About bowel incontinence
Bowel incontinence, also known as faecal incontinence, is the inability to control bowel movements, leading to involuntary soiling. It can vary greatly in severity and frequency:
Types of Bowel Incontinence
- Urge Incontinence: A sudden, strong urge to go to the toilet but being unable to get there in time.
- Passive Incontinence: No sensation before involuntary soiling.
- Occasional Soiling: Some people may experience slight soiling when passing wind.
- Chronic Incontinence: For some, it can be a daily issue; for others, it happens less frequently.
Bowel incontinence is relatively common, affecting up to 1 in 10 people at some point in their lives. While it can affect anyone, it is more prevalent among the elderly and women.
Causes
Bowel incontinence is usually a symptom of an underlying issue, including:
- Diarrhoea or Constipation: Frequent loose stools or impacted stools can affect bowel control.
- Muscle Weakness: Damage or weakening of the anal sphincter muscles.
- Nerve Damage: Conditions affecting nerves that control bowel movements, such as diabetes, multiple sclerosis, or spinal cord injuries.
- Chronic Conditions: Dementia and other long-term illnesses may lead to incontinence.
Seeking Help
It’s important to address bowel incontinence with a healthcare professional:
- No Shame: Bowel incontinence is a medical issue like any other condition and can often be treated.
- Effectiveness of Treatment: There are many treatment options available that can significantly improve symptoms.
- Specialist Services: If you’re not comfortable discussing it with a GP, you can access NHS continence services directly.
Treatment Options
Effective management of bowel incontinence depends on the cause and severity:
- Lifestyle and Diet: Adjustments to relieve constipation or manage diarrhoea.
- Pelvic Floor Exercises: Strengthening the muscles that control bowel movements.
- Medication: To regulate bowel movements, either for constipation or diarrhoea.
- Surgery: Various procedures may be recommended for severe cases.
- Incontinence Products: Anal plugs, pads, and other aids can help until symptoms improve.
With appropriate treatment and support, most people with bowel incontinence can achieve better symptom control and improve their quality
Causes of bowel incontinence
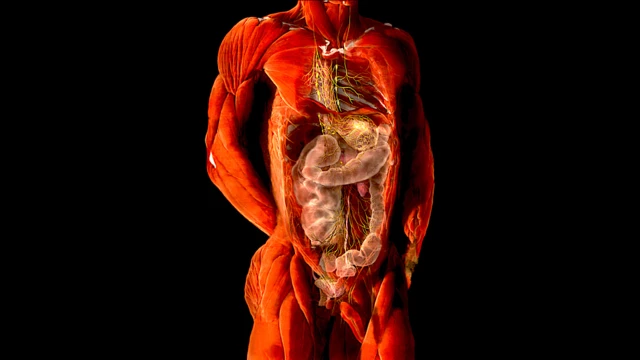
Bowel incontinence often results from physical problems with the structures that control bowel movements. Common causes include:
Problems with the Rectum
- Constipation: Severe constipation can lead to a large, solid stool becoming stuck in the rectum (fecal impaction), stretching and weakening the rectal muscles. This can cause overflow incontinence, where watery stool leaks around the impacted stool. Constipation can also lead to rectal prolapse, when part of the lower intestine protrudes from the anus.
- Diarrhea: The rectum has a harder time retaining liquid stool, which makes it more likely for people with recurrent diarrhea to experience bowel incontinence. Conditions like Crohn’s disease, irritable bowel syndrome (IBS), and ulcerative colitis may cause chronic diarrhea and rectal scarring.
- Haemorrhoids: Enlarged blood vessels in or around the rectum (hemorrhoids) can lead to discomfort, itching, and even bowel incontinence in severe cases.
Problems with the Sphincter Muscles
The sphincter muscles control the opening and closing of the rectum. Weakness or damage to these muscles can lead to incontinence. Childbirth, particularly vaginal deliveries involving a large baby, forceps use, or prolonged labor, can stretch or damage these muscles. Other causes of sphincter muscle damage include injury or surgery involving the bowel or rectum.
Nerve Damage
Bowel incontinence can result from issues with the nerves that link the brain to the rectum. Nerve damage can cause a lack of awareness of stools in the rectum or difficulty controlling the sphincter muscles. Conditions linked to nerve damage include:
- Diabetes
- Multiple sclerosis (MS)
- Stroke
- Spina bifida (a birth defect affecting spinal development)
- Spinal injuries
Other Health Conditions
Certain conditions, such as dementia or severe learning disabilities, may lead to loss of bowel control. Physical disabilities that impair mobility may also make it difficult to reach the toilet in time, contributing to incontinence.
If you experience bowel incontinence, it is important to consult a healthcare professional to identify the cause and explore appropriate treatment options.
Diagnosing bowel incontinence
Diagnosing bowel incontinence involves a combination of discussing symptoms with your GP, a physical examination, and potentially further testing to determine the underlying cause and best treatment options. Here’s what you can expect during the process:
Initial GP Consultation
Your GP will ask about:
- Symptoms and Patterns: When and how frequently incontinence occurs.
- Dietary Habits: Any recent changes that could contribute.
- Bowel Habits: Persistent changes, rectal bleeding, stomach pains, etc.
- Medications: Possible side effects impacting your condition.
Physical Examination
- External Examination: Your GP will visually inspect the anus and surrounding area for damage, hemorrhoids, or other visible issues.
- Rectal Examination: A gloved finger is inserted into the rectum to check for blockages, tumors, or other abnormalities and to assess the strength of your sphincter muscles.
Further Diagnostic Tests
If necessary, your GP may refer you for additional tests:
- Endoscopy (Sigmoidoscopy): A thin, flexible tube with a camera examines the inside of the rectum and lower bowel for obstruction, damage, or inflammation.
- Anal Manometry: Assesses muscle and nerve function in the rectum using a small balloon device that measures pressure and responsiveness.
- Ultrasound: Provides detailed images of the anus and sphincter muscles to detect any underlying damage.
- Defecography: Involves inserting a barium liquid into the rectum to highlight problems using X-rays while you pass stools. This test can also be performed using an MRI scanner to detect obstructions or prolapse.
These tests help identify the specific cause of bowel incontinence, allowing your healthcare provider to recommend the most appropriate treatment options. While the examinations may feel uncomfortable or embarrassing, they are important for accurate diagnosis and effective treatment planning.
Treating bowel incontinence
Treatment for bowel incontinence focuses on the underlying cause and severity of symptoms, typically starting with less invasive methods before considering medication or surgery. Here’s a summary of potential treatments:
1. Continence Products
- Anal Plugs: Made of foam, they expand when in contact with moisture to prevent leakage but are generally a short-term solution.
- Disposable Body Pads: Absorb liquid stools and protect skin, useful for mild incontinence.
- Single-use Silicone Inserts: Form a seal around the rectum and help control moderate to severe incontinence.
- NHS Continence Services: Offer advice and support without a GP referral.
2. Lifestyle and Dietary Changes
- Diarrhea Management: Reduce intake of high-fiber foods, skin and pips of fruits and vegetables, and limit fizzy drinks and caffeine.
- Constipation Management: Adopt a high-fiber diet with fruits, vegetables, whole grains, nuts, seeds, and plenty of fluids.
- Food Diary: Helps identify foods that may worsen symptoms.
3. Exercise Programs
- Pelvic Floor Muscle Training: Helps strengthen pelvic muscles. Involves exercises like squeezing and relaxing pelvic muscles.
- Bowel Retraining: Improves stool consistency, establishes regular bowel times, and finds ways to stimulate bowel movements.
- Biofeedback: Uses a probe to provide feedback on muscle activity during training exercises.
4. Medication
- Loperamide: Used for diarrhea by slowing down stool movement.
- Laxatives: Help with constipation, usually bulk-forming types.
- Enemas or Rectal Irrigation: Used if other treatments fail to remove impacted stool.
5. Surgical Options
- Sphincteroplasty: Repairs damaged sphincter muscles.
- Sacral Nerve Stimulation: Electrical stimulation improves muscle control.
- Tibial Nerve Stimulation: Electrical stimulation of the tibial nerve.
- Injectable Bulking Agents: Strengthen sphincter muscles with injected materials like collagen.
- Endoscopic Heat Therapy: Uses heat to tighten sphincter muscles.
- Artificial Sphincter: A cuff is implanted to control the anus with a control pump.
- Colostomy: Creates an opening in the colon for stool collection in a bag; a last-resort treatment.
Each treatment option aims to improve bowel function and manage symptoms effectively, often combining several approaches to maximize outcomes. Your healthcare provider can offer more detailed advice based on your specific situation and needs.