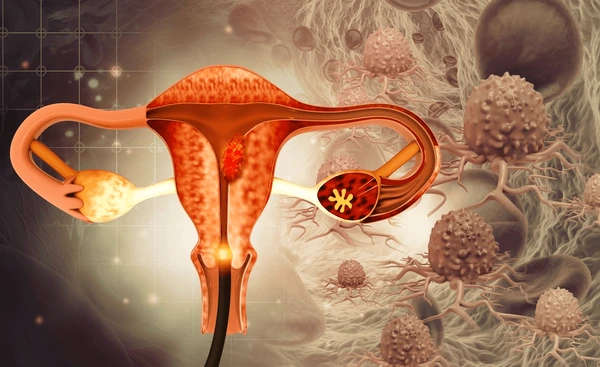
About cervical cancer
Cervical cancer is a form of cancer that develops in the cervix, the lower part of the uterus connecting to the vagina. It often progresses slowly, starting as precancerous changes known as cervical intraepithelial neoplasia (CIN), which may eventually turn into cancer if not detected and treated early.
Symptoms of Cervical Cancer
Cervical cancer in its early stages may not cause any noticeable symptoms. When symptoms do occur, they may include:
- Unusual vaginal bleeding: This can happen after sexual intercourse, between menstrual periods, or after menopause.
- Pain during sexual intercourse.
- Vaginal discharge: May be watery, bloody, or have a foul odor.
- Pelvic pain: Can range from a dull ache to severe discomfort.
- Pain during urination or increased frequency.
Screening for Cervical Cancer
- Cervical Screening (Smear Test/Pap Test): Offered routinely every five years for those aged 25 to 64 in Scotland and other parts of the UK, or more frequently if test results indicate the need for closer monitoring.
- HPV Testing: Most cervical cancers are caused by certain strains of the human papilloma virus (HPV). Testing for high-risk HPV can help detect early changes.
Causes and Risk Factors
- Human Papilloma Virus (HPV): Nearly all cervical cancer cases are linked to HPV infection, particularly strains 16 and 18, which account for 70% of cases. HPV is sexually transmitted.
- Risk Factors:
- Multiple sexual partners and early sexual activity increase the risk of HPV infection.
- Smoking weakens the immune system, reducing the body’s ability to fight HPV.
- Weakened immune system due to conditions like HIV/AIDS or immunosuppressant drugs.
- Long-term use of oral contraceptives and having many full-term pregnancies have also been linked to increased risk.
Preventing Cervical Cancer
- HPV Vaccination: Available for girls and boys, usually administered between the ages of 12 and 13 to protect against high-risk HPV strains.
- Regular Screening: Routine cervical screening helps detect abnormal changes in cervical cells before they turn cancerous.
- Practicing Safe Sex: Using condoms reduces the risk of HPV transmission, although it doesn’t eliminate it entirely as the virus can spread through skin contact.
- Quitting Smoking: Reduces the risk of cervical cancer and improves overall health.
Diagnosing Cervical Cancer
- Cervical Screening Test (Smear Test): Detects precancerous changes in the cervix.
- Colposcopy: If abnormal cells are found, a colposcopy may be performed to take a closer look at the cervix.
- Biopsy: Removal of a small tissue sample for laboratory analysis.
- Imaging Tests: CT scans, MRI, or PET scans may be used to assess the spread and staging of the cancer.
Staging of Cervical Cancer
- Stage 1: Cancer confined to the cervix.
- Stage 2: Cancer has spread beyond the cervix to nearby areas but hasn’t reached the pelvic wall or lower part of the vagina.
- Stage 3: Cancer has spread to the lower vagina, pelvic wall, or nearby lymph nodes.
- Stage 4: Cancer has spread to other organs, such as the bladder, rectum, or distant organs like the lungs.
Treating Cervical Cancer
- Surgery:
- Cone Biopsy: Removes a small, cone-shaped section of abnormal tissue.
- Hysterectomy: Removal of the uterus, and in some cases, other surrounding tissues.
- Trachelectomy: Preserves the uterus, removing the cervix and surrounding tissue, allowing for future pregnancies.
- Radiotherapy: Often used alongside or instead of surgery for early-stage cancer or in combination with chemotherapy for more advanced stages.
- Chemotherapy: Uses drugs to destroy cancer cells and is often combined with radiotherapy.
- Targeted Therapy and Immunotherapy: These newer treatments may be used for advanced cases or in clinical trials.
Complications of Treatment
- Infertility: Can result from surgery or radiotherapy.
- Early Menopause: Removal of the ovaries or damage from treatment may trigger menopause.
- Bladder and Bowel Issues: Radiotherapy can cause long-term changes to bowel and bladder function.
- Emotional Impact: Coping with cancer can be challenging emotionally, requiring support.
Outlook for Cervical Cancer Patients
Prognosis depends on the cancer’s stage at diagnosis:
- Stage 1: 80-99% survival for at least five years.
- Stage 2: 60-90% survival for at least five years.
- Stage 3: 30-50% survival for at least five years.
- Stage 4: Around 20% survival for at least five years.
Living with Cervical Cancer
Managing cervical cancer involves ongoing care, emotional support, and regular check-ups to monitor for recurrence. Support groups, counseling, and talking with healthcare providers can be valuable in helping women and their families cope with the challenges of living with and overcoming cervical cancer.
Symptoms of cervical cancer
Cervical cancer often doesn’t cause noticeable symptoms in its early stages, which is why attending routine cervical screening (smear tests) is crucial for early detection. When symptoms do appear, they may include:
1. Unusual Vaginal Bleeding
- Postcoital bleeding: Bleeding after sexual intercourse.
- Bleeding between periods: Any unexpected bleeding outside of your regular menstrual cycle.
- Postmenopausal bleeding: Bleeding after you have gone through menopause, when your periods have stopped.
2. Other Symptoms
- Pain and discomfort during sex (dyspareunia).
- Unusual vaginal discharge: This may be watery, have a foul smell, or be tinged with blood.
Advanced Cervical Cancer Symptoms
When cervical cancer spreads beyond the cervix to surrounding tissues and organs, additional symptoms may develop:
- Pelvic or abdominal pain.
- Constipation.
- Blood in urine (haematuria).
- Urinary incontinence or loss of bladder control.
- Bone pain.
- Swelling in one leg: This can occur if cancerous tissue blocks lymphatic drainage.
- Severe pain in the side or back (hydronephrosis): Caused by swelling of the kidneys.
- Changes in bladder and bowel habits.
- Loss of appetite and unexplained weight loss.
- Tiredness and low energy levels.
When to Seek Medical Advice
It’s important to consult your GP if you experience:
- Bleeding after sex (postcoital bleeding).
- Bleeding outside of your normal periods.
- New bleeding after menopause.
Vaginal bleeding is a common issue and may not necessarily indicate cervical cancer, but it is a symptom that should always be investigated further by a healthcare professional to rule out any serious conditions, including cervical cancer.
Causes of Cervical Cancer
Cervical cancer develops when healthy cells in the cervix undergo genetic mutations that cause abnormal growth and reproduction, potentially leading to the formation of a cancerous tumor. One of the primary causes of cervical cancer is infection with the human papilloma virus (HPV), which is a group of viruses spread through sexual contact.
How Cervical Cancer Develops
- DNA Mutations: Cancer develops when mutations alter the DNA in cells, affecting their growth and reproduction instructions. This leads to uncontrolled cell growth and the formation of a tumor.
- HPV Infection:
- HPV Types: There are over 100 types of HPV, and many are harmless. However, around 15 types are considered high-risk for cervical cancer. HPV types 16 and 18 are responsible for approximately 70% of cervical cancer cases.
- Transmission: HPV is spread through sexual contact, including vaginal, anal, and oral sex, as well as skin-to-skin contact in the genital area. The virus often causes no symptoms and can be present for years before causing changes to cervical cells.
- High-Risk HPV Types and Cancer: High-risk HPV types may introduce genetic material into the cells of the cervix, disrupting their normal function and leading to abnormal cell changes and potentially cancer over time.
Pre-Cancerous Conditions: Cervical Intraepithelial Neoplasia (CIN)
- CIN and CGIN (Cervical Glandular Intraepithelial Neoplasia): Before cervical cancer develops, cells in the cervix often show changes referred to as CIN or CGIN, which are pre-cancerous conditions. They don’t pose an immediate threat but may develop into cancer over many years.
- Progression: The progression from HPV infection to CIN/CGIN to cervical cancer can take 10 to 20 years. Cervical screening helps detect and treat CIN or CGIN early, reducing the risk of cancer development.
Additional Risk Factors for Cervical Cancer
While HPV infection is necessary for almost all cases of cervical cancer, other factors can increase the risk:
- Smoking: Women who smoke are twice as likely to develop cervical cancer. Chemicals in tobacco may damage the cervix’s cells and make them more susceptible to HPV.
- Weakened Immune System: A compromised immune system (e.g., due to HIV/AIDS or taking immunosuppressive drugs) makes it harder to fight HPV infections.
- Long-Term Use of Oral Contraceptives: Taking the contraceptive pill for more than five years doubles the risk of cervical cancer. The exact reason is unclear.
- Childbirth: Women who have had multiple children are at a higher risk, potentially due to hormonal changes during pregnancy that make the cervix more susceptible to HPV.
- Family History: Having a family history of cervical cancer may increase risk.
Spread of Cervical Cancer
If untreated, cervical cancer can spread:
- Locally: It may grow downward into the vagina and pelvic muscles or upward to the ureters (tubes connecting kidneys and bladder).
- Distant Spread (Metastasis): It can affect the bladder, rectum, liver, lungs, and bones.
- Lymphatic System: Cancerous cells may spread through the lymphatic system to lymph nodes near the cervix, chest, and abdomen.
Early diagnosis and treatment are key to controlling the progression and spread of cervical cancer. Regular cervical screenings and HPV vaccinations play critical roles in prevention.
Diagnosing Cervical Cancer
If cervical cancer is suspected, you will be referred to a gynecologist who specializes in conditions of the female reproductive system. Referrals are typically made if cervical screening test results suggest cell abnormalities or if you experience symptoms such as abnormal vaginal bleeding or growths noticed during a GP examination.
Initial Assessment and Testing
- Cervical Screening Abnormalities: Not all abnormalities detected in cervical screening mean cancer is present; further examination is needed.
- Sexually Transmitted Infection Testing: Since some STIs, like chlamydia, can cause abnormal bleeding, your GP may recommend testing for these first.
Colposcopy
A colposcopy is often the first step after an abnormal screening or concerning symptoms. This procedure involves using a colposcope, a small microscope with a light source, to closely examine the cervix for abnormalities. During the procedure, a small tissue sample (biopsy) may be taken for laboratory analysis to check for cancerous cells.
Cone Biopsy
For a more detailed examination, a cone biopsy may be performed. This involves removing a small, cone-shaped section of the cervix to examine under a microscope for cancerous cells. This procedure is done in a hospital, usually under local anesthesia. It may cause vaginal bleeding for up to four weeks and period-like pain.
Further Testing for Cancer Spread
If the biopsy indicates cervical cancer, further tests may be done to assess whether it has spread:
- Pelvic Examination under General Anesthetic: The womb, vagina, rectum, and bladder are examined for signs of cancer.
- Blood Tests: These check liver, kidney, and bone marrow function.
- Imaging Tests:
- CT Scan: Creates detailed 3D images of the inside of the body, identifying tumors and their spread.
- MRI Scan: Uses magnetic fields and radio waves for detailed internal images.
- Chest X-ray: Checks for potential spread to the lungs.
- PET Scan: Involves injecting a mildly radioactive substance to highlight cancerous tissues, often combined with a CT scan for detailed imaging.
Staging Cervical Cancer
Once testing is complete, your gynecologist will determine the stage of the cancer, which measures its spread:
- Stage 0 (Pre-Cancer): No cancerous cells, but there are changes (CIN or carcinoma in situ) that may lead to cancer.
- Stage 1: Cancer is confined to the cervix.
- Stage 2: Cancer has spread outside the cervix but not to the pelvic wall or lower vagina.
- Stage 3: Cancer has spread to the lower vagina and/or pelvic wall.
- Stage 4: Cancer has spread to nearby organs, such as the bowel, bladder, or distant organs like the lungs.
Accurate staging is crucial for guiding treatment options and predicting outcomes. Early diagnosis and intervention improve the chances of successful treatment.
Treating Cervical Cancer
The treatment for cervical cancer depends on the stage of the cancer, the location of the tumor, and whether it has spread. Treatment is often planned and carried out by a multidisciplinary team (MDT) of specialists who work together to create the best treatment plan for each individual. Treatment options include surgery, radiotherapy, chemotherapy, or a combination of these treatments.
1. Early-Stage Cervical Cancer
- Surgery is often recommended to remove part or all of the womb (uterus) and sometimes nearby lymph nodes.
- Radiotherapy, either alone or combined with surgery, is another option for early-stage cancer.
2. Advanced Cervical Cancer
- Radiotherapy combined with chemotherapy (chemoradiation) is the most common treatment approach.
- Surgery may sometimes be considered but is less commonly used than for early-stage cancer.
Surgical Options for Cervical Cancer
- Large Loop Excision of the Transformation Zone (LLETZ):
- This procedure removes abnormal cells using a fine wire loop heated with an electric current.
- Cone Biopsy:
- This involves removing a cone-shaped section of the cervix containing abnormal cells.
- Radical Trachelectomy:
- Removes the cervix, surrounding tissue, and upper part of the vagina but leaves the womb intact. This procedure preserves fertility and may be considered if cancer is diagnosed at an early stage.
- Hysterectomy:
- Removes the womb and cervix and sometimes the ovaries and fallopian tubes. There are two types:
- Simple Hysterectomy (removes cervix and womb).
- Radical Hysterectomy (removes cervix, womb, surrounding tissue, and nearby lymph nodes).
- Pelvic Exenteration:
- This is a major operation performed when cervical cancer returns and involves removing multiple organs in the pelvic region, followed by creating openings (stomas) to pass urine and feces.
- Removes the womb and cervix and sometimes the ovaries and fallopian tubes. There are two types:
Radiotherapy
Radiotherapy can be used alone or in combination with surgery and chemotherapy. It works by directing high-energy waves at cancer cells to destroy them.
- External Radiotherapy: A machine directs radiation beams at the pelvis.
- Internal Radiotherapy (Brachytherapy): Radioactive implants are placed near the tumor inside the vagina and cervix.
- Side Effects: Common side effects include diarrhea, pain when urinating, vaginal bleeding, fatigue, nausea, sore skin, narrowing of the vagina, infertility, and damage to the bladder or bowel. Most side effects gradually improve after treatment ends, though some may be long-lasting.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or prevent them from multiplying. It is usually given through an intravenous drip in cycles and can be combined with radiotherapy (chemoradiation) or used alone for advanced cancer.
- Common Medications: Cisplatin is commonly used, often in combination with other chemotherapy drugs.
- Side Effects: Include nausea, vomiting, diarrhea, fatigue, reduced blood cell counts (anemia), increased risk of infection, mouth ulcers, loss of appetite, and sometimes hair loss.
Follow-Up Care
After completing treatment, follow-up care is essential to monitor for any signs of recurrence and to manage side effects.
- Regular Appointments: Usually every four months for the first two years, and then every six to twelve months for another three years.
- Examinations and Tests: Include physical exams of the vagina and cervix, and additional testing or biopsies if any abnormalities are detected.
Palliative Care
If a complete cure isn’t possible, palliative care focuses on slowing the progression of cancer, managing symptoms, and improving quality of life.
Support and Fertility Preservation
For those concerned about fertility, options such as egg or embryo freezing may be available before treatment. The MDT will discuss fertility-preserving options, such as ovarian transposition or alternative fertility treatments, based on individual circumstances.
Cervical cancer treatment can have a significant impact on physical and emotional well-being. Support groups, counseling, and specialist care can help manage the effects of treatment and provide necessary support during and after recovery.
Complications of Cervical Cancer
Cervical cancer complications can arise from the disease itself or as side effects of treatment. Managing these complications is an essential part of the care plan.
Complications Related to Treatment
Early Menopause
- Cause: Triggered if ovaries are surgically removed or damaged by radiotherapy.
- Symptoms:
- Irregular or stopped periods
- Hot flushes
- Vaginal dryness
- Loss of libido
- Mood changes
- Stress incontinence
- Night sweats
- Osteoporosis (thinning of bones)
- Management: Hormone Replacement Therapy (HRT) can help relieve symptoms by stimulating the production of oestrogen and progesterone.
Narrowing of the Vagina
- Cause: Commonly due to radiotherapy.
- Treatment:
- Hormonal Creams: To increase moisture in the vagina.
- Vaginal Dilators: Tampon-shaped devices that help maintain or increase vaginal flexibility. Regular use over several months may be recommended.
- Sexual Activity: Regular sex can help reduce discomfort over time. Emotional readiness is important, and resources like Macmillan Cancer Support offer guidance on intimacy after treatment.
Lymphoedema
- Cause: Swelling due to disruption of the lymphatic system, often after pelvic lymph node removal.
- Management: Exercises, massage, specially designed compression garments, and bandages can reduce swelling.
Emotional Impact
- Common Reactions: The journey can involve anxiety, sadness, depression, and feelings of isolation.
- Management: Support groups, talking therapies such as Cognitive Behavioral Therapy (CBT), and antidepressant medication may help. Healthcare professionals and support groups like Macmillan Cancer Support offer guidance.
Complications Due to Advanced Cervical Cancer
Pain
- Cause: Cancer spreading to nerves, bones, or muscles.
- Treatment:
- Painkillers (from paracetamol to morphine) tailored to individual needs.
- Short-term radiotherapy may provide relief.
- Macmillan nurses offer specialized pain management.
Kidney Failure
- Cause: Cancer may press on the ureters, blocking urine flow, leading to hydronephrosis and potential kidney damage.
- Treatment:
- Percutaneous Nephrostomy: Tube insertion to drain urine.
- Stents: Small tubes to widen ureters.
Blood Clots
- Risk Factors: Increased due to cancer, prolonged rest, or tumor pressure on pelvic veins.
- Symptoms: Pain, swelling, tenderness in legs, heavy ache, warm/red skin.
- Treatment: Blood-thinning medications (heparin, warfarin) and compression garments.
Bleeding
- Cause: Cancer spreading to the vagina, bowel, or bladder, causing damage and bleeding.
- Treatment:
- Tranexamic Acid: To encourage clotting.
- Radiotherapy: For controlling bleeding.
- Surgery or Vaginal Packing may be required for severe cases.
Fistula Formation
- Cause: Abnormal channels may form between the bladder/vagina or rectum/vagina due to cancer.
- Treatment:
- Surgery: If possible.
- Medication/Creams: To manage symptoms if surgery isn’t viable.
Vaginal Discharge
- Cause: Tissue breakdown, bacterial infection, or fistula formation.
- Treatment: Antibacterial gels like metronidazole and charcoal-containing garments to absorb odor.
Palliative Care
If a cure is not possible, palliative care focuses on symptom relief and quality of life. It involves:
- Managing Symptoms: Pain relief, emotional and social support.
- Support Services: Offered by Macmillan Cancer Support, Marie Curie, and Hospice UK, among others, providing at-home care, hospice support, and guidance.
Palliative care also supports psychological, social, and spiritual needs for both patients and their families.
Living with Cervical Cancer
Living with cervical cancer can impact daily life in many ways, from physical recovery to emotional and practical challenges. Here’s an overview of how it may affect your life and tips on managing these challenges:
Recovery from Surgery
- Radical Hysterectomy: Most women with cervical cancer undergo this major operation. Recovery typically takes 6 to 12 weeks, during which:
- Avoid strenuous activities: No heavy lifting, such as carrying children or heavy shopping.
- Driving: Usually, you will be unable to drive for 3 to 8 weeks post-surgery.
- Work: Many women require 8 to 12 weeks off work for recovery. It’s essential to follow your doctor’s recommendations regarding when to resume normal activities.
Fatigue
- Treatments like chemotherapy and radiotherapy can cause severe fatigue. You may need to adjust your normal routine and take more rest.
- Ask for help: Reach out to family, friends, or your local authority for practical help with tasks or chores.
Work and Employment Rights
- Work adjustments: You may be able to continue working, but modifications might be necessary.
- Flexibility: Your employer must make “reasonable adjustments” to accommodate your needs, such as flexible working hours or time off for appointments.
- Legal protection: Under the Equality Act 2010, employers cannot discriminate based on illness.
- Support: Communicate with HR or a union representative if you face difficulties with your employer. Macmillan Cancer Support offers additional advice on work and cancer.
Financial Support
- Statutory Sick Pay: Available if you cannot work due to illness.
- Employment and Support Allowance: Available if you are unable to work and do not have a job.
- Carer’s Allowance: Available if you are caring for someone with cancer.
- Other benefits: Available based on your household income and family situation.
- Advice: Speak to a hospital social worker for guidance on financial support.
Sexual Health and Intimacy
- Resuming Sex: Safe to resume a normal sex life a few weeks after treatment, once your body has healed.
- Precautions during Chemotherapy: Male partners should use condoms, as it is unclear how chemotherapy may affect partners.
- Side Effects: Vaginal dryness and narrowing may occur after treatment, making sex uncomfortable. Treatments, including vaginal dilators, can help.
- Emotional Challenges: It is natural to feel apprehensive. Discuss any concerns with your healthcare team, as they can provide support and resources.
Practical Tips
- Plan for Recovery: Gradually increase your activity levels.
- Seek Support: Join local or online support groups for emotional and practical advice.
- Communicate Openly: Talk to your healthcare team about any physical or emotional concerns.
- Keep Track of Finances: Explore financial assistance early to avoid stress.
Living with cervical cancer can be challenging, but support is available to help you manage treatment, recovery, work, relationships, and your overall quality of life.
Preventing Cervical Cancer
While it’s not possible to entirely prevent cervical cancer, there are several measures you can take to significantly reduce your risk.
1. Safer Sex Practices
- Use Protection: Most cervical cancer cases are linked to human papillomavirus (HPV) infections, which are spread through unprotected sexual contact. Condoms and dental dams can help reduce the risk of HPV transmission.
- HPV Transmission Beyond Penetrative Sex: HPV can be transmitted through skin-to-skin contact in the genital area, including during oral sex or sharing sex toys. Practicing safe sex in all scenarios can help reduce transmission risk.
- Sexual Partners and Timing: While having multiple sexual partners or starting sexual activity at an early age can increase your risk of HPV infection, anyone can develop cervical cancer. Safe practices and regular health checks are important.
2. Regular Cervical Screening (Smear Tests)
- Routine Screening: In Scotland, cervical screening is offered to anyone with a cervix aged 25 to 64 every five years. This helps detect abnormal changes in cervical cells that may lead to cancer.
- Keep Contact Information Updated: Ensure your GP has your correct address and contact details to avoid missing screening invitations.
- Screening Despite HPV Vaccination: Even if you’ve been vaccinated, it’s crucial to continue attending cervical screening tests, as the vaccine does not protect against all types of cervical cancer.
- Report Symptoms: Always consult your GP if you experience symptoms like unusual vaginal bleeding, regardless of recent screening results.
3. Cervical Cancer Vaccination
- HPV Vaccine: The NHS offers Gardasil, which protects against four types of HPV, including HPV16 and HPV18—responsible for most cervical cancer cases. It also protects against genital warts.
- Routine Vaccination: The vaccine is routinely offered to girls aged 12 to 13 years through the childhood immunisation programme, with three doses administered over six months.
- Screening Post-Vaccination: Vaccination doesn’t guarantee immunity from all cervical cancer strains, so regular screening remains essential.
4. Avoid Smoking
- Tobacco and HPV: Smoking weakens your immune system’s ability to clear HPV infections, increasing the risk of cervical cancer.
- Quitting Support: Contact Quit Your Way Scotland at 0800 84 84 84 for expert advice and support on quitting smoking. Your GP can also provide prescriptions for medications to ease withdrawal symptoms.
- Resources: Explore tools and resources like Nicotine Replacement Therapy (NRT) and behavioral support to aid in quitting smoking.
By combining these preventative measures—safer sex, regular screening, vaccination, and quitting smoking—you can significantly reduce your risk of developing cervical cancer. Regular health check-ups and awareness of symptoms are key to early detection and better outcomes.