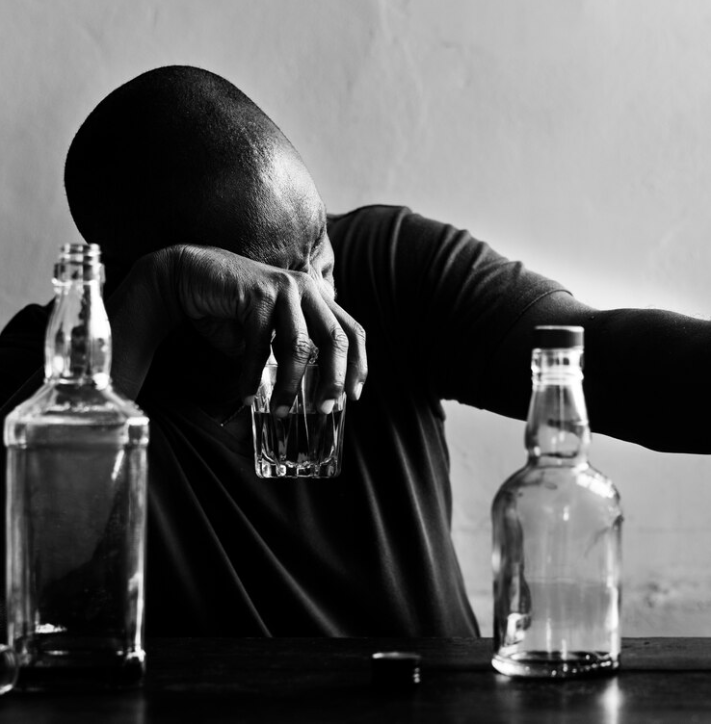
The Relationship Between Alcohol and Depression
What is Depression?
Depression is a common mental health condition characterized by prolonged feelings of sadness, hopelessness, and a lack of interest in daily activities. Depression can significantly impact how you feel, think, and function, making it challenging to manage your day-to-day responsibilities. Symptoms can range from mild to severe and often require intervention to improve.[1]
Symptoms of Depression
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness, worthlessness, or pessimism
- Irritability or restlessness
- Loss of interest in previously enjoyed activities
- Fatigue or decreased energy
- Difficulty concentrating, making decisions, or remembering details
- Significant changes in appetite or weight
- Sleep disturbances, including insomnia or oversleeping
- Physical symptoms such as chronic pain, headaches, or digestive issues
- Suicidal thoughts, ideation, or attempts[2]
Depression can be influenced by a range of genetic, biological, psychological, and environmental factors. Treatment often involves therapy, medication, or a combination of both.[3]
Clinical vs. Non-Clinical Depression
Clinical Depression refers to a form of depression that meets specific diagnostic criteria, such as Major Depressive Disorder (MDD) as defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM). Symptoms must persist for at least two weeks and significantly impair one’s ability to function.[4]
Non-Clinical Depression may describe feelings of sadness or low mood that do not meet the full criteria for a clinical diagnosis. While non-clinical depression may not cause as much disruption to daily life, it can still be distressing and should be taken seriously. Non-clinical depression may evolve into a more severe condition if not addressed.[5]
What is Alcohol Use Disorder?
Alcohol Use Disorder (AUD) is a chronic and often relapsing condition characterized by an inability to control alcohol consumption despite negative consequences. This condition can affect your physical, emotional, and social well-being and can range in severity from mild to severe.
Key Features of AUD
- Compulsive Alcohol Use: Persistent cravings and an inability to limit drinking despite harmful consequences.
- Loss of Control: Difficulty stopping or controlling alcohol intake once drinking begins.
- Dependence: Physical dependence occurs when the body becomes accustomed to alcohol, leading to withdrawal symptoms if intake is reduced.
- Tolerance: Needing increasing amounts of alcohol to achieve the same effect.
- Negative Emotional States: Experiencing anxiety, depression, or irritability when not drinking.
- Impact on Life: AUD can affect health, relationships, work, and finances and may lead to legal problems.[6]
AUD is diagnosed based on criteria outlined in the DSM and is classified as mild, moderate, or severe depending on the number of symptoms experienced.[6]
When Does Alcohol Use Become Problematic?
Alcohol use becomes problematic when it negatively affects aspects of life such as health, relationships, work, or daily functioning. Indicators of problematic alcohol use include frequent intoxication, physical dependence, withdrawal symptoms, and the inability to reduce or control drinking.[7]
How Are Depression and Alcohol Use Related?
The relationship between depression and alcohol use is complex and bidirectional. People with depression may use alcohol as a coping mechanism to temporarily alleviate symptoms like sadness or anxiety. However, alcohol often exacerbates these feelings, creating a vicious cycle where alcohol worsens depression and vice versa.[8]
Biological Connections
Both conditions affect neurotransmitters such as serotonin and dopamine, which regulate mood and reward. Alcohol disrupts these systems, worsening mood disorders like depression.[9]
Impaired Judgment and Increased Risk
Alcohol can impair judgment and increase impulsivity, potentially leading to risky behaviors. Depression can exacerbate these effects, increasing the likelihood of excessive alcohol use or addiction. Both conditions are risk factors for suicidal thoughts and behaviors, and addressing them concurrently is essential for effective treatment.[10]
The Need for Integrated Treatment
Integrated treatment approaches that address both depression and alcohol use disorders, such as therapy and medications, can be beneficial. Professional intervention from addiction specialists or mental health professionals is crucial for managing these conditions.[10]
Steps to Take if You Need Help with Depression and Alcohol Use
1. Reach Out for Support
Talk to trusted friends, family, or a mental health professional. Building a support network can provide encouragement and reduce feelings of isolation.
2. Seek Professional Help
Consult with a healthcare provider to assess your situation. If necessary, managed withdrawal from alcohol in a medical setting may be recommended for safety.
3. Explore Therapy Options
Therapies like Cognitive Behavioral Therapy (CBT) can help address both depression and alcohol use by changing thought patterns and behaviors.
4. Medication Management
Antidepressants or medications to reduce cravings for alcohol may be recommended. Always follow your provider’s guidance.
5. Consider Inpatient Treatment
Residential treatment programs offer intensive support for co-occurring conditions in a structured environment, combining therapy, medical care, and holistic approaches.
6. Engage in Aftercare Programs
After initial treatment, ongoing support through outpatient therapy, support groups, and aftercare programs can help maintain progress and prevent relapse.
Recovery is a journey, and setbacks are normal. Stay patient, stay committed, and lean on your support network.