Crohn’s Disease
What is Crohn’s Disease?
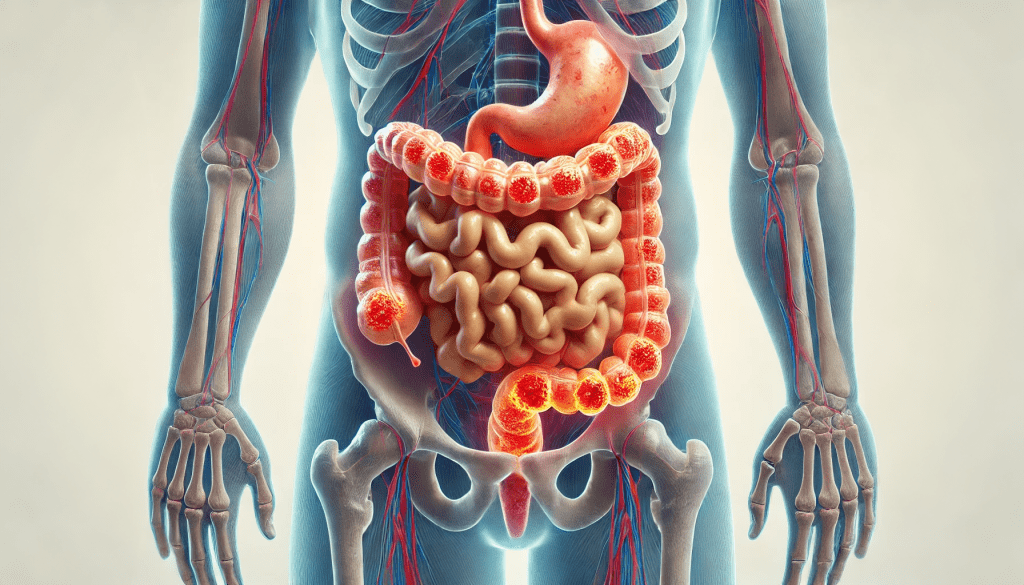
Crohn’s Disease is a chronic condition that causes inflammation of the lining of the digestive system, primarily affecting the last section of the small intestine (ileum) or the large intestine (colon). The inflammation can appear anywhere from the mouth to the anus, causing a wide range of symptoms. It is a type of inflammatory bowel disease (IBD).
Symptoms
Symptoms of Crohn’s Disease can vary greatly depending on the part of the digestive system affected and the severity of inflammation. Common symptoms include:
- Recurring Diarrhea: Often severe and may contain blood or mucus.
- Abdominal Pain and Cramping: Pain typically worsens after meals.
- Fatigue: Extreme tiredness is common, even when resting.
- Unintended Weight Loss: Due to reduced appetite and poor nutrient absorption.
- Blood and Mucus in Stool: Can occur during severe flare-ups.
Additional Symptoms
- High temperature (fever)
- Nausea or vomiting
- Joint pain and swelling (arthritis)
- Inflammation of the eyes (uveitis)
- Skin issues such as painful, red, and swollen areas, often on the legs
- Mouth ulcers
- Perianal symptoms like anal pain and discharge
Children with Crohn’s disease may experience delayed growth and development.
When to Consult Your GP:
- Persistent diarrhea lasting more than seven days
- Unexplained abdominal pain or weight loss
- Blood in the stool
- Concerns about your child’s growth and development
Causes
The exact cause of Crohn’s Disease remains unclear, but a combination of factors plays a role, including:
- Genetics: A family history of Crohn’s may increase the risk.
- Immune System Dysfunction: An abnormal immune response may attack healthy gut bacteria, leading to inflammation.
- Environmental Triggers: Air pollution, previous infections, and certain medications.
- Smoking: Increases the risk and severity of symptoms.
Diagnosis
Diagnosis typically involves assessing symptoms, family history, diet, and recent medical history. Tests may include:
- Blood Tests: To check for inflammation, infection, and anemia.
- Stool Sample: To detect blood, infection, or inflammation.
- Specialist Tests: Colonoscopy, gastroscopy, sigmoidoscopy, MRI, CT scans, or capsule endoscopy.
Treatment Options
While there is no cure for Crohn’s Disease, treatment aims to manage symptoms and reduce inflammation:
1. Medications
- Steroids: Corticosteroids such as prednisolone are used for quick inflammation reduction but are not suitable for long-term use.
- Immunosuppressants: Help suppress immune activity, such as azathioprine or methotrexate.
- Biological Therapies: Target specific chemicals in the immune response, such as adalimumab, infliximab, or vedolizumab.
Note: These medications may have side effects, so regular monitoring is essential.
2. Surgery
- May involve resection (removing affected bowel segments) or creating an ileostomy.
- Used when medications fail or complications arise.
3. Lifestyle and Dietary Changes
- Diet: Eat small meals, drink water, and maintain a balanced diet. Avoid trigger foods.
- Smoking Cessation: Crucial to reduce symptoms and complications.
Complications
- Stricture: Narrowing of the bowel, causing blockage.
- Fistula: Abnormal connection between the bowel and other organs or skin.
Complications often require surgery for correction.
Pregnancy and Fertility
- Crohn’s generally does not affect fertility, but surgeries may have an impact.
- Women planning pregnancy should discuss medication changes with their IBD team.
Support and Management
- Regular check-ups and discussions with healthcare professionals.
- Monitoring symptoms and adjusting treatments as needed.
- Mental and emotional support, including counseling.
For more personalized support, always speak to your healthcare provider.