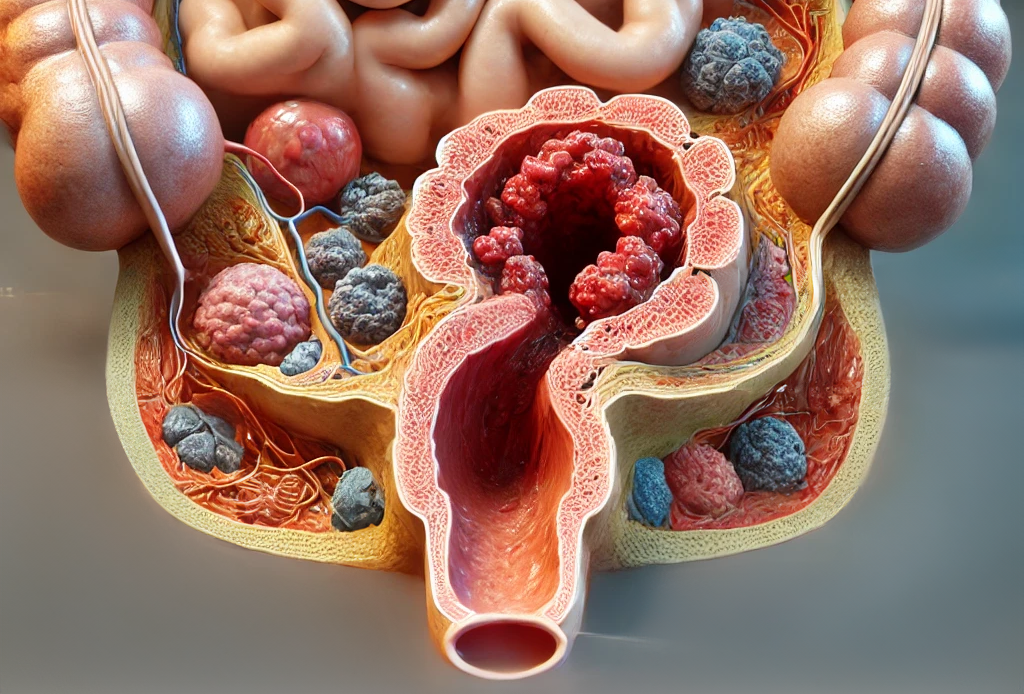
Anal Cancer: Symptoms, Causes, and Treatment
Anal cancer is a rare form of cancer that affects the end of the large bowel (rectum). The symptoms can be similar to less serious conditions, making it important to be aware of potential signs and seek medical advice when necessary.
Symptoms of Anal Cancer
Symptoms may resemble those of other conditions, such as hemorrhoids or anal fissures. Common symptoms include:
- Rectal Bleeding: Bleeding from the bottom
- Anal Itching and Pain: Persistent discomfort around the anus
- Small Lumps: Bumps around the anus
- Mucus Discharge: Unusual discharge from the anus
- Bowel Incontinence: Loss of bowel control
Note: Some individuals may have no symptoms. It’s best to consult a GP if you experience any of these symptoms to rule out serious conditions.
Diagnosing Anal Cancer
Diagnosis often begins with a GP consultation, during which your doctor will ask about symptoms and perform a rectal examination. Further tests may be required if cancer is suspected, including:
- Sigmoidoscopy: A flexible tube with a camera is inserted into the rectum to detect abnormalities.
- Proctoscopy: An examination using a hollow tube-like instrument with a light.
- Biopsy: A tissue sample may be collected for laboratory analysis.
If cancer is suspected, additional scans may be performed to assess its spread and stage the cancer.
Treatment Options for Anal Cancer
Treatment involves a multidisciplinary team of specialists. The primary options include:
1. Chemoradiation
This is a combination of chemotherapy and radiotherapy, and it’s the most common treatment for anal cancer.
- Chemotherapy: Usually given in cycles, with breaks in between. It may involve a small tube (PICC) inserted in the arm for drug delivery, or it may be administered through tablets.
- Radiotherapy: Delivered in daily sessions over several weeks.
Side Effects of chemoradiation can include tiredness, skin irritation, hair loss, nausea, and longer-term issues such as bowel control problems, erectile dysfunction, or vaginal pain. Discuss potential side effects with your care team before beginning treatment.
2. Surgery
Surgery is less common and typically reserved for cases where chemoradiation is ineffective or the tumor is small and well-defined.
- Local Excision: Removal of a small tumor, often requiring a short hospital stay.
- Abdominoperineal Resection: A more complex surgery that involves removing the anus, rectum, part of the colon, and nearby tissues. A colostomy (opening in the abdomen) is created to pass stools.
Adjusting to a colostomy can be challenging, but support from specialist nurses is available.
Follow-Up Care
Regular follow-up appointments will be scheduled after treatment to monitor recovery and detect any signs of recurrence.
Causes and Risk Factors
The exact cause of anal cancer is unknown, but several risk factors have been identified:
- Human Papillomavirus (HPV): A common virus spread through sexual contact.
- Sexual Activity: Having multiple partners or engaging in anal sex may increase the risk due to a higher likelihood of HPV exposure.
- History of Certain Cancers: Including cervical, vaginal, or vulvar cancer.
- Smoking: Linked to an increased risk.
- Weakened Immune System: Conditions like HIV can elevate risk.
- Age and Gender: Risk increases with age, with half of cases diagnosed in people over 65. Anal cancer is slightly more common in women.
When to Speak to a Healthcare Professional
If you notice persistent symptoms or are concerned about anal cancer, make an appointment with your GP. Early diagnosis is crucial for effective treatment.
More Information: Learn about the stages of anal cancer, living with a colostomy, and additional treatment options on trusted health websites like Cancer Research UK.

 4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all
4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all



