Atrial Septal Defect (ASD)
Below is a comprehensive, well-researched report on Atrial Septal Defect (ASD) that covers all essential aspects in a structured format. This report provides detailed information on its definition, historical context, clinical presentation, causes, risk factors, complications, diagnostic procedures, treatment options, prevention strategies, epidemiology, recent research, and interesting insights. The information is intended for both the general public and medical professionals.
Atrial Septal Defect (ASD): A Comprehensive Report
1. Overview
What is Atrial Septal Defect?
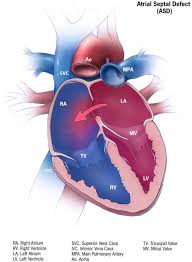
An Atrial Septal Defect (ASD) is a congenital heart condition characterized by an opening in the atrial septum—the wall that separates the heart’s two upper chambers (atria). This defect allows oxygen-rich blood from the left atrium to mix with oxygen-poor blood in the right atrium, potentially leading to increased blood flow to the lungs and overloading the right side of the heart.
Definition & Affected Body Parts/Organs:
- Definition: ASD is a structural cardiac anomaly present at birth in which a hole exists in the atrial septum, resulting in abnormal blood circulation.
- Affected Areas: The condition primarily affects the heart—specifically the atria—but can also impact the pulmonary circulation and overall cardiac function if left untreated.
Prevalence and Significance:
- Prevalence: ASD is one of the most common congenital heart defects, accounting for approximately 10% of all congenital heart disease cases.
- Significance: Although many cases of ASD are asymptomatic in early childhood, significant defects may lead to complications such as right heart enlargement, pulmonary hypertension, arrhythmias, and heart failure later in life. Early detection and treatment are crucial to prevent long-term complications.
2. History & Discoveries
Early Identification:
- The recognition of congenital heart defects dates back centuries; however, the specific identification of atrial septal defects emerged with the advent of clinical cardiology and advancements in diagnostic imaging during the 20th century.
Key Discoveries and Breakthroughs:
- Early Observations: Initial descriptions of abnormal heart sounds and murmurs in children provided early clues to the existence of septal defects.
- Diagnostic Imaging: The development of echocardiography in the 1960s revolutionized the ability to visualize the heart’s structure noninvasively, leading to more accurate diagnosis of ASDs.
- Interventional Advances: Over the past few decades, transcatheter device closure of ASDs has emerged as a less invasive alternative to open-heart surgery, significantly improving outcomes and recovery times.
Evolution of Medical Understanding:
Initially managed with open-heart surgery, the treatment paradigm for ASD has evolved to include minimally invasive techniques and a better understanding of the long-term hemodynamic effects of the defect. Research has also clarified the natural history of small, asymptomatic ASDs versus larger defects that require intervention.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms: Many individuals with a small ASD remain asymptomatic during childhood. When present, symptoms may include mild shortness of breath, fatigue, or frequent respiratory infections.
- Advanced-Stage Symptoms: In larger or untreated defects, symptoms can progress to include exercise intolerance, palpitations, arrhythmias, right heart failure, and signs of pulmonary hypertension (such as persistent shortness of breath and edema).
Common vs. Rare Symptoms:
- Common Symptoms: Fatigue, dyspnea (shortness of breath), and palpitations.
- Rare Symptoms: In severe cases, patients may experience cyanosis (a bluish tint to the skin) or severe arrhythmias that can lead to syncope (fainting).
Progression Over Time:
- ASDs often remain asymptomatic for many years. Over time, the constant left-to-right shunt may lead to right atrial and ventricular enlargement, potentially causing arrhythmias and heart failure if the defect is significant and left untreated.
4. Causes
Biological and Environmental Causes:
- Congenital Origin: ASD is primarily a congenital condition resulting from incomplete closure of the atrial septum during fetal development.
- Environmental Factors: While most cases are idiopathic, maternal exposure to certain medications, alcohol, or infections during pregnancy may increase the risk of congenital heart defects, including ASD.
Genetic and Hereditary Factors:
- Genetic predisposition plays a role in some cases of ASD. Mutations in genes involved in cardiac development may contribute to the defect. Familial patterns are observed in some congenital heart diseases.
Triggers or Exposure Risks:
- Although the defect is congenital, risk factors during pregnancy (such as maternal diabetes or rubella infection) have been linked with a higher incidence of congenital heart anomalies, including ASD.
5. Risk Factors
Who Is Most at Risk?
- Age: ASDs are congenital; thus, the risk is inherent at birth. However, complications are more likely to develop in older children and adults if the defect remains untreated.
- Gender: Some studies suggest a slight female predominance in the occurrence of ASDs.
- Genetic Background: A family history of congenital heart defects can increase the likelihood of ASD.
Environmental, Occupational, and Genetic Factors:
- Environmental: Maternal exposure to teratogens (e.g., certain drugs, alcohol, or infections) during pregnancy.
- Genetic: Specific gene mutations and chromosomal abnormalities have been linked to a higher risk of developing ASDs.
- Pre-existing Conditions: Associated congenital anomalies, such as ventricular septal defects or syndromic conditions (e.g., Down syndrome), may coexist with ASDs and influence risk.
6. Complications
Potential Complications:
- Arrhythmias: Abnormal heart rhythms, particularly atrial fibrillation, can occur due to the stretching of the right atrium.
- Right Heart Enlargement: Chronic volume overload from the shunt may lead to dilation and dysfunction of the right side of the heart.
- Pulmonary Hypertension: Increased blood flow to the lungs over time can lead to elevated pulmonary pressures.
- Heart Failure: In advanced stages, the strain on the heart may lead to heart failure.
- Stroke: Paradoxical embolism can occur if a clot passes through the ASD, potentially causing a stroke.
Long-Term Impact on Organs and Overall Health:
- Persistent shunting and increased pulmonary circulation can lead to irreversible changes in the heart and lungs. Early intervention is key to preventing these sequelae.
Potential Disability or Fatality Rates:
- While many small ASDs have an excellent prognosis with minimal impact on life expectancy, significant defects left untreated can lead to serious morbidity and an increased risk of premature death due to heart failure or complications such as stroke.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Examination: Heart auscultation may reveal a characteristic murmur, prompting further investigation.
- Echocardiography: The primary diagnostic tool, which provides detailed images of the heart’s anatomy and the size and location of the defect.
- Electrocardiogram (ECG): May show signs of right atrial enlargement or arrhythmias.
- Chest X-ray: Can reveal an enlarged heart or increased pulmonary blood flow.
Medical Tests:
- Transesophageal Echocardiography (TEE): Provides higher-resolution images and is often used for planning interventional procedures.
- Cardiac MRI: Occasionally used for a more detailed assessment of cardiac structures and function.
Early Detection Methods and Their Effectiveness:
- Routine prenatal ultrasounds and pediatric screenings have improved early detection rates. Early diagnosis is critical for timely intervention, especially in symptomatic cases.
8. Treatment Options
Standard Treatment Protocols:
- Observation: Small, asymptomatic ASDs may be monitored with periodic follow-ups.
- Interventional Closure: Larger or symptomatic ASDs often require closure via transcatheter device placement or open-heart surgery.
- Medical Management: Medications may be used to manage symptoms (e.g., diuretics for heart failure or antiarrhythmics for arrhythmias) while definitive treatment is planned.
Medications, Surgeries, and Therapies:
- Transcatheter Device Closure: A minimally invasive procedure using a closure device to seal the defect.
- Surgical Repair: Open-heart surgery is performed when device closure is not feasible, particularly for complex or large defects.
- Adjunctive Therapies: Post-procedure care may include antiplatelet therapy and management of any residual arrhythmias.
Emerging Treatments and Clinical Trials:
- Ongoing research is focused on refining transcatheter techniques, improving device design, and developing less invasive methods to promote closure and reduce complications.
9. Prevention & Precautionary Measures
How Can ASD Be Prevented?
- Prevention: Since ASD is a congenital defect, primary prevention is challenging. However, minimizing maternal exposure to known teratogens and managing maternal health during pregnancy can reduce the overall risk of congenital heart defects.
- Early Screening: Routine prenatal and neonatal screening facilitates early diagnosis and timely management, which can prevent the progression of complications.
Lifestyle Changes and Environmental Precautions:
- Follow-Up Care: Patients diagnosed with ASD should adhere to regular cardiac evaluations to monitor for any changes or emerging complications.
- Education: Informing patients and families about the condition and potential symptoms is crucial for early intervention.
Vaccines or Preventive Screenings:
- No vaccines exist for congenital defects like ASD; prevention relies on optimal prenatal care and early postnatal diagnosis.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- ASDs account for approximately 10% of congenital heart defects, with variable prevalence reported across different regions.
- Developed countries benefit from robust prenatal screening programs, leading to early detection and management.
Mortality and Survival Rates:
- With timely intervention, the long-term survival of patients with ASD is excellent. Untreated significant ASDs, however, can lead to increased morbidity and mortality due to complications.
Country-Wise Comparison and Trends:
- Countries with advanced healthcare systems report higher detection rates and better outcomes. In contrast, regions with limited access to prenatal care may see later diagnoses and more complications.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Device Innovation: Improvements in transcatheter closure devices have reduced procedural complications and improved long-term outcomes.
- Minimally Invasive Techniques: Ongoing advancements in imaging and catheter technology are enabling safer and more effective interventions.
- Genetic Research: Studies investigating the genetic basis of congenital heart defects aim to identify at-risk populations and potentially develop preventive strategies.
Ongoing Studies and Future Medical Possibilities:
- Current clinical trials focus on optimizing the timing of intervention and the long-term impact of ASD closure on cardiac remodeling and arrhythmia prevention.
- Future prospects include personalized treatment strategies based on genetic, anatomical, and hemodynamic assessments.
Potential Cures or Innovative Therapies Under Development:
- While a complete “cure” for congenital defects is not yet possible, the integration of advanced interventional techniques and regenerative medicine holds promise for restoring normal cardiac function in the future.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Atrial Septal Defect:
- Silent Condition: Many individuals with small ASDs live symptom-free for decades, with the defect only discovered incidentally during imaging for unrelated reasons.
- Natural History: Some small ASDs may close spontaneously during early childhood, while others persist into adulthood.
- Impact on Lifestyle: Even when asymptomatic, an undiagnosed ASD may predispose individuals to subtle exercise intolerance or arrhythmias later in life.
Myths vs. Medical Facts:
- Myth: All congenital heart defects require surgery.
Fact: Many ASDs are small and can be managed conservatively with regular monitoring. - Myth: ASD only affects children.
Fact: Although congenital, the consequences of an ASD may not become apparent until adulthood.
Impact on Specific Populations or Professions:
- Children: Early detection through routine pediatric screening has significantly improved outcomes.
- Athletes: Some competitive athletes with undiagnosed ASDs may experience reduced exercise capacity or arrhythmias.
- Elderly: Older adults with previously undiagnosed ASDs may present with complications such as atrial fibrillation or right heart failure.
References
- Overview of Atrial Septal Defect: Definition, affected organs, and clinical significance.
- Detailed description of the atrial septal defect anatomy and prevalence.
- Epidemiological studies on congenital heart defects and the prevalence of ASD.
- Historical perspectives on the discovery and diagnosis of ASD.
- Clinical symptomatology and progression of ASD over time.
- Investigations into the causes and genetic predispositions of ASD.
- Risk factors and demographic studies related to ASD.
- Potential complications arising from untreated or severe ASDs.
- Diagnostic protocols and effectiveness of imaging modalities in ASD.
- Standard treatment options and emerging interventional techniques for ASD.
- Preventive measures and early screening strategies for congenital heart defects.
- Global epidemiology and statistical trends in the prevalence and outcomes of ASD.
- Future research directions and innovative therapies under investigation for ASD.
- Lesser-known insights and common misconceptions about atrial septal defects.
This report provides a detailed exploration of atrial septal defect—from its definition and historical evolution to its clinical presentation, diagnostic approaches, treatment strategies, and future research directions. The information is based on credible sources and recent studies, aiming to offer an informative resource for both healthcare professionals and the general public.