Understanding Congenital Heart Disease: Types, Symptoms, Causes, and Outlook
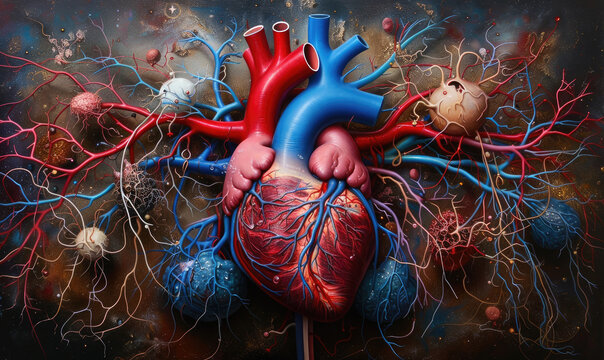
Congenital heart disease (CHD) refers to a wide range of structural defects in the heart that are present at birth. These defects can vary in severity and complexity, affecting the way blood flows through the heart and the rest of the body. While some cases may be mild, others may require immediate surgical intervention after birth or ongoing medical management throughout a person’s life.
Types of Congenital Heart Disease
There are over 30 different types of congenital heart defects, but they generally fall into two main categories:
1. Cyanotic Heart Disease
- Description: Cyanotic heart disease occurs when the heart’s structure leads to low levels of oxygen in the blood. This can happen due to issues such as defects in the heart valves, holes between heart chambers, or abnormal connections between major blood vessels.
- Symptoms: Babies with cyanotic heart disease often exhibit a bluish tint to their skin, lips, fingers, and toes (cyanosis) due to a lack of oxygen-rich blood. Other symptoms include:
- Breathlessness
- Chest pain
- Palpitations (irregular or rapid heartbeats)
- Fainting episodes
- Fatigue and lethargy
- Common Conditions: Examples include Tetralogy of Fallot, Transposition of the Great Arteries, and Truncus Arteriosus.
2. Acyanotic Heart Disease
- Description: In acyanotic heart disease, the blood contains sufficient oxygen but circulates abnormally within the body due to structural defects in the heart. While these conditions may not cause noticeable cyanosis, they can place excessive pressure on the heart and blood vessels.
- Symptoms: Babies born with acyanotic heart disease may not exhibit symptoms initially. However, over time, symptoms can manifest as the condition progresses, including:
- Increased blood pressure in the lungs (pulmonary hypertension)
- Breathlessness, especially during physical activity
- Fatigue and exhaustion
- Dizziness and light-headedness
- Risk of heart failure if the heart becomes too weak to pump blood efficiently
- Common Conditions: Examples include Ventricular Septal Defect (VSD), Atrial Septal Defect (ASD), and Patent Ductus Arteriosus (PDA).
How Common is Congenital Heart Disease?
Congenital heart disease is the most prevalent type of birth defect, occurring in approximately 1 in 180 live births. The causes of CHD are multifactorial and may include genetic factors, environmental influences, and unknown causes. Notably, certain conditions such as Down syndrome are often associated with a higher incidence of congenital heart defects.
Causes and Risk Factors of Congenital Heart Disease
While the exact cause of many congenital heart defects remains unclear, some known risk factors and potential causes include:
- Genetic Conditions: CHD is more common in babies with chromosomal abnormalities such as Down syndrome or Turner syndrome.
- Maternal Infections: Certain infections during pregnancy, such as rubella, can contribute to the development of congenital heart defects.
- Maternal Health Conditions: Conditions such as diabetes and obesity during pregnancy can increase the risk of CHD.
- Family History: A family history of heart defects may increase the risk of congenital heart disease in children.
- Environmental Factors: Exposure to certain medications, alcohol, or toxic substances during pregnancy may play a role in the development of heart defects.
Diagnosis and Treatment of Congenital Heart Disease
Diagnosis of congenital heart disease typically involves:
- Prenatal Ultrasound: Many defects can be detected before birth during routine prenatal scans.
- Echocardiography: This non-invasive imaging test uses sound waves to create images of the heart’s structure and blood flow.
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and can help detect irregular heart rhythms.
- Other Imaging Tests: In some cases, MRI or CT scans may be used to provide detailed images of the heart.
Treatment for congenital heart disease depends on the type and severity of the defect:
- Medication: Certain medications can help manage symptoms, improve heart function, and prevent complications such as blood clots.
- Surgery: Many children with CHD require surgical interventions, ranging from minimally invasive procedures to complex open-heart surgeries.
- Catheter-Based Procedures: These minimally invasive procedures use a catheter to repair certain heart defects without the need for open surgery.
- Ongoing Monitoring: Children and adults with CHD may need regular follow-ups with a cardiologist to monitor their heart health.
Long-Term Outlook for Congenital Heart Disease
The outlook for individuals with congenital heart disease has improved significantly due to advances in medical and surgical care. Approximately 80% of children born with CHD now survive into adulthood. This has led to the development of specialized centers focused on providing lifelong care for adults with congenital heart disease, known as “grown-up congenital heart disease” (GUCH) or Adult Congenital Heart Disease (ACHD).
Challenges for Adults with CHD:
- Adults living with CHD may face unique challenges, including complex heart conditions, arrhythmias, and complications related to their previous surgeries or treatments.
- Lifelong care and regular follow-ups with specialists are essential to manage these potential complications and maintain heart health.
Living with Congenital Heart Disease
Living with congenital heart disease can be challenging, but with appropriate care, many individuals lead fulfilling lives. Support networks, specialized care, and advances in treatment options continue to improve the quality of life for those affected by CHD.
Symptoms of Cyanotic Heart Disease
Cyanotic heart disease occurs when there is insufficient oxygen in the blood. This leads to a distinctive bluish tint on the skin and mucous membranes due to reduced oxygen levels, a condition known as cyanosis. Key symptoms of cyanotic heart disease include:
- Cyanosis (Blue Tinge to Lips, Fingers, and Toes)
- One of the hallmark signs of cyanotic heart disease, cyanosis results from a lack of adequate oxygen in the bloodstream. This often manifests as a blue or purplish hue on the lips, fingertips, and toes, especially during physical exertion.
- Palpitations
- Patients may experience irregular or unusually fast heartbeats, creating a sensation of pounding or fluttering in the chest. This can contribute to feelings of discomfort and anxiety.
- Fainting (Syncope)
- Sudden fainting spells can occur due to inadequate oxygen supply to the brain. This symptom often arises during physical activity or moments of exertion.
- Fatigue
- A persistent sense of tiredness or exhaustion, even after minimal physical exertion, is common due to the heart’s reduced efficiency in oxygenating the body.
- Chest Pain
- Discomfort or pain in the chest can arise from the heart working harder to pump blood through narrowed or abnormal pathways.
- Breathing Problems
- Breathlessness, wheezing, or labored breathing is common due to decreased oxygenation. It can become more pronounced during physical activities or even at rest.
Additional Symptoms Linked to Hypoxia:
In severe cases, oxygen levels can drop even further, leading to symptoms such as:
- Anxiety: A sense of unease or fear may result from low oxygen levels.
- Confusion or Disorientation: Reduced oxygen supply to the brain can cause cognitive disturbances.
Symptoms of Acyanotic Heart Disease
Acyanotic heart disease involves defects where oxygenated blood is circulated abnormally around the body. Unlike cyanotic conditions, there is typically no cyanosis, but this form of CHD can still lead to serious complications over time. Symptoms include:
- Severe Tiredness (Fatigue)
- Persistent tiredness and a lack of energy, even with light activity, are common due to the heart’s increased workload.
- Palpitations
- Irregular or rapid heartbeats can occur, creating discomfort or distress for patients.
- Chest Pain
- This may be present due to increased strain on the heart muscles as they work harder to pump blood throughout the body.
- Shortness of Breath (Dyspnea)
- Difficulty breathing or catching one’s breath, especially during physical exertion like climbing stairs or engaging in routine tasks, is a frequent symptom.
Common Symptoms Shared by Both Cyanotic and Acyanotic Heart Disease
Some symptoms are common to both types of congenital heart disease and reflect the heart’s overall difficulty in functioning properly. These include:
- Poor Appetite and Feeding Difficulties
- Babies and young children with CHD often struggle to feed effectively. Feeding may be tiring for them due to labored breathing or poor circulation, leading to prolonged feeding times and less food intake.
- Excessive Sweating (Especially While Feeding)
- Sweating during feeding or other minor exertions is a sign that the heart is under strain as it works harder than normal.
- Delayed Growth and Development
- Children with CHD may experience slower growth rates and fail to meet typical developmental milestones. This is often due to a combination of feeding difficulties, poor nutrition, and the body’s increased energy expenditure.
Weight Concerns:
- Children with Acyanotic Heart Disease: They are often underweight due to poor appetite and difficulty feeding.
- Children with Cyanotic Heart Disease: They tend to be both underweight and smaller for their age because of chronic low oxygen levels impacting growth and development.
What Causes Congenital Heart Disease?
CHD occurs when there are structural abnormalities in the heart that prevent it from functioning correctly. It typically forms during fetal development, and while the exact cause of many cases remains unknown, several factors and conditions can increase the risk of CHD.
Common Types of Congenital Heart Disease
1. Cyanotic Heart Disease
This form of CHD occurs when blood contains insufficient oxygen, leading to symptoms such as cyanosis (a bluish tint to the skin).
- Symptoms: Cyanotic heart disease often results in blue-colored lips, fingers, and toes due to low oxygen levels. Other symptoms may include breathlessness, chest pain, fatigue, palpitations, and fainting.
2. Acyanotic Heart Disease
In acyanotic heart disease, oxygen levels are normal, but blood flow within the heart is abnormal, placing strain on the heart and increasing blood pressure.
- Symptoms: This can lead to breathlessness, fatigue, chest pain, and pulmonary hypertension (high blood pressure in the lungs).
Specific Conditions Leading to CHD
Acyanotic Heart Conditions
Ventricular Septal Defect (VSD)
VSD is a common acyanotic defect involving a hole between the left and right ventricles. This allows blood to flow from the left side to the right side due to higher pressure on the left. This can strain the heart and increase blood pressure in the lungs (pulmonary hypertension).Atrial Septal Defect (ASD)
Similar to VSD but involving a hole between the left and right atria, ASD places strain on the heart and lungs over time. This condition is often referred to as a “hole in the heart.”Pulmonary Stenosis
Pulmonary stenosis involves a narrowing of the pulmonary valve, causing the heart to work harder to pump blood into the lungs.Aortic Stenosis
Here, the aortic valve narrows, limiting the flow of oxygen-rich blood throughout the body and leading to symptoms such as breathlessness and dizziness.Patent Ductus Arteriosus (PDA)
This is a duct that remains open after birth, allowing oxygen-rich blood to leak back into the lungs. This places excess strain on the heart and lungs.
Cyanotic Heart Conditions
Tetralogy of Fallot (TOF)
TOF involves four different heart defects: a ventricular septal defect, pulmonary stenosis, thickened right ventricle (right ventricular hypertrophy), and an overriding aorta. Together, these defects cause oxygen-low blood to be pumped around the body.Transposition of the Great Arteries (TGA)
In this condition, the pulmonary artery and the aorta are incorrectly attached, leading to oxygen-poor blood being circulated through the body, causing cyanotic symptoms.
Risk Factors for Congenital Heart Disease
1. Maternal Diabetes
Women with diabetes are five times more likely to have a baby with congenital heart defects, likely due to high levels of insulin impacting fetal development.
2. Rubella Infection
Contracting rubella during the first trimester of pregnancy poses an 80% risk of the baby being born with birth defects, including CHD.
3. Maternal Alcohol Use
Alcohol consumption during pregnancy significantly increases the risk of CHD in newborns. It is best to avoid alcohol entirely during pregnancy.
4. Genetic Conditions
Several genetic syndromes are linked to CHD, including:
- Down’s Syndrome: Approximately 50% of children with Down’s syndrome have congenital heart defects.
- Turner Syndrome and Noonan Syndrome: Both conditions are known to cause structural heart abnormalities.
Diagnosing Congenital Heart Disease
Diagnosing congenital heart disease (CHD) is critical to providing timely treatment and ensuring optimal outcomes for affected individuals. Detection can occur during pregnancy or postnatally, depending on the severity and type of defect.
Prenatal Diagnosis
Foetal Echocardiography
A foetal echocardiogram is an advanced ultrasound test that provides detailed images of an unborn baby’s heart. Conducted between the 18th and 20th week of pregnancy, this test offers a chance to detect congenital heart defects early, allowing for proactive planning and care. However, mild heart defects can be challenging to spot using this method.
Why It Matters:
Early diagnosis through foetal echocardiography enables parents and healthcare teams to plan and implement immediate care strategies once the baby is born.
Postnatal Diagnosis
Immediate Signs of CHD
For babies born with cyanotic heart disease, diagnosis is often straightforward due to the characteristic bluish tint to their skin, caused by low oxygen levels. In contrast, acyanotic heart disease may not present symptoms until months or even years after birth.
Symptoms to Watch For in Children:
- Difficulty feeding
- Slow growth or failure to thrive
- Shortness of breath, especially during activities
- Fatigue after exertion
- Swelling in hands, feet, or ankles
Parental Action:
If you notice any of these symptoms in your child, contact your GP for an evaluation. Timely detection and intervention are crucial for managing CHD effectively.
Further Diagnostic Testing for Congenital Heart Disease
1. Echocardiogram (Echo)
This test uses ultrasound waves to produce images of the heart. Echocardiograms can detect underlying heart issues that may have been missed during prenatal scans, offering a non-invasive view of heart function and structure.
Learn More: Visit the British Heart Foundation website for additional details on echocardiograms.
2. Electrocardiogram (ECG)
An ECG measures the heart’s electrical activity using electrodes placed on the chest, arms, and legs. This test helps assess heart rhythm and can identify abnormalities associated with CHD.
Learn More: More about ECGs can be found on the British Heart Foundation website.
3. Chest X-ray
A chest X-ray provides a detailed view of the heart and lungs. It helps detect abnormalities such as an enlarged heart or issues with the lungs that may be related to CHD.
Learn More: Explore more about chest X-rays at the British Heart Foundation.
4. Pulse Oximetry
This non-invasive test measures blood oxygen levels using a sensor placed on the fingertip, ear, or toe. Low oxygen readings (below 94%) are common in children with cyanotic heart defects.
5. Cardiac Catheterisation
A catheterisation procedure involves inserting a small flexible tube into a blood vessel, usually in the groin or arm, to examine heart function. Contrast dye is used to visualize the flow of blood and assess heart chambers. Blood pressure measurements taken during this procedure provide essential information for diagnosis and treatment planning.
- Procedure Details: Cardiac catheterisation is typically performed under local anaesthesia and is relatively painless.
Why Accurate Diagnosis Matters
Proper diagnosis of congenital heart disease allows for tailored treatment plans, ensuring the best possible outcomes for affected children. From minimally invasive procedures to complex surgeries, accurate diagnostic information helps healthcare professionals provide life-changing care.
Treating Congenital Heart Disease
Congenital heart disease (CHD) encompasses a wide range of structural defects present at birth. Treatment options depend on the severity, type of defect, and the age of the patient. Here’s a detailed guide on available treatments and management strategies for congenital heart disease.
Surgical Techniques for Treating CHD
1. Catheter-Based Procedures
This minimally invasive technique involves inserting a catheter (a thin flexible tube) into the heart. Tools are passed through the catheter to repair defects, offering the advantage of avoiding open-heart surgery. This approach typically involves a shorter recovery period and fewer complications than traditional surgery.
Common Uses:
- Sealing holes in the heart (e.g., atrial septal defect)
- Widening narrow heart valves using balloon angioplasty
- Inserting metal coils or plugs to close abnormal blood vessels
2. Open-Heart Surgery
For complex heart defects, open-heart surgery is necessary. Surgeons operate directly on the heart to repair structural issues. During the procedure, the heart may be temporarily stopped, and a bypass machine is used to maintain blood circulation.
Typical Procedures:
- Repairing or replacing damaged valves
- Sealing holes between heart chambers
- Reconstructing heart structures
3. Heart Transplant
In severe cases where the heart is too damaged to be repaired, a heart transplant may be required. The patient is placed on a waiting list for a suitable donor heart. Machines, such as ventricular assist devices (VADs), may support heart function while waiting for a transplant.
Specific Treatments for Common CHD Types
1. Septal Defects (e.g., Ventricular/Atrial Septal Defect)
- Small Defects: Often resolve on their own; monitored closely by healthcare providers (watchful waiting).
- Medium/Large Defects: Catheter-based closure using specially designed mesh or patches; open-heart surgery for direct patch placement.
2. Stenosis (Narrowed Heart Valves)
- Mild Cases: Monitoring and possibly medication to lower blood pressure and reduce heart strain.
- Severe Cases: Balloon angioplasty or open-heart surgery to widen or replace valves using human, artificial, or modified animal valves.
3. Patent Ductus Arteriosus (PDA)
- Medications: Indomethacin or ibuprofen to stimulate duct closure shortly after birth.
- Catheter Procedure: Sealing the duct with a coil or plug if medication is ineffective.
4. Tetralogy of Fallot (TOF)
- Emergency Surgery: Blalock-Taussig shunt for severe breathlessness to increase blood oxygen.
- Open-Heart Surgery: Repairing the ventricular defect and widening the pulmonary valve.
5. Transposition of the Great Arteries (TGA)
- Surgery: Arterial switch procedure shortly after birth to correct the positioning of arteries for proper blood flow.
CHD Management in Adulthood
With advancements in CHD treatment, around 80% of affected children survive into adulthood. Managing congenital heart disease as an adult comes with unique challenges, such as monitoring the functionality of repaired or replaced heart structures and managing routine medical procedures like childbirth or anesthesia under specialized care.
Recommendations for Adults:
- Register with specialized adult congenital heart disease clinics.
- Receive regular check-ups and assessments.
- Coordinate care with specialists for any medical interventions.
Congenital Heart Disease Complications
Congenital heart disease (CHD) can lead to a variety of complications, impacting different aspects of a child’s health and development. Understanding these complications is crucial to provide appropriate care and support.
Developmental Delays and Learning Difficulties
Children with CHD often face developmental challenges. The condition may delay key milestones, such as walking, talking, and social interactions. This is because their heart’s reduced efficiency in pumping oxygen-rich blood can affect physical stamina, brain function, and growth. Some common developmental issues include:
- Delayed Motor Skills: Difficulty achieving typical milestones such as crawling, walking, and running.
- Cognitive and Learning Difficulties: Challenges with memory, attention, and learning can manifest, often necessitating individualized educational strategies.
- Psychological and Emotional Support Needs: CHD may also impact a child’s emotional well-being due to hospitalizations and physical limitations.
Individual Education Plans (IEP) for Children with CHD:
- Assessment: The local educational authority should perform a detailed assessment to understand the child’s specific needs.
- Tailored Services: Services may include speech and language therapy, occupational therapy, and access to educational psychologists.
- Activity Modifications: Physical activity recommendations are based on the child’s unique condition. While children with CHD are encouraged to stay active, contact sports or strenuous activities may need to be avoided.
Increased Risk of Endocarditis
What is Endocarditis?
Endocarditis is a serious infection that affects the inner lining of the heart, particularly its valves. It occurs when bacteria or other pathogens from another part of the body, such as the mouth or skin, travel through the bloodstream and attach to the heart’s damaged areas or valves.
Symptoms of Endocarditis:
- Persistent fever and chills
- Night sweats
- Muscle and joint pain
- Chest pain and coughing
- Weakness and fatigue
- Shortness of breath
- Headaches
Treatment for Endocarditis:
- Hospitalization and Antibiotic Therapy: Patients typically require a hospital stay for several weeks to receive intravenous antibiotics to clear the infection. In severe cases, surgery may be necessary to repair damaged heart valves.
Prevention Tips for People with CHD:
- Practice Excellent Oral Hygiene: Gum disease can increase the risk of endocarditis. Regular brushing, flossing, and routine dental check-ups are essential.
- Avoid Certain Procedures: Cosmetic procedures involving skin piercings or tattoos should generally be avoided due to the increased risk of infections that could lead to endocarditis.
- Be Aware of Symptoms: Recognizing the early signs of endocarditis and seeking prompt medical care can significantly reduce the risk of severe complications.
Managing Physical Activity and Lifestyle
Balancing Activity Levels:
Children with CHD can often participate in various physical activities, which can enhance their physical and emotional well-being. However, the level and type of activity should be guided by a healthcare professional:
- Moderate Activities: Walking, swimming, or gentle sports can often be beneficial.
- Avoid High-Impact Sports: Contact sports or activities with a high risk of collision may not be recommended due to the increased strain they can place on the heart.
Social and Emotional Support:
Living with CHD can impact a child’s social interactions and emotional health. Support groups, counseling, and community-based activities can play a vital role in providing encouragement and fostering positive mental health.