Diastolic Heart Failure
Below is a comprehensive, structured report on Diastolic Heart Failure covering its definition, historical background, clinical presentation, causes, risk factors, complications, diagnosis, treatment, prevention, global statistics, recent research, and additional insights. This report is designed to be informative for both the general public and healthcare professionals.
1. Overview
What is Diastolic Heart Failure?
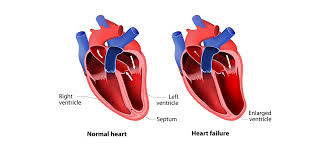
Diastolic heart failure, also known as heart failure with preserved ejection fraction (HFpEF), is a condition in which the heart’s ventricles become stiff and unable to relax properly during diastole. This impaired relaxation prevents adequate filling of the heart, leading to increased pressures in the heart and lungs, despite a normal or near-normal ejection fraction.
Detailed Definition
In diastolic heart failure, the heart muscle does not relax sufficiently during the diastolic phase, which means that the ventricles do not fill with blood as efficiently as they should. As a result, even though the heart’s pumping (systolic) function is preserved, the reduced filling can lead to symptoms of heart failure. This condition is primarily due to the increased stiffness of the myocardium, often secondary to conditions such as hypertension, aging, or metabolic disorders.
Affected Body Parts/Organs
- Left Ventricle: The primary chamber affected by diastolic dysfunction.
- Left Atrium: Experiences increased pressure due to impaired filling of the left ventricle.
- Lungs: Elevated pressures in the left atrium can lead to pulmonary congestion and edema.
- Systemic Circulation: Chronic pressure overload may eventually affect other organs.
Prevalence and Significance
Diastolic heart failure accounts for approximately 40–50% of all heart failure cases. It is especially prevalent among older adults and women. Despite its high prevalence, diastolic heart failure is challenging to treat, and its prognosis remains guarded, making it a major public health concern.
2. History & Discoveries
When and How Was Diastolic Heart Failure First Identified?
- Early Observations: Clinicians have long observed symptoms of heart failure even in patients with normal ejection fractions. However, the distinct concept of diastolic dysfunction began to emerge in the latter half of the 20th century.
- Modern Recognition: With the advent of echocardiography in the 1970s and 1980s, it became possible to assess diastolic function more accurately, leading to the recognition that heart failure can occur despite preserved systolic function.
Who Discovered It?
- Pioneering Contributions: Although no single individual is credited with “discovering” diastolic heart failure, the contributions of cardiologists and researchers in refining echocardiographic techniques and developing the concept of heart failure with preserved ejection fraction (HFpEF) have been crucial.
Major Discoveries and Breakthroughs
- Echocardiography: Revolutionized the ability to differentiate between systolic and diastolic dysfunction.
- Pathophysiological Insights: Research identified that factors such as myocardial fibrosis, hypertrophy, and inflammation contribute to increased ventricular stiffness.
- Treatment Paradigms: The realization that controlling blood pressure, reducing myocardial load, and managing comorbidities could improve symptoms has guided current management strategies.
Evolution of Medical Understanding
Medical understanding has evolved from viewing heart failure solely as a pump failure to recognizing the importance of ventricular relaxation and filling. This paradigm shift has spurred research into targeted therapies for HFpEF.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Exertional dyspnea (shortness of breath during physical activity)
- Fatigue and reduced exercise tolerance
- Occasional chest discomfort or palpitations
- Advanced-Stage Symptoms:
- Persistent shortness of breath, even at rest
- Orthopnea (difficulty breathing when lying flat)
- Paroxysmal nocturnal dyspnea (sudden nighttime episodes of breathlessness)
- Pulmonary edema (fluid accumulation in the lungs)
- Swelling in the lower extremities (peripheral edema) as a result of increased systemic venous pressure
Common vs. Rare Symptoms
- Common Symptoms:
Shortness of breath, fatigue, and exercise intolerance are the hallmark features. - Rare Symptoms:
Some patients may develop atypical symptoms such as subtle cognitive impairment due to chronic low cardiac output or arrhythmias, though these are less frequently observed in early stages.
How Symptoms Progress Over Time
Symptoms of diastolic heart failure typically develop gradually. Early in the disease, patients may only notice decreased exercise capacity or mild dyspnea. As the condition progresses, fluid retention and elevated pressures in the heart lead to more pronounced symptoms, including rest dyspnea and edema. Early intervention can help slow progression and improve quality of life.
4. Causes
Biological and Environmental Causes
- Biological Causes:
The primary mechanism is the increased stiffness of the ventricular myocardium due to:- Hypertensive heart disease
- Myocardial fibrosis
- Infiltrative diseases (e.g., amyloidosis)
- Environmental Causes:
Long-term exposure to factors that promote hypertension (e.g., high-sodium diet, sedentary lifestyle) indirectly contribute to diastolic dysfunction.
Genetic and Hereditary Factors
- Inherited Predispositions:
Family history of cardiovascular disease can predispose individuals to conditions leading to diastolic dysfunction. Genetic factors affecting myocardial structure and response to injury may also play a role.
Known Triggers or Exposure Risks
- Chronic Hypertension:
The most significant risk factor, as it causes left ventricular hypertrophy and subsequent stiffness. - Diabetes and Obesity:
Metabolic disorders contribute to myocardial remodeling. - Aging:
Natural age-related changes in the heart increase myocardial stiffness and impair relaxation.
5. Risk Factors
Who Is Most at Risk?
- Age:
Incidence increases with age, particularly in individuals over 65. - Gender:
Women are at a relatively higher risk for diastolic dysfunction and HFpEF compared to men. - Lifestyle:
Sedentary lifestyle, poor diet, and obesity are significant contributors. - Pre-existing Conditions:
Chronic hypertension, diabetes, and coronary artery disease elevate risk.
Environmental, Occupational, and Genetic Factors
- Environmental:
Urban environments with high stress and lifestyle factors that contribute to cardiovascular risk. - Occupational:
Jobs associated with high stress and sedentary behavior may indirectly increase risk. - Genetic:
Family history of heart disease and specific genetic markers related to myocardial structure may predispose to diastolic dysfunction.
Impact of Pre-existing Conditions
- Comorbidities:
Conditions like chronic kidney disease, metabolic syndrome, and atrial fibrillation can worsen diastolic function and contribute to a poorer prognosis.
6. Complications
What Complications Can Arise from Diastolic Heart Failure?
- Progression to Systolic Dysfunction:
Although diastolic and systolic dysfunction are distinct, long-standing diastolic failure can eventually lead to combined forms of heart failure. - Pulmonary Edema:
Elevated left atrial pressure can result in fluid accumulation in the lungs. - Arrhythmias:
Increased atrial pressures can predispose to atrial fibrillation. - Multi-organ Dysfunction:
Reduced cardiac output can impair perfusion to other organs, leading to renal and hepatic dysfunction.
Long-term Impact on Organs and Overall Health
Chronic diastolic heart failure can lead to persistent symptoms, reduced quality of life, and increased risk for hospitalizations. The condition may also predispose patients to recurrent heart failure episodes and increased overall cardiovascular mortality.
Potential Disability or Fatality Rates
While early-stage diastolic dysfunction is generally manageable, progression to advanced heart failure significantly increases the risk of disability and mortality. Prognosis depends on the severity of underlying conditions and the effectiveness of management strategies.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
Detailed medical history, physical examination, and assessment of symptoms. - Echocardiography:
The primary diagnostic tool used to assess ventricular structure, function, and diastolic filling patterns. - Electrocardiogram (ECG):
Helps identify left ventricular hypertrophy and arrhythmias.
Medical Tests
- Doppler Echocardiography:
Evaluates diastolic function by measuring parameters such as E/A ratio, deceleration time, and tissue Doppler imaging. - Blood Tests:
BNP (B-type natriuretic peptide) levels may be elevated in heart failure. - Advanced Imaging:
Cardiac MRI can be used for detailed assessment of myocardial tissue characteristics.
Early Detection Methods and Their Effectiveness
Early detection of diastolic dysfunction using echocardiography and biomarkers is highly effective. Routine cardiovascular screening in at-risk populations allows for early intervention, which is essential to prevent progression and improve outcomes.
8. Treatment Options
Standard Treatment Protocols
- Lifestyle Modifications:
Dietary changes (e.g., low-sodium diet), regular physical exercise, weight management, and stress reduction. - Pharmacotherapy:
- Antihypertensives: ACE inhibitors, ARBs, and beta-blockers to control blood pressure and reduce myocardial stress.
- Diuretics: To manage fluid overload and reduce pulmonary congestion.
- Aldosterone Antagonists: May help in reducing myocardial fibrosis and improving outcomes.
- Management of Comorbidities:
Tight control of diabetes, obesity, and coronary artery disease.
Medications, Surgeries, and Therapies
- Medications:
A combination of blood pressure control agents, diuretics, and possibly statins to address underlying atherosclerosis. - Non-pharmacologic Therapies:
Cardiac rehabilitation programs and lifestyle interventions. - Emerging Treatments:
Novel agents targeting myocardial fibrosis, and innovative therapies based on precision medicine are under investigation.
Emerging Treatments and Clinical Trials
- Targeted Molecular Therapies:
Investigational drugs aimed at modulating myocardial stiffness and inflammation. - Clinical Trials:
Ongoing studies are evaluating new pharmacologic combinations and the potential role of regenerative therapies to improve diastolic function.
9. Prevention & Precautionary Measures
How Can Diastolic Heart Failure Be Prevented?
- Risk Factor Modification:
Control of hypertension, diabetes, and obesity is key. A healthy diet, regular exercise, and weight management are critical. - Lifestyle Changes:
Avoidance of smoking and excessive alcohol consumption, stress reduction, and adherence to prescribed medications. - Regular Screening:
Routine cardiovascular assessments, especially in at-risk populations, can help detect early diastolic dysfunction.
Lifestyle Changes and Environmental Precautions
- Diet and Exercise:
A balanced diet low in salt and saturated fats along with regular physical activity helps maintain cardiovascular health. - Public Health Initiatives:
Community-based programs to improve cardiovascular awareness and promote healthy lifestyles.
Vaccines or Preventive Screenings
- Preventive Screenings:
While there is no vaccine for diastolic heart failure, regular blood pressure monitoring, and echocardiographic assessments are essential preventive strategies.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Prevalence:
Diastolic heart failure (HFpEF) accounts for nearly half of all heart failure cases. Its prevalence increases with age and is higher among women. - Regional Variability:
Developed countries report higher detection rates due to advanced screening and diagnostic tools, whereas incidence in developing regions is rising with aging populations and increasing rates of hypertension and diabetes.
Mortality and Survival Rates
- Mortality:
While overall mortality for HFpEF is significant due to the chronic nature of heart failure, early detection and management can improve survival. - Survival:
Five-year survival rates vary depending on comorbidities, but HFpEF is associated with substantial morbidity and reduced quality of life.
Country-wise Comparison and Trends
- Developed Countries:
Higher diagnosis rates with better treatment outcomes due to access to advanced healthcare. - Developing Countries:
Increasing incidence due to demographic changes and rising prevalence of risk factors, with outcomes often limited by healthcare access.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Molecular Insights:
Research is focusing on the molecular mechanisms underlying myocardial fibrosis and stiffening. - Precision Medicine:
Genomic and biomarker studies are paving the way for personalized therapies tailored to individual risk profiles. - Innovative Therapies:
Investigational drugs targeting inflammatory pathways and myocardial remodeling show promise.
Ongoing Studies and Future Medical Possibilities
- Clinical Trials:
Numerous trials are underway to assess novel drug therapies and the impact of lifestyle interventions on diastolic function. - Regenerative Medicine:
Early-stage research into stem cell therapies and tissue engineering aims to promote myocardial repair. - Integrated Care Models:
Combining pharmacotherapy, lifestyle changes, and digital health monitoring may further enhance patient outcomes.
Potential Cures or Innovative Therapies Under Development
While a definitive cure for diastolic heart failure remains elusive, emerging therapies focusing on reducing myocardial stiffness, controlling comorbidities, and improving overall cardiac function offer hope for better long-term management and quality of life improvements.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Diastolic Heart Failure
- Prevalence:
Diastolic heart failure accounts for almost 50% of heart failure cases, yet it is often under-recognized compared to systolic dysfunction. - Gender Differences:
Women are disproportionately affected by HFpEF compared to men. - Complex Diagnosis:
Despite a preserved ejection fraction, patients may have severe symptoms due to impaired ventricular relaxation and increased filling pressures.
Myths and Misconceptions vs. Medical Facts
- Myth: “A normal ejection fraction means the heart is functioning normally.”
Fact: In diastolic heart failure, the ejection fraction is preserved, but the heart’s filling capacity is impaired, leading to symptoms of heart failure. - Myth: “Diastolic heart failure is less serious than systolic heart failure.”
Fact: Although the ejection fraction is normal, the prognosis of HFpEF is similar to that of systolic heart failure due to the chronic burden of symptoms and comorbidities. - Myth: “Lifestyle modifications have little impact on diastolic heart failure.”
Fact: Lifestyle changes, such as weight loss, exercise, and dietary adjustments, can significantly improve symptoms and overall heart function.
Impact on Specific Populations or Professions
- High-Risk Groups:
Older adults, particularly women, and those with a history of hypertension, diabetes, or obesity are at increased risk. - Occupational Impact:
Chronic heart failure can affect work productivity and quality of life, making effective management essential for maintaining daily function.
References
- – Provides comprehensive data on the epidemiology, diagnosis, and management of diastolic heart failure.
- – Offers global statistics and public health guidelines for heart failure.
- – Summarizes recent clinical studies and research findings on diastolic dysfunction and HFpEF.
This report integrates current clinical knowledge and research findings to provide a detailed overview of diastolic heart failure. Understanding its pathophysiology, early detection, and effective management strategies is critical to improving outcomes and quality of life for affected individuals, while guiding future research and public health interventions.

 4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all
4.1 Attribution Theory and Person Perception: Why We Judge People the Way We Do (Even When We’re Totally Wrong) Let’s be honest. We’ve all



