- Bulbourethral Glands (Cowper’s Glands):
- Location: Below the prostate gland.
- Function: Produce a clear, slippery fluid that lubricates the urethra and neutralizes any acidity from residual urine.
7. Penis in “Male Reproductive System”
- Structure: The penis contains three columns of erectile tissue: two corpora cavernosa and one corpus spongiosum.
- Function: Delivers sperm into the female reproductive tract. During sexual arousal, the erectile tissues fill with blood, causing an erection.
Hormonal Regulation in “Male Reproductive System”
The male reproductive system is regulated by hormones from the hypothalamus, pituitary gland, and testes.
1. Hypothalamus
- Function: Releases gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland.
2. Pituitary Gland
- Function: Secretes two key hormones in response to GnRH:
- Luteinizing Hormone (LH): Stimulates Leydig cells in the testes to produce testosterone.
- Follicle-Stimulating Hormone (FSH): Works alongside testosterone to stimulate the production of sperm in the seminiferous tubules.
3. Testes
- Function: Produce testosterone, which is crucial for the development of male secondary sexual characteristics, spermatogenesis, and maintaining libido.
Spermatogenesis in “Male Reproductive System”
Spermatogenesis is the process of sperm production, which occurs in the seminiferous tubules of the testes.
- Spermatogonia: These are the diploid stem cells located in the seminiferous tubules. They undergo mitosis to produce primary spermatocytes.
- Primary Spermatocytes: These cells undergo the first meiotic division to form secondary spermatocytes.
- Secondary Spermatocytes: These cells undergo the second meiotic division to produce spermatids.
- Spermatids: These immature sperm cells undergo a series of changes (spermiogenesis) to become mature spermatozoa (sperm).
Sperm Structure in “Male Reproductive System”
- Head: Contains the nucleus with densely packed chromosomes and an acrosome, which contains enzymes that help the sperm penetrate the egg.
- Midpiece: Packed with mitochondria that provide the energy for the sperm to swim.
- Tail (Flagellum): Provides motility, enabling the sperm to swim towards the egg.
Testes (Male Reproductive System quiz)
- Q: What is the primary function of the testes?
- A: The primary function of the testes is to produce sperm and secrete testosterone.
- Q: Where are the testes located?
- A: The testes are located in the scrotum.
- Q: What structures within the testes produce sperm?
- A: Seminiferous tubules produce sperm.
- Q: Which cells in the testes produce testosterone?
- A: Leydig cells produce testosterone.
- Q: What is spermatogenesis?
- A: Spermatogenesis is the process of sperm production.
Epididymis
- Q: What is the function of the epididymis?
- A: The epididymis stores and matures sperm.
- Q: How does sperm change in the epididymis?
- A: Sperm gain motility and the ability to fertilize an egg.
- Q: Where is the epididymis located?
- A: The epididymis is attached to the back of each testis.
Vas Deferens
- Q: What is the function of the vas deferens?
- A: The vas deferens transports mature sperm to the urethra.
- Q: Where does the vas deferens extend from and to?
- A: It extends from the epididymis to the pelvic cavity.
Ejaculatory Ducts
- Q: How are the ejaculatory ducts formed?
- A: They are formed by the fusion of the vas deferens and the seminal vesicles.
- Q: What is the function of the ejaculatory ducts?
- A: They mix sperm with fluids from the seminal vesicles and transport the mixture to the urethra.
Urethra
- Q: What dual functions does the urethra serve in males?
- A: It conveys both urine and semen out of the body.
- Q: Where does the urethra run through?
- A: It runs from the bladder through the penis.
Accessory Glands
- Q: What are the three main accessory glands in the male reproductive system?
- A: Seminal vesicles, prostate gland, and bulbourethral glands.
- Q: What is the function of the seminal vesicles?
- A: They produce a viscous fluid rich in fructose that provides energy for sperm.
- Q: What is the role of the prostate gland?
- A: It secretes a slightly alkaline fluid that helps neutralize the acidic environment of the female reproductive tract.
- Q: What do the bulbourethral glands produce?
- A: They produce a clear, slippery fluid that lubricates the urethra and neutralizes any acidity from residual urine.
Penis
- Q: What is the primary function of the penis?
- A: It delivers sperm into the female reproductive tract.
- Q: What causes an erection?
- A: Erectile tissues fill with blood during sexual arousal.
Hormonal Regulation
- Q: What hormone does the hypothalamus release to regulate the male reproductive system?
- A: Gonadotropin-releasing hormone (GnRH).
- Q: What hormones are secreted by the pituitary gland in response to GnRH?
- A: Luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- Q: What is the function of LH in males?
- A: It stimulates Leydig cells to produce testosterone.
- Q: What is the role of FSH in males?
- A: It works with testosterone to stimulate the production of sperm.
Spermatogenesis
- Q: Where does spermatogenesis occur?
- A: In the seminiferous tubules of the testes.
- Q: What are spermatogonia?
- A: Diploid stem cells that undergo mitosis to produce primary spermatocytes.
- Q: What do primary spermatocytes undergo to form secondary spermatocytes?
- A: The first meiotic division.
- Q: What do secondary spermatocytes undergo to produce spermatids?
- A: The second meiotic division.
- Q: What process do spermatids undergo to become mature sperm?
- A: Spermiogenesis.
Sperm Structure
- Q: What is contained in the head of the sperm?
- A: The nucleus with densely packed chromosomes and an acrosome.
- Q: What is the function of the acrosome?
- A: It contains enzymes that help the sperm penetrate the egg.
- Q: What does the midpiece of the sperm contain?
- A: Mitochondria that provide energy for the sperm to swim.
- Q: What is the function of the sperm’s tail (flagellum)?
- A: It provides motility, enabling the sperm to swim towards the egg.
Additional Questions
Testes
- Q: What type of cells are found within the seminiferous tubules?
- A: Sertoli cells, which support and nourish developing sperm cells.
- Q: What is the blood-testis barrier?
- A: A physical barrier formed by Sertoli cells that protects developing sperm from the immune system.
Epididymis
- Q: How long does it typically take for sperm to travel through the epididymis?
- A: About 2 to 3 weeks.
- Q: What role does the epididymis play in sperm maturation?
- A: It provides an environment for sperm to gain motility and the ability to fertilize an egg.
Vas Deferens
- Q: What happens during a vasectomy?
- A: The vas deferens is cut and sealed to prevent sperm from reaching the urethra.
Ejaculatory Ducts
- Q: How long are the ejaculatory ducts?
- A: They are about 2 cm in length.
- Q: What fluid contributes to the ejaculate from the seminal vesicles?
- A: A fluid rich in fructose, which provides energy for the sperm.
Urethra
- Q: How is the flow of urine and semen controlled in the urethra?
- A: By the internal and external urethral sphincters.
Accessory Glands
- Q: What percentage of semen volume is contributed by the seminal vesicles?
- A: About 60-70%.
- Q: What enzyme in the prostate fluid helps liquefy semen?
- A: Prostate-specific antigen (PSA).
Penis
- Q: What are the two main parts of the penis?
- A: The shaft and the glans.
- Q: What is the prepuce?
- A: The foreskin, a fold of skin covering the glans.
Hormonal Regulation (Male Reproductive System quiz)
- Q: What is the role of testosterone in male development?
- A: It promotes the development of male secondary sexual characteristics and maintains reproductive tissues.
- Q: How does testosterone affect spermatogenesis?
- A: It is essential for the maintenance of spermatogenesis.
Spermatogenesis
- Q: How many sperm are produced from each primary spermatocyte?
- A: Four haploid sperm cells.
- Q: What is the duration of the spermatogenesis process?
- A: Approximately 64 days.
Sperm Structure
- Q: What is the function of the acrosomal reaction?
- A: It releases enzymes that help the sperm penetrate the egg’s outer layers.
Additional Questions on Functions and Processes (Male Reproductive System)
- Q: What is the primary function of Sertoli cells?
- A: To support and nourish developing sperm cells.
- Q: What is the main function of the scrotum?
- A: To regulate the temperature of the testes for optimal spermatogenesis.
- Q: What is the significance of the blood-testis barrier?
- A: It prevents immune cells from attacking developing sperm cells.
- Q: What role do Leydig cells play in the male reproductive system?
- A: They produce and secrete testosterone.
- Q: How do sperm gain motility?
- A: They gain motility during their passage through the epididymis.
Diseases and Disorders (Male Reproductive System)
- Q: What is cryptorchidism?
- A: A condition where one or both testes fail to descend into the scrotum.
- Q: What is benign prostatic hyperplasia (BPH)?
- A: A noncancerous enlargement of the prostate gland.
- Q: What is the most common cancer in young men aged 15-35?
- A: Testicular cancer.
- Q: What is prostatitis?
- A: Inflammation of the prostate gland.
- Q: What is erectile dysfunction?
- A: The inability to achieve or maintain an erection sufficient for satisfactory sexual performance.
Spermatogenesis Details
- Q: What hormones regulate spermatogenesis?
- A: FSH, LH, and testosterone.
- Q: What is the role of the hypothalamus in spermatogenesis?
- A: It releases GnRH, which stimulates the pituitary gland to secrete FSH and LH.
- Q: How does FSH influence spermatogenesis?
- A: It stimulates Sertoli cells to support sperm production.
- Q: How does LH influence spermatogenesis?
- A: It stimulates Leydig cells to produce testosterone.
Hormonal Control
- Q: What feedback mechanism regulates testosterone levels?
- A: Negative feedback on the hypothalamus and pituitary gland.
- Q: What happens to GnRH, FSH, and LH levels when testosterone levels are high?
- A: They decrease.
Seminal Fluid
- Q: What components are found in seminal fluid?
- A: Fructose, proteins, enzymes, and alkaline substances.
- Q: What is the function of fructose in seminal fluid?
- A: To provide energy for sperm motility.
- Q: How does the alkaline nature of seminal fluid benefit sperm?
- A: It neutralizes the acidic environment of the female reproductive tract.
Accessory Glands
- Q: What is the role of the bulbourethral glands during ejaculation?
- A: To secrete a pre-ejaculate fluid that lubricates the urethra.
- Q: How does prostate fluid contribute to semen?
- A: It contains enzymes and substances that enhance sperm motility and survival.
Erection and Ejaculation (Male Reproductive System)
- Q: What causes an erection?
- A: Increased blood flow to the erectile tissues of the penis.
- Q: What triggers ejaculation?
- A: Rhythmic contractions of the pelvic muscles and the reproductive ducts.
- Q: What is the refractory period?
- A: A period of time after ejaculation during which a man is unable to achieve another erection.
Hormonal Effects
- Q: What are secondary sexual characteristics in males?
- A: Features such as facial hair, deep voice, and increased muscle mass influenced by testosterone.
- Q: How does testosterone affect the male brain?
- A: It influences libido and aggression.
Fertility
- Q: What is the average sperm count in a healthy male?
- A: About 15 million to over 200 million sperm per milliliter of semen.
- Q: What is azoospermia?
- A: A condition characterized by the absence of sperm in semen.
- Q: How can lifestyle affect male fertility?
- A: Factors such as smoking, alcohol consumption, and stress can reduce sperm count and motility.
Anatomy
- Q: What are the primary structures of the male external genitalia?
- A: The penis and scrotum.
- Q: What is the role of the glans penis?
- A: It is the sensitive tip of the penis that plays a key role in sexual arousal.
Physiology
- Q: How does the scrotum regulate testicular temperature?
- A: Through contraction and relaxation of the cremaster muscle.
- Q: What is the average temperature difference between the testes and the rest of the body?
- A: The testes are typically about 2-3 degrees Celsius cooler than the body.
Pathophysiology
- Q: What is testicular torsion?
- A: A medical emergency where the spermatic cord twists, cutting off blood supply to the testis.
- Q: What is the most common symptom of testicular cancer?
- A: A painless lump or swelling in the testis.
Genetic and Developmental Aspects (Male Reproductive System)
- Q: What gene is crucial for the development of male characteristics?
- A: The SRY gene on the Y chromosome.
- Q: What role does dihydrotestosterone (DHT) play in male development?
- A: It is essential for the development of male external genitalia.
Endocrine Interactions
- Q: What is the role of inhibin in male reproduction?
- A: It inhibits FSH production to regulate spermatogenesis.
- Q: How does the male reproductive system respond to exogenous testosterone?
- A: It can lead to reduced endogenous testosterone production and spermatogenesis.
Clinical Interventions
- Q: What is the purpose of hormone replacement therapy (HRT) in males?
- A: To treat low testosterone levels.
- Q: What is the function of the vasectomy reversal procedure?
- A: To restore fertility by reconnecting the vas deferens.
Molecular Biology
- Q: What is the function of protamines in sperm?
- A: They replace histones to tightly pack DNA in the sperm head.
- Q: What is capacitation?
- A: A physiological change sperm undergo to gain the ability to penetrate and fertilize an egg.
Immunology
- Q: Why is the blood-testis barrier important?
- A: It protects sperm from autoimmune attacks.
Biochemistry
- Q: What enzymes are involved in the acrosome reaction?
- A: Acrosin and hyaluronidase.
Behavioral Aspects
- Q: How does testosterone influence male behavior?
- A: It can increase aggression and libido.
Comparative Anatomy
- Q: How do male reproductive systems differ among vertebrates?
- A: Differences exist in structure, function, and reproductive strategies.
Evolutionary Biology
- Q: What evolutionary advantage does external testis placement provide?
- A: Cooler temperatures favor optimal spermatogenesis.
Experimental Techniques
- Q: How is male fertility assessed in a laboratory setting?
- A: Through semen analysis evaluating sperm count, motility, and morphology.
- Q: What is the purpose of a testicular biopsy? – A: To diagnose conditions affecting spermatogenesis and testicular function.