Crohn’s Disease
Below is a comprehensive, structured report on Crohn’s Disease. This detailed overview covers essential aspects—from its definition and history to symptoms, causes, risk factors, complications, diagnostic procedures, treatment options, prevention strategies, global statistics, and future research directions. The report is designed to be accessible to both the general public and healthcare professionals.
1. Overview
What is Crohn’s Disease?
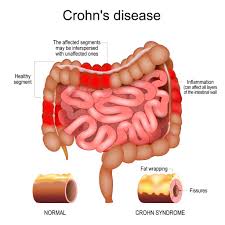
Crohn’s disease is a chronic inflammatory bowel disease (IBD) characterized by inflammation of the gastrointestinal tract. It can affect any part of the digestive system, from the mouth to the anus, though it most commonly involves the terminal ileum and the beginning of the colon.
Concise yet Detailed Definition
Crohn’s disease is an idiopathic, relapsing-remitting inflammatory condition marked by transmural inflammation of the gastrointestinal tract. Unlike ulcerative colitis, which is limited to the colon and rectum, Crohn’s disease can involve multiple, discontinuous segments of the digestive tract, leading to complications such as strictures, fistulas, and abscesses.
Affected Body Parts/Organs
- Gastrointestinal Tract: Can affect the entire digestive system, with a predilection for the terminal ileum, colon, and perianal region.
- Transmural Involvement: Inflammation extends through the full thickness of the bowel wall, which distinguishes it from other forms of IBD.
- Extra-Intestinal Sites: Can also involve the eyes, skin, joints, and liver (with conditions such as primary sclerosing cholangitis).
Prevalence and Significance of the Disease
- Prevalence: Crohn’s disease affects approximately 100–300 per 100,000 individuals in North America and Europe, with rising incidence in newly industrialized nations.
- Significance: The disease imposes a significant burden on quality of life due to chronic symptoms, frequent hospitalizations, and the need for lifelong management. It also has considerable economic and healthcare implications.
2. History & Discoveries
When and How was Crohn’s Disease First Identified?
- Early Recognition: Although symptoms of chronic intestinal inflammation were noted in historical medical texts, Crohn’s disease was first clearly described in the early 20th century.
- Clinical Definition: In 1932, Dr. Burrill B. Crohn and colleagues published a seminal paper that distinguished the disease as a unique entity separate from other forms of colitis.
Who Discovered It?
- Pioneers: The landmark work by Dr. Crohn, along with Drs. Leon Ginzburg and Gordon Oppenheimer, established the clinical and pathological features of the disease, which now bears Crohn’s name.
Major Discoveries and Breakthroughs
- Pathological Characteristics: Early studies identified the patchy, transmural inflammation and the formation of granulomas as hallmark features.
- Diagnostic Innovations: Advances such as endoscopy, radiographic imaging (CT and MRI enterography), and capsule endoscopy have improved diagnosis and disease monitoring.
- Therapeutic Breakthroughs: The development of immunomodulators and biologic agents (especially anti-TNF therapies) has revolutionized the treatment landscape.
Evolution of Medical Understanding Over Time
- Initially grouped with ulcerative colitis as a single IBD entity, subsequent research clarified that Crohn’s disease has distinct clinical, pathological, and genetic features. Modern understanding emphasizes the multifactorial etiology involving immune dysregulation, environmental triggers, and genetic predisposition.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Intermittent abdominal pain (often in the lower right quadrant).
- Diarrhea, which may be non-bloody or mildly bloody.
- Weight loss and fatigue.
- Advanced-Stage Symptoms:
- Severe, persistent abdominal pain.
- Frequent, debilitating diarrhea.
- Formation of fistulas, strictures, and abscesses.
- Systemic symptoms such as fever and significant weight loss.
- Perianal disease including fissures, fistulas, and abscesses.
Common vs. Rare Symptoms
- Common Symptoms:
- Abdominal cramping and pain.
- Diarrhea and urgency.
- Unintentional weight loss.
- Fatigue and general malaise.
- Rare Symptoms:
- Extra-intestinal manifestations such as arthritis, skin lesions (e.g., erythema nodosum), and eye inflammation (uveitis).
- Rare complications such as malabsorption syndromes and nutritional deficiencies.
How Symptoms Progress Over Time
- Crohn’s disease typically follows a relapsing-remitting course. Early, mild symptoms may progress to more severe, chronic inflammation if left untreated. Over time, repeated inflammatory episodes can result in structural damage to the bowel, leading to complications such as strictures and fistulas, which significantly impact quality of life.
4. Causes
Biological and Environmental Causes
- Immune Dysregulation: Crohn’s disease is believed to result from an abnormal immune response to gut microbiota in genetically predisposed individuals.
- Environmental Factors: Diet, stress, and exposure to certain pathogens are considered potential triggers that may incite or exacerbate the inflammatory process.
Genetic and Hereditary Factors
- Genetic Predisposition: Multiple genetic loci have been associated with increased susceptibility, notably mutations in the NOD2 gene and other genes involved in the innate immune response.
- Family History: Individuals with a family history of IBD have a higher risk of developing Crohn’s disease.
Known Triggers or Exposure Risks
- Microbial Factors: Alterations in the gut microbiome, including dysbiosis, have been implicated as contributing factors.
- Lifestyle Factors: Smoking is a well-established risk factor and is associated with a more aggressive disease course.
- Environmental Exposures: Urbanization, diet high in fats and refined sugars, and certain medications (e.g., antibiotics) have also been linked with increased risk.
5. Risk Factors
Who is Most at Risk?
- Age: Crohn’s disease often presents in adolescents and young adults, typically between the ages of 15 and 35.
- Gender: The disease affects both genders relatively equally, though slight variations in incidence and disease behavior have been noted.
- Ethnicity: Higher prevalence is observed in Caucasian populations, particularly those of Northern European descent; however, incidence is rising in other ethnic groups.
Environmental, Occupational, and Genetic Factors
- Environmental: Urban living, Western dietary patterns, and smoking are significant environmental risk factors.
- Occupational: Although less studied, occupations with high stress or exposure to environmental toxins may play a role.
- Genetic: A strong genetic component exists, with several identified risk alleles contributing to susceptibility.
Impact of Pre-existing Conditions
- Autoimmune Disorders: Patients with other autoimmune conditions may be at higher risk.
- Previous Gastrointestinal Infections: Prior infections that disrupt normal gut flora can predispose individuals to Crohn’s disease.
6. Complications
What Complications Can Arise from Crohn’s Disease?
- Bowel Obstruction: Chronic inflammation can lead to the formation of strictures, which narrow the intestinal lumen.
- Fistulas and Abscesses: Transmural inflammation may cause abnormal connections between the bowel and adjacent structures, as well as localized abscesses.
- Malnutrition: Chronic inflammation and malabsorption can result in significant nutritional deficiencies.
- Increased Cancer Risk: Long-standing Crohn’s disease, especially with extensive colonic involvement, is associated with an increased risk of colorectal cancer.
Long-Term Impact on Organs and Overall Health
- Persistent inflammation may lead to progressive bowel damage, reduced quality of life, and systemic complications affecting joints, skin, eyes, and liver.
Potential Disability or Fatality Rates
- Although Crohn’s disease itself is rarely fatal, its complications can lead to significant morbidity. Severe disease may result in disability due to chronic pain, nutritional deficiencies, and repeated surgical interventions.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation: Detailed patient history and physical examination focusing on gastrointestinal symptoms, nutritional status, and extra-intestinal manifestations.
- Endoscopy: Colonoscopy and upper endoscopy allow direct visualization of the mucosal surface and enable biopsies to confirm inflammation and granulomas.
- Imaging Studies: CT enterography, MRI, and small bowel follow-through studies help evaluate the extent of disease and detect complications such as strictures and fistulas.
Medical Tests
- Blood Tests: Inflammatory markers (CRP, ESR), complete blood count (CBC) for anemia, and tests for nutritional deficiencies.
- Stool Studies: To exclude infections and assess for occult blood.
- Histologic Examination: Biopsies obtained during endoscopy reveal the characteristic transmural inflammation and granuloma formation.
Early Detection Methods and Their Effectiveness
- Early detection via endoscopy and imaging, combined with serologic markers, facilitates timely intervention, potentially slowing disease progression and reducing complications.
8. Treatment Options
Standard Treatment Protocols
- Medications:
- Aminosalicylates: Used for mild to moderate disease to reduce inflammation.
- Corticosteroids: Employed for acute flare management.
- Immunomodulators: Agents such as azathioprine and 6-mercaptopurine help maintain remission.
- Biologic Therapies: Anti-TNF agents (e.g., infliximab, adalimumab), anti-integrin, and anti-interleukin drugs target specific inflammatory pathways.
- Surgical Interventions: Surgery is reserved for complications (e.g., strictures, fistulas, abscesses) or refractory disease. Resection of affected bowel segments may be necessary, though surgery is not curative.
- Nutritional Support: Dietary management and supplementation are critical to address malnutrition and support overall health.
Medications, Surgeries, and Therapies
- Medications: Often used in combination to achieve and maintain remission.
- Surgical Options: Include resection of diseased segments, stricturoplasty, and, in severe cases, creation of an ostomy.
- Adjunct Therapies: Psychological support, stress management, and physical rehabilitation play supportive roles in comprehensive care.
Emerging Treatments and Clinical Trials
- Novel Biologics and Small Molecule Inhibitors: Ongoing research is exploring new therapeutic targets, including JAK inhibitors and agents targeting IL-12/IL-23 pathways.
- Microbiome-Based Therapies: Fecal microbiota transplantation (FMT) and targeted probiotic therapies are under investigation for their potential to restore gut microbial balance.
- Personalized Medicine: Advances in genomics and biomarker identification are paving the way for more individualized treatment approaches.
9. Prevention & Precautionary Measures
How Can Crohn’s Disease be Prevented?
- Primary Prevention: Given its multifactorial etiology, complete prevention is not currently possible. However, minimizing modifiable risk factors—such as smoking cessation and maintaining a balanced diet—may help reduce risk.
- Secondary Prevention: Regular monitoring and early intervention can reduce the severity of flares and limit long-term complications.
Lifestyle Changes and Environmental Precautions
- Diet and Nutrition: A balanced, anti-inflammatory diet can support gut health. Some patients benefit from specific dietary modifications based on individual triggers.
- Smoking Cessation: Avoiding tobacco use is crucial, as smoking is associated with a more severe disease course.
- Stress Reduction: Psychological stress can trigger flares; stress management techniques, such as mindfulness and counseling, may be beneficial.
- Regular Medical Follow-Up: Routine check-ups and appropriate surveillance (including imaging and endoscopy) can help in early detection of complications.
Vaccines or Preventive Screenings
- Screenings: Regular endoscopic surveillance is recommended for patients with longstanding disease to monitor for dysplasia and early colorectal cancer.
- Vaccinations: While there is no vaccine for Crohn’s disease, patients should stay current with immunizations (e.g., influenza, pneumococcal) to reduce the risk of infections that might trigger flares.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Global Prevalence: Crohn’s disease affects approximately 100–300 per 100,000 individuals in North America and Europe, with increasing incidence in Asia and other regions.
- Regional Variations: Higher prevalence is noted in Western countries; however, globalization and lifestyle changes are contributing to rising rates in previously low-incidence areas.
Mortality and Survival Rates
- Mortality Impact: While Crohn’s disease itself is rarely directly fatal, its complications (e.g., sepsis, intestinal perforation) can increase mortality risk. Advances in treatment have improved long-term survival.
- Quality of Life: Effective management strategies have substantially enhanced quality of life and reduced disability for many patients.
Country-Wise Comparison and Trends
- Developed Countries: More comprehensive healthcare systems and advanced diagnostic tools contribute to earlier detection and better outcomes.
- Developing Regions: Underdiagnosis and limited access to specialized care may result in higher morbidity, though the incidence is rising as environmental risk factors become more prevalent.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Biologic and Targeted Therapies: Continued development of biologic agents and small molecule inhibitors is providing more effective and tailored treatment options.
- Microbiome Research: Studies investigating the gut microbiome are yielding insights that could lead to innovative therapies aimed at restoring a healthy microbial balance.
- Genomic and Biomarker Studies: Advances in genetics are helping to identify at-risk populations and may lead to personalized treatment regimens based on individual disease profiles.
Ongoing Studies and Future Medical Possibilities
- Clinical Trials: Numerous clinical trials are evaluating new treatment modalities, including combination therapies and novel immunomodulators.
- Regenerative Medicine: Research into stem cell therapies and tissue engineering holds promise for repairing damaged intestinal tissue.
- Precision Medicine: Future approaches may enable treatments to be tailored to the genetic and immunologic characteristics of each patient, potentially improving efficacy and minimizing adverse effects.
Potential Cures or Innovative Therapies
- While no cure for Crohn’s disease currently exists, emerging therapies—including immunomodulatory agents, microbiome-based treatments, and regenerative medicine—offer hope for achieving long-term remission and reducing disease progression.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Crohn’s Disease
- Disease Heterogeneity: Crohn’s disease exhibits a highly variable clinical course, with some patients experiencing mild intermittent symptoms while others develop severe, progressive disease.
- Extra-Intestinal Manifestations: Beyond gastrointestinal symptoms, Crohn’s can affect the skin, eyes, joints, and liver, underscoring its systemic nature.
- Environmental Paradox: Unlike ulcerative colitis, smoking is a well-established risk factor for Crohn’s disease and is associated with a more aggressive disease course.
Myths and Misconceptions vs. Medical Facts
- Myth: Crohn’s disease is caused solely by diet.
- Fact: While diet may influence symptoms, the etiology of Crohn’s disease is multifactorial, involving genetic, environmental, and immune-mediated factors.
- Myth: Surgery is a cure for Crohn’s disease.
- Fact: Surgery may be necessary to manage complications but does not cure the underlying inflammatory process.
- Myth: Crohn’s disease only affects the intestines.
- Fact: The disease has systemic implications, with extra-intestinal manifestations common in many patients.
Impact on Specific Populations or Professions
- Quality of Life: Crohn’s disease can significantly affect work, education, and social interactions, especially during active flares.
- Pediatric and Adolescent Impact: Early-onset Crohn’s disease may affect growth and development, necessitating tailored management strategies.
- Occupational Considerations: Individuals in high-stress or physically demanding jobs may experience exacerbated symptoms and require workplace accommodations.
References
– Provides clinical descriptions, diagnostic criteria, and treatment protocols for Crohn’s disease.
– Offers epidemiological data, risk factor analysis, and management strategies for Crohn’s disease based on current clinical guidelines.
– Summarizes recent research trends, emerging therapies, and genetic studies related to Crohn’s disease.