Chronic Pancreatitis: A Detailed Overview
What is Chronic Pancreatitis?
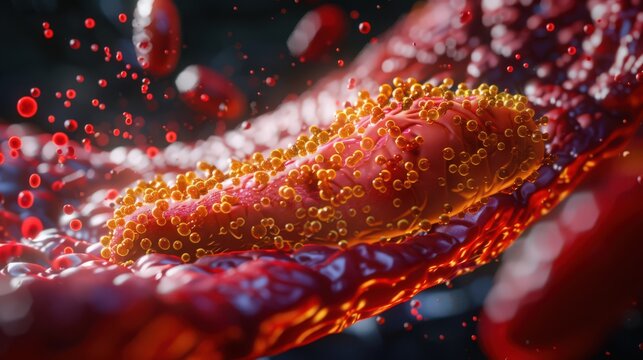
Chronic pancreatitis is a long-term condition where the pancreas becomes inflamed and damaged, leading to permanent changes in its structure and function. The pancreas is a small organ situated behind the stomach and below the ribcage, essential for producing enzymes that aid digestion and hormones like insulin that regulate blood sugar levels. Chronic pancreatitis differs from acute pancreatitis, which is a sudden and short-term inflammation of the pancreas.
Symptoms of Chronic Pancreatitis
The primary symptom of chronic pancreatitis is severe, recurrent abdominal pain, often felt in the upper abdomen and radiating to the back. Pain episodes may last for several hours or even days, with certain triggers such as eating or consuming fatty foods exacerbating symptoms.
As the condition progresses, additional symptoms can develop, including:
- Greasy, Foul-Smelling Stools (Steatorrhea): Due to insufficient production of digestive enzymes, fats are not properly digested, resulting in oily, foul-smelling stools that may float.
- Weight Loss: Despite adequate food intake, weight loss occurs due to nutrient malabsorption.
- Nausea and Vomiting: Frequent episodes can occur, especially after meals.
- Diabetes: Damage to insulin-producing cells in the pancreas may lead to the development of diabetes.
When to Seek Medical Advice
It is crucial to consult your GP if you experience:
- Severe abdominal pain, as it may be a sign of pancreatic inflammation or other complications.
- Persistent digestive symptoms such as oily stools or unintentional weight loss.
Causes of Chronic Pancreatitis
The causes of chronic pancreatitis include:
- Long-Term Alcohol Misuse: Heavy, prolonged alcohol consumption accounts for approximately 70% of cases. Repeated damage from alcohol can lead to inflammation and scarring of the pancreas.
- Smoking: Smoking can exacerbate pancreatic inflammation and increase the risk of complications.
- Autoimmune Response: In some cases, the immune system mistakenly attacks the pancreas, causing chronic inflammation.
- Genetic Factors: Genetic mutations may disrupt the pancreas’ normal functions, increasing susceptibility to chronic inflammation.
- Idiopathic Chronic Pancreatitis: In about 30% of cases, no specific cause can be identified.
Who is Affected?
Chronic pancreatitis can affect individuals of any age, but it is most common in middle-aged men, particularly those aged 45 to 54. Lifestyle factors such as alcohol consumption and smoking play a significant role in the risk of developing the condition.
Treatment of Chronic Pancreatitis
While there is no cure for chronic pancreatitis, the treatment focuses on managing symptoms, slowing disease progression, and improving the quality of life. The key aspects of treatment include:
- Lifestyle Changes:
- Avoiding Alcohol: Alcohol cessation is crucial for reducing symptoms and preventing further damage.
- Quitting Smoking: Smoking cessation can help control inflammation and reduce the risk of complications.
- Pain Management: Chronic pain is often challenging to manage and may require:
- Pain Relievers: Non-prescription or prescription pain medications.
- Nerve Blocks: Injections that block pain signals from reaching the brain.
- Enzyme Replacement Therapy: Supplements can aid digestion by replacing missing pancreatic enzymes, improving nutrient absorption, and reducing symptoms like oily stools.
- Insulin Therapy: Diabetes resulting from pancreatic damage may require insulin or other medications to manage blood sugar levels.
- Surgery: In severe cases where symptoms are unmanageable with medication, surgical interventions may be necessary to relieve blockages, drain fluid, or remove damaged tissue.
Complications of Chronic Pancreatitis
Living with chronic pancreatitis can lead to both physical and mental health challenges, including:
- Chronic Pain: Persistent pain can lead to stress, anxiety, or depression. It is important to seek psychological support if needed.
- Diabetes: Damage to the insulin-producing cells in the pancreas may lead to diabetes, requiring careful management.
- Increased Risk of Pancreatic Cancer: Chronic inflammation increases the risk of pancreatic cancer, making regular monitoring essential.
Managing Chronic Pancreatitis
Managing chronic pancreatitis involves lifestyle modifications, medication adherence, and regular medical follow-ups. People who avoid alcohol and smoking tend to experience fewer symptoms and complications, leading to a better quality of life and potentially a longer lifespan. If you experience mental health challenges or struggle with chronic pain, consult your GP for support options, such as counseling or therapy, to help you manage the physical and emotional impact of the condition.
Symptoms of chronic pancreatitis
Chronic pancreatitis is characterized by persistent inflammation of the pancreas, leading to long-term damage and symptoms that can significantly impact quality of life. The primary symptom is recurrent abdominal pain, often accompanied by digestion problems over time.
Symptoms of Chronic Pancreatitis
Abdominal Pain
- Primary Symptom: The hallmark of chronic pancreatitis is repeated episodes of abdominal pain.
- Location: The pain typically develops in the middle or left side of the abdomen and can sometimes radiate to the back.
- Nature of Pain: It has been described as a burning or shooting sensation, which may come and go, but can persist for hours or even days in some cases.
- Pain Triggers: Although pain can occasionally be triggered by eating, there is often no clear cause for its onset.
- Frequency and Severity: As the condition progresses, episodes of pain may become more frequent and severe. For some individuals, a constant mild to moderate pain may develop in between severe episodes, particularly among those who continue to drink alcohol following their diagnosis.
- Nausea and Vomiting: Some individuals experience nausea and vomiting during pain episodes.
Advanced Symptoms
Over time, chronic pancreatitis can lead to additional symptoms as the pancreas loses its ability to produce essential digestive enzymes. These include:
- Smelly, Greasy Stools: The inability to break down fats and certain proteins may cause stools that are greasy, foul-smelling, and difficult to flush.
- Weight Loss: Difficulty digesting food and reduced appetite can lead to significant weight loss.
- Loss of Appetite: People may experience reduced interest in eating.
- Jaundice: Yellowing of the skin and eyes, which occurs due to bile buildup, can be a sign of advanced disease.
- Diabetes Symptoms: Chronic damage to the pancreas can eventually impair insulin production, leading to symptoms such as excessive thirst, frequent urination, and fatigue.
- Ongoing Nausea and Vomiting: Persistent symptoms may develop as the disease advances.
When to Seek Medical Advice
- Severe Pain: Always consult with your GP if you experience severe abdominal pain, as it indicates a potential issue that requires attention.
- Jaundice Symptoms: Yellowing of the skin and eyes should prompt a visit to your GP, as it may signal underlying problems with your digestive system.
- Persistent Vomiting: If you experience continuous vomiting, it is important to seek medical advice promptly.
Early diagnosis and management of chronic pancreatitis can help alleviate symptoms, slow disease progression, and reduce the risk of complications such as diabetes and malnutrition. Lifestyle changes, particularly abstaining from alcohol and smoking, may help reduce symptom severity for some individuals.
Causes of chronic pancreatitis
Chronic pancreatitis is a condition marked by persistent inflammation of the pancreas, which can lead to permanent damage over time. The inflammation can result from a variety of causes, many of which affect the digestive enzymes and hormones produced by the pancreas. Below are the key causes and contributing factors of chronic pancreatitis:
1. Alcohol Consumption
- Heavy and Prolonged Drinking: The majority of chronic pancreatitis cases are linked to excessive alcohol consumption over many years. Repeated alcohol-induced episodes of acute pancreatitis—a sudden inflammation of the pancreas—can eventually lead to chronic damage if the individual continues drinking.
- Mechanism: Chronic inflammation due to excessive alcohol use damages pancreatic tissue over time, resulting in fibrosis (scar tissue formation) and a permanent loss of function.
- Risk: Regular alcohol consumption increases the risk, but not all individuals who drink heavily will develop the condition, suggesting that other factors, such as genetic predisposition, may play a role.
2. Idiopathic Chronic Pancreatitis
- Unknown Causes: For about 30% of individuals with chronic pancreatitis, the underlying cause remains unidentified. This form is referred to as ‘idiopathic’ chronic pancreatitis. Research is ongoing to determine any genetic, environmental, or lifestyle factors that might contribute to these cases.
3. Genetic Causes
- Inherited Mutations: Some cases are linked to inherited genetic mutations. Genes implicated include PRSS1 and SPINK-1, which affect how the pancreas functions and responds to damage.
- Genetic Susceptibility to Alcohol: Genetic mutations may also influence how susceptible an individual’s pancreas is to the harmful effects of alcohol.
- CFTR Gene Mutations: Mutations in the CFTR gene—which is also responsible for cystic fibrosis—can contribute to chronic pancreatitis in a small number of cases.
4. Immune System-Related Causes (Autoimmune Pancreatitis)
- Autoimmune Attack on the Pancreas: In rare cases, the immune system mistakenly attacks the pancreas, leading to inflammation and chronic damage. This form is known as autoimmune pancreatitis.
- Related Conditions: People with autoimmune pancreatitis often have other autoimmune conditions, such as ulcerative colitis or Crohn’s disease, which cause inflammation in the digestive system.
5. Other Rare Causes
- Injury to the Pancreas: Trauma or injury to the pancreas can lead to chronic inflammation and damage.
- Blocked or Narrowed Pancreatic Ducts: Blockages or narrowing of the ducts that carry digestive enzymes from the pancreas can cause buildup and inflammation, leading to chronic damage.
- Smoking: Smoking is considered a significant risk factor and can contribute to the development of chronic pancreatitis, particularly in individuals with other underlying risk factors such as heavy alcohol use.
- Radiotherapy: Exposure to radiotherapy in the abdominal area can lead to chronic pancreatic inflammation in some cases.
Reducing Risk Factors
- Avoid Alcohol and Smoking: Quitting alcohol and smoking is essential for reducing the risk of chronic pancreatitis and its complications.
- Manage Underlying Conditions: Proper management of autoimmune conditions and maintaining overall digestive health can also play a role in reducing the risk of chronic pancreatitis.
Understanding the underlying causes of chronic pancreatitis is key to managing symptoms and preventing further pancreatic damage. Those with a family history of the condition or with significant risk factors should speak with a healthcare provider for assessment and possible genetic testing.
Diagnosing Chronic Pancreatitis
Chronic pancreatitis is a condition that can be challenging to diagnose, often requiring a series of specialized tests and imaging studies. Diagnosis primarily focuses on examining the pancreas for signs of inflammation and long-term damage. If you present with symptoms of chronic pancreatitis, such as abdominal pain, digestive issues, or greasy stools, your GP will start by taking a detailed history and conducting a physical examination. If chronic pancreatitis is suspected, they will refer you to a hospital for further diagnostic tests.
Key Diagnostic Tests for Chronic Pancreatitis
Stool Sample Analysis:
- This test checks for the presence of undigested fat in the stool, which is a common sign of malabsorption caused by pancreatic dysfunction. It may reveal greasy, foul-smelling stools indicative of impaired digestion.
Imaging Tests:
- Ultrasound Scan:
- An ultrasound uses sound waves to create images of the internal organs, including the pancreas. It helps detect inflammation, scarring, or calcifications (hardened deposits) in the pancreas.
- Computerised Tomography (CT) Scan:
- A CT scan combines a series of X-ray images taken from different angles to create a more detailed, three-dimensional view of the pancreas and surrounding structures. It can reveal structural damage, cysts, or calcifications associated with chronic pancreatitis.
- Magnetic Resonance Cholangiopancreatography (MRCP):
- An MRCP uses a magnetic resonance imaging (MRI) scanner to generate highly detailed images of the pancreas, gallbladder, and bile ducts. A contrast agent may be injected to enhance the visibility of these structures, helping detect any blockages, stones, or abnormalities that could be contributing to your symptoms.
- Ultrasound Scan:
Endoscopic Ultrasonography (EUS):
- This procedure involves inserting a thin, flexible telescope (endoscope) equipped with an ultrasound probe through your mouth and into your stomach. By positioning the ultrasound probe close to the pancreas, this test provides highly detailed images of the pancreas and surrounding tissues.
- You’ll typically be given a sedative to keep you comfortable during the procedure.
Biopsy:
- In cases where pancreatic cancer is a potential concern, a biopsy may be recommended. Symptoms like jaundice (yellowing of the skin and eyes) and unexplained weight loss can overlap with chronic pancreatitis and necessitate ruling out cancer.
- A biopsy involves removing a small sample of pancreatic tissue for microscopic examination. The sample may be taken using a long, thin needle guided by ultrasound or CT imaging, or it may be obtained during an endoscopic ultrasonography procedure.
The Importance of Accurate Diagnosis
- Chronic pancreatitis can often mimic other conditions, including pancreatic cancer, gallbladder disease, or digestive disorders. Accurate diagnosis through a combination of imaging tests and biopsies ensures that appropriate treatment can be provided and any underlying causes or complications are addressed effectively.
If you experience severe abdominal pain, unexplained weight loss, jaundice, or persistent digestive symptoms, it is essential to seek medical advice promptly for an accurate diagnosis and timely management.
Treating Chronic Pancreatitis
Chronic pancreatitis is a long-term condition characterized by persistent inflammation of the pancreas. While there is no cure, treatment focuses on managing symptoms, minimizing damage to the pancreas, and improving quality of life.
1. Lifestyle Changes
Avoiding Alcohol:
- The most critical step in managing chronic pancreatitis is to stop drinking alcohol, regardless of whether alcohol is the cause. Continuing to drink can worsen symptoms and increase the likelihood of severe complications.
- People with alcohol-related chronic pancreatitis who struggle with dependence can seek help through counseling, self-help groups like Alcoholics Anonymous, or medications like acamprosate to reduce cravings.
Quitting Smoking:
- Smoking cessation is essential, as smoking can worsen the progression of chronic pancreatitis. Treatments such as nicotine replacement therapy (NRT) or medications like bupropion can increase the chances of successfully quitting.
- Consult your GP or utilize NHS Stop Smoking support services for assistance.
Dietary Changes:
- Chronic pancreatitis can impair digestion. A low-fat, high-protein, high-calorie diet with fat-soluble vitamin supplements may be recommended. Consult with a dietitian before making changes.
2. Medications
Enzyme Supplements:
- Pancreatic enzyme supplements contain artificial enzymes that aid digestion and help the body absorb nutrients. Side effects may include diarrhea, constipation, nausea, or stomach pain.
Steroid Medications:
- For autoimmune-related chronic pancreatitis, corticosteroids can relieve inflammation, but long-term use may cause osteoporosis, weight gain, and other side effects.
Pain Relief:
- Managing pain is crucial. Options include:
- Mild Painkillers: Start with paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. Long-term use of NSAIDs may require proton pump inhibitors (PPIs) to reduce stomach ulcer risk.
- Stronger Painkillers: If mild painkillers are ineffective, opiate-based painkillers like codeine or tramadol may be used, though they can cause constipation, nausea, and drowsiness.
- For severe pain, stronger opiates like morphine or pethidine may be needed temporarily. Amitriptyline, originally for depression, can also help manage pain.
- Nerve Blocks: Temporary relief may be provided by a nerve block injection to stop pain signals from the pancreas.
3. Hospitalization for Severe Episodes
- If the pancreas becomes acutely inflamed, hospitalization may be required for IV fluids and oxygen therapy.
4. Surgical Interventions
Endoscopic Surgery:
- Stones blocking the pancreatic duct may be treated with endoscopic surgery and lithotripsy (shock waves to break stones into smaller pieces).
Pancreas Resection:
- If inflammation affects specific areas of the pancreas, surgical removal of the affected parts (pancreas resection) may reduce pain.
Total Pancreatectomy:
- In severe cases, total removal of the pancreas may be necessary. Autologous pancreatic islet cell transplantation (APICT) may follow, where insulin-producing cells are transplanted into the liver. This can reduce the need for insulin therapy in the short term.
5. Managing Complications
- Diabetes Management: Chronic pancreatitis can lead to diabetes, requiring insulin therapy.
- Mental Health Support: Chronic pain can lead to stress, anxiety, and depression. Talking to a GP, counselor, or support group can help.
Effective treatment of chronic pancreatitis involves collaboration with healthcare professionals to create a personalized care plan and commitment to lifestyle modifications, including alcohol and smoking cessation, proper diet, and managing pain and complications through medications or surgery as needed.
Complications of Chronic Pancreatitis
Chronic pancreatitis is a long-term condition that can lead to a range of complications, mainly due to persistent inflammation and damage to the pancreas. These complications can affect both the physical and psychological health of those living with the condition.
1. Psychological Effects
Chronic pain and persistent health challenges can severely impact mental health. Studies have shown that up to 94% of individuals with chronic pancreatitis experience pain, and many also struggle with psychological difficulties such as:
- Stress, anxiety, and depression: Around one in seven people with chronic pancreatitis may experience psychological or emotional challenges due to the ongoing nature of the illness.
- Seeking Support: It is important to talk to a GP if you are experiencing emotional difficulties. Treatments such as counseling, therapy, and medication can help improve symptoms. Connecting with support groups for chronic pancreatitis can also be helpful in reducing isolation and stress through shared experiences and understanding.
2. Diabetes
- Prevalence: Approximately one-third of people with chronic pancreatitis eventually develop diabetes, often years after the initial diagnosis. In some cases, it may take up to 20 years for diabetes to appear.
- Causes: Diabetes occurs when the damaged pancreas loses its ability to produce insulin, a hormone essential for regulating blood sugar levels.
- Symptoms of Diabetes:
- Feeling very thirsty
- Frequent urination, especially at night
- Extreme fatigue
- Weight loss and muscle wasting
- Treatment: Diabetes resulting from chronic pancreatitis typically requires regular insulin injections to replace the body’s natural insulin.
3. Pseudocysts
- Description: Pseudocysts are fluid-filled sacs that form on the surface of the pancreas. They affect about 10% of people with chronic pancreatitis.
- Symptoms: Pseudocysts may not cause symptoms, but when they do, symptoms can include:
- Bloating
- Indigestion
- Dull abdominal pain
- Treatment:
- Small pseudocysts that do not cause symptoms may not need treatment, as they can resolve independently.
- Larger pseudocysts (greater than 6cm) or symptomatic pseudocysts may need to be drained to prevent rupture or infection. Fluid can be drained using a needle through the skin or an endoscopic procedure. In some cases, part of the pancreas may need to be surgically removed using laparoscopic techniques (laparoscopic distal pancreatectomy).
4. Pancreatic Cancer
- Increased Risk: Chronic pancreatitis slightly raises the risk of developing pancreatic cancer, but the overall risk remains relatively low. For every 100 people with chronic pancreatitis, only 1 or 2 may develop pancreatic cancer.
- Symptoms of Pancreatic Cancer: The initial signs of pancreatic cancer may mimic those of chronic pancreatitis and include:
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain
- Unexplained weight loss
Monitoring and Early Detection
- Regular Check-Ups: People with chronic pancreatitis should have regular medical check-ups to monitor for potential complications, such as diabetes or cancer, and to manage symptoms effectively.
- Lifestyle Changes: Avoiding alcohol, stopping smoking, and adhering to dietary recommendations can help manage symptoms and reduce the risk of complications.
Living with chronic pancreatitis can be challenging, but appropriate medical care, lifestyle adjustments, and psychological support can improve quality of life and help manage complications effectively.

 4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all
4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all



