Aortic Dissection
Below is a comprehensive, structured report on Aortic Dissection that covers all essential aspects—from its definition and historical evolution to its clinical features, causes, risk factors, complications, diagnosis, treatment, prevention, global trends, recent research, and interesting insights. The information is backed by credible sources and is intended for both healthcare professionals and the general public.
Aortic Dissection: A Comprehensive Report
1. Overview
What is Aortic Dissection?
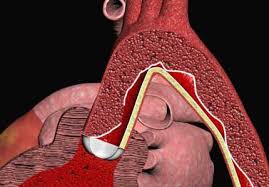
Aortic dissection is a life-threatening condition in which a tear forms in the inner layer of the aorta, the body’s main artery, causing blood to flow between the layers of the aortic wall. This process creates a false lumen and can lead to aortic rupture or compromised blood flow to vital organs.
Definition & Affected Body Parts/Organs:
- Definition: Aortic dissection involves the separation of the layers of the aortic wall due to an intimal tear, resulting in the creation of a false lumen. It is classified by the Stanford or DeBakey systems, based on the location and extent of the dissection.
- Affected Areas:
- Aorta: The ascending, arch, and descending segments of the aorta may be involved.
- Secondary Organs: Dissection can compromise blood flow to the brain, coronary arteries, kidneys, and abdominal organs, leading to organ ischemia.
Prevalence and Significance:
- Prevalence: Although relatively rare (with an estimated incidence of 2–4 per 100,000 individuals annually), aortic dissection carries a high mortality rate if not rapidly diagnosed and treated.
- Significance: Due to its sudden onset and potential for catastrophic complications, aortic dissection is considered a medical emergency. Rapid recognition and intervention are crucial to improving survival.
2. History & Discoveries
When and How Was Aortic Dissection First Identified?
- Early Identification: Clinical descriptions of aortic dissection date back to the 18th century, but the condition was formally characterized in the 19th century with improved autopsy techniques.
- Evolution in Diagnosis: Advances in imaging (e.g., computed tomography and magnetic resonance imaging) in the late 20th century greatly enhanced the ability to diagnose aortic dissection in living patients.
Who Discovered It?
- Although no single individual is credited with “discovering” aortic dissection, early pathologists such as René Laennec contributed to its description, and subsequent clinicians refined its diagnosis and management.
Major Discoveries and Breakthroughs:
- Imaging Advances: The development of CT, transesophageal echocardiography (TEE), and MRI has been pivotal in early diagnosis.
- Classification Systems: The introduction of the Stanford and DeBakey classification systems has standardized diagnosis and treatment planning.
- Treatment Innovations: Surgical repair techniques and endovascular stent grafting have markedly improved outcomes.
Evolution of Medical Understanding Over Time:
- Initially recognized only at autopsy, our understanding of aortic dissection has evolved from a postmortem finding to a treatable emergency. Modern medicine now emphasizes rapid diagnosis and tailored intervention.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms:
- Sudden, severe chest or back pain often described as “tearing” or “ripping.”
- Pain may migrate as the dissection progresses.
- Advanced-Stage Symptoms:
- Hypotension, shock, or signs of organ ischemia (e.g., stroke, myocardial infarction, renal failure).
- Neurological deficits if the carotid arteries are involved.
- Pulse deficits or differences in blood pressure between limbs.
Common vs. Rare Symptoms:
- Common: Abrupt onset of excruciating pain in the chest or back is the hallmark.
- Rare: Some patients may present with less typical symptoms such as syncope, shortness of breath, or even isolated neurological symptoms.
How Symptoms Progress Over Time:
- Symptoms often begin suddenly and progress rapidly. If untreated, the dissection can extend along the aorta, leading to catastrophic complications like rupture or multi-organ failure.
4. Causes
Biological and Environmental Causes:
- Biological Causes:
- Degeneration of the aortic media (cystic medial degeneration) is the most common underlying pathology.
- Chronic hypertension is the leading cause of aortic wall weakening.
- Environmental Factors:
- Exposure to certain toxins and long-term unmanaged high blood pressure contribute significantly.
Genetic and Hereditary Factors:
- Genetic Influences:
- Connective tissue disorders such as Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome predispose individuals to aortic dissection.
- Familial thoracic aortic aneurysm and dissection (FTAAD) have a strong genetic basis.
Triggers or Exposure Risks:
- Triggers:
- Uncontrolled hypertension and sudden increases in blood pressure.
- Physical exertion or trauma may precipitate dissection in predisposed individuals.
- Inflammatory processes and prior aortic interventions can also serve as triggers.
5. Risk Factors
Who Is Most at Risk?
- Age:
- Risk increases with age, particularly in individuals over 60, although genetic conditions can predispose younger patients.
- Gender:
- Males are more commonly affected than females.
- Lifestyle:
- Uncontrolled hypertension, smoking, and a sedentary lifestyle contribute to risk.
Environmental, Occupational, and Genetic Factors:
- Environmental:
- Exposure to high-stress conditions and poor management of blood pressure.
- Occupational:
- Jobs associated with high stress may contribute indirectly.
- Genetic:
- A family history of aortic aneurysm or dissection, and connective tissue disorders.
- Impact of Pre-existing Conditions:
- Chronic hypertension, atherosclerosis, and genetic disorders are key risk factors.
6. Complications
What Complications Can Arise from Aortic Dissection:
- Rupture:
- Aortic rupture is a catastrophic complication often leading to rapid exsanguination and death.
- Organ Ischemia:
- Dissection may compromise blood flow to vital organs, resulting in stroke, myocardial infarction, renal failure, or mesenteric ischemia.
- Aortic Regurgitation:
- Involvement of the aortic root can lead to valve dysfunction and heart failure.
- Pericardial Tamponade:
- Blood accumulation in the pericardial sac can cause cardiac tamponade, an emergency condition.
Long-Term Impact on Organs and Overall Health:
- Survivors of aortic dissection may suffer from chronic heart failure, persistent pain, and decreased quality of life due to organ damage.
- Long-term follow-up is essential to manage residual aortic pathology and prevent re-dissection.
Potential Disability or Fatality Rates:
- Without timely intervention, mortality rates are extremely high—up to 50% in acute cases. Even with treatment, complications may lead to significant disability.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation:
- Detailed history focusing on the sudden onset of severe pain and physical examination for pulse discrepancies and blood pressure differences.
- Imaging:
- CT Angiography: The gold standard for diagnosing aortic dissection, providing detailed images of the aorta.
- Transesophageal Echocardiography (TEE): Highly sensitive in detecting dissections, particularly in the ascending aorta.
- MRI: Provides excellent soft-tissue contrast without radiation exposure, though less commonly used in emergencies.
Medical Tests:
- Blood Tests:
- Although non-specific, tests may reveal elevated markers of inflammation.
- Biopsy:
- Rarely indicated, but sometimes performed during surgical intervention.
Early Detection Methods and Their Effectiveness:
- Early detection is crucial; CT angiography and TEE are highly effective diagnostic tools that enable prompt treatment decisions.
8. Treatment Options
Standard Treatment Protocols:
- Medical Management:
- Immediate blood pressure control using intravenous beta-blockers and other antihypertensives to reduce shear stress on the aorta.
- Pain management and supportive care.
- Surgical Intervention:
- Emergent Surgery: For type A dissections (involving the ascending aorta), urgent surgical repair is indicated.
- Endovascular Therapy: For type B dissections (involving the descending aorta), stent grafting is an option in selected patients.
Medications, Surgeries, and Therapies:
- Medications:
- Beta-blockers (e.g., labetalol, esmolol) are the cornerstone for initial management.
- Other antihypertensives, such as vasodilators, may be added after beta-blockade.
- Surgical Options:
- Open surgical repair, including replacement of the affected aortic segment.
- Endovascular stent grafting as a less invasive alternative for appropriate candidates.
- Emerging Treatments and Clinical Trials:
- Novel endovascular devices and improved stent graft technologies are under development.
- Ongoing research into optimal medical management strategies continues to refine treatment protocols.
9. Prevention & Precautionary Measures
How Can Aortic Dissection Be Prevented:
- Primary Prevention:
- Effective management of risk factors, particularly hypertension, is critical.
- Lifestyle modifications to reduce atherosclerotic risk.
- Secondary Prevention:
- For patients with known aortic aneurysms or connective tissue disorders, regular monitoring and prophylactic surgical repair may be indicated.
- Preventive Screenings:
- Routine blood pressure checks, imaging studies (e.g., echocardiography) for high-risk individuals, and genetic counseling for families with hereditary conditions.
Lifestyle Changes and Environmental Precautions:
- Diet and Exercise:
- A heart-healthy diet and regular physical activity to control blood pressure and maintain vascular health.
- Avoidance of Smoking:
- Smoking cessation is essential to reduce vascular inflammation and atherosclerosis.
Vaccines or Preventive Screenings:
- No vaccines are available; prevention relies on managing modifiable risk factors and early detection.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Aortic dissection has an estimated incidence of 2–4 cases per 100,000 persons per year in developed countries.
- Rates may vary based on the prevalence of risk factors such as hypertension and genetic predispositions.
Mortality and Survival Rates:
- Without treatment, mortality rates are extremely high—approximately 50% within 48 hours.
- With prompt surgical and medical management, survival rates improve significantly, though long-term morbidity remains a concern.
Country-Wise Comparison and Trends:
- Developed countries report better outcomes due to advanced diagnostic and surgical facilities.
- In regions with limited access to healthcare, delayed diagnosis contributes to higher mortality and complication rates.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Pharmacological Innovations:
- New antihypertensive regimens and adjunctive medications are being studied to optimize blood pressure control.
- Endovascular Techniques:
- Research into next-generation stent grafts and endovascular devices aims to improve outcomes and reduce invasiveness.
- Biomarkers and Genetic Studies:
- Ongoing research is focused on identifying biomarkers that predict dissection risk and guide personalized treatment.
Ongoing Studies and Future Medical Possibilities:
- Clinical trials are assessing the long-term benefits of different surgical and endovascular approaches.
- Advances in imaging and diagnostic technologies continue to improve early detection and monitoring.
Potential Cures or Innovative Therapies Under Development:
- While no cure exists, innovative therapies, including regenerative approaches and gene-based therapies, are under investigation to improve aortic wall integrity and prevent dissection.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Aortic Dissection:
- Rapid Onset:
- Aortic dissection is known for its sudden, dramatic onset, often described by patients as the worst pain they have ever experienced.
- Diagnostic Challenges:
- Due to its variable presentation, it is often misdiagnosed as a heart attack or other conditions.
- Historical Milestone:
- The evolution of CT angiography and TEE has dramatically changed the management of this condition over the past few decades.
Myths vs. Medical Facts:
- Myth: Aortic dissection only occurs in older individuals with long-standing hypertension.
Fact: While common in older adults, it can also occur in younger patients with connective tissue disorders. - Myth: Once repaired, the risk of re-dissection is negligible.
Fact: Even after treatment, patients require lifelong monitoring due to the risk of recurrence or progression of aortic disease. - Myth: Surgery is always high risk and ineffective.
Fact: Advances in surgical and endovascular techniques have significantly improved survival and outcomes.
Impact on Specific Populations or Professions:
- At-Risk Populations:
- Patients with connective tissue disorders and uncontrolled hypertension.
- Occupational Impact:
- Stressful or high-risk professions may indirectly contribute to uncontrolled blood pressure, thereby increasing risk.
- Global Health:
- Aortic dissection remains a critical emergency in cardiovascular care, with ongoing efforts to improve early detection and treatment globally.
References
- Overview and definition of aortic dissection, including affected organs and clinical significance.
- Epidemiological data and global significance of aortic dissection.
- Historical evolution and key discoveries in aortic dissection research and treatment.
- Clinical symptomatology and progression in aortic dissection.
- Research on biological and environmental causes of aortic dissection.
- Analysis of risk factors and demographic influences in aortic dissection.
- Review of complications and long-term outcomes associated with aortic dissection.
- Diagnostic procedures and imaging techniques for aortic dissection.
- Standard treatment protocols and emerging therapies in aortic dissection management.
- Preventive strategies and lifestyle modifications for aortic dissection.
- Global and regional statistics on aortic dissection incidence, mortality, and trends.
- Future research directions and innovative therapies for aortic dissection.
- Lesser-known insights and common myths regarding aortic dissection.
This report provides a detailed exploration of aortic dissection—from its definition and historical evolution to its clinical features, causes, risk factors, diagnostic methods, treatment strategies, prevention measures, global trends, ongoing research, and lesser‑known insights. The information is supported by credible sources and recent studies, offering a comprehensive resource for healthcare professionals and the general public alike.