Overview
Definition: Mesothelioma is a rare but aggressive cancer arising from the mesothelium – the thin layer of tissue lining internal organs. It most often develops in the pleura (lining of the lungs) but can also occur in the peritoneum (abdominal lining), pericardium (heart sac), or tunica vaginalis (testicular lining). This malignancy is strongly linked to asbestos exposure, which causes DNA damage and chronic inflammation in mesothelial cells.
Affected Organs: Depending on the site, mesothelioma is classified as:
- Pleural mesothelioma: affecting the lung linings (about 65–70% of cases).
- Peritoneal mesothelioma: affecting the abdominal lining (≈30% of cases).
- Pericardial mesothelioma: around the heart (1–2%).
- Tunica vaginalis mesothelioma: around the testes (extremely rare, <1%).
Prevalence and Significance: Mesothelioma is uncommon but highly significant due to its severity. Globally, about 30,000 new cases are diagnosed each year. In the United States, roughly 2,500–3,000 cases occur annually (≈1 case per 100,000 people). It disproportionately affects older adults (average age ~72 for pleural mesothelioma), and men are diagnosed more often than women (likely due to occupational asbestos exposure). Mesothelioma carries a poor prognosis – the median survival is only around 12 months. Five-year survival rates are low (approximately 10% overall in pleural mesothelioma), underscoring the disease’s aggressive nature and the importance of awareness and research.
2. History & Discoveries
First Identification: The earliest known reference to mesothelioma dates back to 1767, when French physician Joseph Lieutaud described tumors on the pleural lining during autopsies. In 1819, René Laennec (inventor of the stethoscope) also suggested that cancer could originate in the pleura. However, for much of the 19th century, pleural tumors were thought to be extensions of other cancers rather than primary tumors.
Nomenclature and Early Research: The term “mesothelioma” was officially coined in 1909 by J.G. Adami to describe this rare cancer of the mesothelial tissue. Early 20th-century doctors began recognizing mesotheliomas as distinct tumors. In 1908, Miller and Wynn reported a case of peritoneal mesothelioma in a 32-year-old patient with abdominal tumors. Throughout the 1930s and 1940s, scattered reports (e.g. by pathologist Steven Gloyne in 1935 and H.W. Wedler in 1943) hinted at a connection between asbestos exposure and pleural tumors, but solid evidence was still lacking.
Link to Asbestos: A major breakthrough came in 1960. J. Christopher Wagner and colleagues published a seminal study of 33 mesothelioma cases in South Africa, conclusively linking asbestos exposure (particularly crocidolite, a blue asbestos mined there) to mesothelioma. This study firmly established asbestos as the primary cause of mesothelioma and changed public health policies. Subsequent research in the 1960s, such as studies by Dr. Irving Selikoff in the U.S. and by Muriel Newhouse in the U.K., reinforced the asbestos–mesothelioma connection, showing high mesothelioma rates in asbestos workers and even their family members (from fibers brought home on clothing). By the late 20th century, the link was indisputable, leading to regulations limiting asbestos use in many countries.
Evolution of Understanding: Over time, medical understanding of mesothelioma has greatly evolved. Initially, treatment options were almost nonexistent and diagnosis was often made only at autopsy. The late 20th century saw development of diagnostic imaging and pathology techniques that allowed mesothelioma to be diagnosed while patients were alive, enabling some treatment. In 2004, the first effective chemotherapy (pemetrexed with cisplatin) was approved, improving survival modestly. In the 2010s, researchers discovered genetic factors like the BAP1 gene mutation that predispose individuals to mesothelioma, explaining why some people develop the cancer even with lower asbestos exposure. Most recently, in 2020, a combination immunotherapy (nivolumab and ipilimumab) was approved for mesothelioma, marking the first new systemic treatment in over a decade. Today, ongoing clinical trials are exploring targeted therapies, gene therapy, and innovative treatments, reflecting a much deeper scientific understanding than in the past.
3. Symptoms
Mesothelioma symptoms develop insidiously and often resemble more common illnesses, which contributes to delayed diagnosis. Early-stage mesothelioma may cause very mild or no symptoms at all. Many patients feel healthy for years during the cancer’s long latency period (20–50 years after exposure). When symptoms do emerge, they tend to be vague: slight shortness of breath, fatigue, or a mild persistent cough can be early signs for pleural cases, while abdominal bloating or discomfort may be early signs for peritoneal cases.
Advanced-stage symptoms become more pronounced as the tumor grows and spreads. These symptoms differ somewhat by mesothelioma type:
Pleural Mesothelioma (lung lining): Common symptoms include chest pain or tightness, chronic dry cough, and increasing shortness of breath. Patients might notice difficulty taking deep breaths or feel as if their lower back or side chest is painful. As disease advances, fluid buildup in the chest (pleural effusion) can cause a feeling of heaviness and severe breathlessness. Other symptoms can include hoarseness, trouble swallowing, or swelling of the face and arms due to pressure on veins (these tend to be less common).
Peritoneal Mesothelioma (abdominal lining): Symptoms often begin with abdominal pain or a feeling of fullness. As the cancer progresses, nearly all patients develop ascites, an abnormal fluid buildup in the abdomen, leading to visible swelling. This can cause abdominal distension, nausea, loss of appetite, and bowel habit changes (constipation or diarrhea). In late stages, tumors may cause bowel obstructions – patients experience severe abdominal cramps, inability to move bowels, and vomiting.
Pericardial Mesothelioma (heart lining): This rare form can cause chest pain, heart palpitations or irregular heartbeat, and shortness of breath as the tumor and fluid around the heart (pericardial effusion) impair cardiac function. These symptoms often resemble other heart conditions.
Tunica Vaginalis Mesothelioma (testicular lining): Extremely rare; it may present as a painless testicular mass or swelling in the scrotum. Often it’s discovered incidentally during surgery for what is thought to be a hernia.
General/Systemic Symptoms: Regardless of location, mesothelioma can cause systemic signs such as unexplained weight loss (even without dieting), fatigue and muscle weakness, low-grade fevers, and night sweats. Some patients develop finger clubbing (changes in fingernail shape) in pleural mesothelioma, a relatively uncommon sign. Blood clots can also occur more frequently in cancer patients.
Symptom Progression: Mesothelioma symptoms tend to worsen over time. For example, a patient might start with a mild cough and slight breathlessness that gradually progress to severe respiratory distress as pleural fluid accumulates. Early on, symptoms are so nonspecific that they are often attributed to minor ailments (for instance, chest pain and fatigue might be blamed on aging or smoking). As the cancer advances to late stages, symptoms like intense pain (from tumor pressure on nerves or chest wall), pronounced swelling, or debilitating shortness of breath typically force patients to seek medical attention. Unfortunately, by this time the disease is usually advanced. It’s important to note that the early subtle symptoms often mimic benign conditions, so any persistent symptom in someone with asbestos exposure history should be evaluated promptly. Early detection, though difficult, can improve outcomes.
4. Causes
Mesothelioma is primarily caused by environmental and occupational exposure to certain carcinogens, with asbestos being by far the leading cause. Key causes and contributing factors include:
Asbestos Exposure: Asbestos is a group of fibrous minerals once widely used in construction, insulation, shipbuilding, and various industries for its fire-resistant properties. Inhalation or ingestion of asbestos fibers is the predominant cause of mesothelioma. In the U.K., for example, asbestos exposure is linked to >95% of mesothelioma cases in men and ~85% in women. When asbestos fibers are inhaled, they can lodge in the pleura (lung lining) causing chronic inflammation and cellular damage. Some fibers can be coughed up and swallowed, leading to peritoneal mesothelioma in the abdomen. Over years, the persistent irritation and reactive oxygen species from these fibers cause DNA mutations in mesothelial cells, triggering cancer. All types of asbestos (blue crocidolite, brown amosite, and even white chrysotile) are now recognized as hazardous, though blue and brown are most strongly linked to mesothelioma. Notably, mesothelioma typically appears decades after asbestos exposure – the latency period is often 20–50 years.
Industrial Pollutants and Other Fibrous Minerals: Besides asbestos, other fibrous silicate minerals can cause mesothelioma. In certain regions of Turkey, exposure to erionite (a natural zeolite fiber found in rock/soil) led to epidemic mesothelioma in villages. Another mineral called fluoro-edenite (found in Italy) has also been implicated in mesothelioma cases. These substances act similarly to asbestos fibers when inhaled. Occupational exposure to refractory ceramic fibers has likewise been suggested as a risk, though asbestos remains the main culprit.
Radiation Exposure: In rare cases, high-dose ionizing radiation to the chest has been linked to mesothelioma. For instance, some patients who received chest radiation therapy for lymphoma (such as mantle radiation for Hodgkin’s disease) years later developed mesothelioma. This is an uncommon cause but is documented in medical literature. The radiation likely damages mesothelial DNA directly.
Simian Virus 40 (SV40): Some studies in the past speculated that SV40 (a virus found as a contaminant in 1950s–60s polio vaccines) might contribute to mesothelioma. SV40 DNA was detected in some mesothelioma tumors, raising questions about a cofactor role. However, this link remains controversial and unproven; asbestos is overwhelmingly the primary cause in exposed individuals. Current consensus is that if SV40 plays any role, it is minor compared to asbestos.
Genetic Factors: While asbestos is the trigger in most cases, genetics can influence susceptibility. A notable example is the BAP1 gene (BRCA1-Associated Protein 1). Inherited mutations in BAP1 cause a rare BAP1 tumor predisposition syndrome, which greatly increases the risk of mesothelioma (as well as melanoma and other cancers). Individuals with a BAP1 mutation who are exposed to asbestos have a higher likelihood of developing mesothelioma, sometimes with shorter latency. Even sporadic (non-inherited) BAP1 mutations are found in many mesotheliomas, indicating this gene’s importance. Other genetic differences, such as deletions in chromosomes 1p, 3p, 6q, or 9p, have been observed in mesothelioma cells, though their role as causes is still being studied. Essentially, a genetic predisposition can lower the “threshold” of asbestos required to cause disease.
Other Possible Factors: Chronic irritation or scarring in the mesothelium may contribute in rare circumstances. For example, chronic pleural inflammation from old tuberculosis or prior pleural injury has been considered as a very uncommon precursor. Some cases of peritoneal mesothelioma had no asbestos exposure but a history of chronic peritonitis. These situations are not well understood. It’s important to note that smoking is not a direct cause of mesothelioma. Unlike lung cancer, smoking alone has no proven effect on mesothelioma risk – though in people who also have asbestos exposure, smoking greatly increases the risk of lung cancer (a different malignancy). This is a common misconception; the only established lifestyle factor causing mesothelioma is asbestos exposure, often occupational.
In summary, asbestos exposure stands out as the dominant cause of mesothelioma, with a handful of other factors (certain minerals, high-dose radiation, or genetic mutations) playing a role in a minority of cases. Most patients have a history of working with or around asbestos decades before their diagnosis.
5. Risk Factors
While anyone can develop mesothelioma, certain risk factors greatly increase the likelihood:
Occupational Exposure: The highest risk is among people who worked with asbestos-containing materials. Occupations historically associated with heavy asbestos exposure include:
- Shipyard and Navy workers: Shipbuilders, insulators, and boiler workers were heavily exposed (asbestos was used in ship insulation and engines).
- Construction and Demolition workers: Carpenters, plumbers, electricians, roofers, and demolition crews often encountered asbestos in insulation, ceiling tiles, cement, and drywall of older buildings.
- Asbestos Mining and Manufacturing: Asbestos miners and mill workers, as well as factory workers making products like asbestos cement, textiles, brakes, and gaskets, had chronic exposure.
- Industrial and Power Plant workers: Mechanics (especially brake and clutch repair where asbestos was used), refinery and chemical plant workers, and power plant workers were at risk due to asbestos insulation on pipes and machinery.
- Military personnel: Certain military roles (Navy engine rooms, military construction) had asbestos exposure. Some veterans have higher mesothelioma rates due to this.
- Firefighters and First Responders: They may be exposed when old buildings burn or collapse, releasing asbestos dust.
Among heavily exposed workers, an estimated 8–13% may eventually develop mesothelioma. The risk correlates with dose and duration of exposure – long-term, high-level exposure (e.g., decades in an asbestos factory) carries the greatest risk. However, even short-term or secondary exposure can be dangerous.
Secondary Exposure: Family members of asbestos workers also face risk. Workers can unknowingly bring asbestos fibers home on their clothes, hair, or tools, exposing their families. Wives washing work clothes or children hugging a parent in dusty overalls have contracted mesothelioma from this “second-hand” asbestos exposure. Living near asbestos mines or factories is another form of environmental exposure; communities around such facilities have shown higher mesothelioma rates due to airborne fibers.
Age: Mesothelioma typically occurs in older adults. The disease has a long latency, often appearing 20–50 years after exposure. Thus, most patients are senior citizens by the time of diagnosis. In the U.S., the average age at diagnosis for pleural mesothelioma is about 72 years. Cases under 45 are very uncommon. Children and young adults rarely get mesothelioma; when they do, it’s often peritoneal and without any known asbestos contact, possibly linked to other genetic factors.
Gender: Men are significantly more likely to develop mesothelioma than women. In the U.S., about 80% of mesothelioma patients are male. This gap is because men historically held most jobs with high asbestos exposure (shipyards, construction, etc.). Women’s cases often come from secondary exposure (e.g., a spouse’s workplace exposure) or environmental sources. Notably, women who do develop mesothelioma may have slightly better survival on average, though the reasons aren’t clear. Gender itself (biologically) isn’t a risk, but exposure patterns differ by gender.
Geographic Region: Risk varies by country depending on past asbestos use and regulations. For instance, the U.K., Belgium, and Australia (which used asbestos heavily mid-20th century) have the highest mesothelioma incidence – up to ~30 cases per million people per year. In contrast, countries that used little asbestos (or banned it earlier) have lower rates (e.g., <1 per million in some African nations). Living in regions with naturally occurring asbestos or erionite (such as parts of Turkey or North Dakota, USA) also raises risk if fibers become airborne.
Genetic Predisposition: As mentioned, a family history of mesothelioma or related cancers might indicate a genetic risk like the BAP1 mutation. If a person inherits a BAP1 mutation (or certain other rare mutations), their risk of mesothelioma increases, especially if they are ever exposed to asbestos. However, these hereditary cases are a very small fraction of all mesotheliomas. For the general population, routine genetic testing isn’t done – but in families with multiple mesotheliomas or BAP1 syndrome, genetic counseling is advisable.
Other Lung Conditions: Having asbestosis (chronic asbestos-induced lung scarring) or pleural plaques (benign asbestos scarring on pleura) indicates significant asbestos exposure and thus a higher risk for mesothelioma in the future. However, conditions like COPD or tuberculosis, by themselves, are not known to cause mesothelioma – they might only confound diagnosis or co-exist.
Lifestyle Factors: Interestingly, smoking does not increase mesothelioma risk. This is a key difference from lung cancer. But smoking combined with asbestos markedly raises lung cancer risk, which can complicate a patient’s overall health. Alcohol use, diet, or other lifestyle factors have no confirmed direct link to mesothelioma. Being in good general health might help one tolerate treatment better, but it doesn’t prevent mesothelioma if asbestos exposure has occurred. There is some emerging evidence that general wellness (like exercise) could potentially improve outcomes or delay disease in those exposed, but it’s not a proven preventive measure.
In summary, the profile of highest risk is an individual (usually a man over 60) who worked in an asbestos-rich industry for many years. That said, because of secondary exposures and environmental sources, mesothelioma can also appear in people without direct occupational contact, including some women and younger individuals. Recognizing these risk factors is crucial for clinicians to maintain a high index of suspicion when such individuals present with compatible symptoms.
6. Complications
Mesothelioma, especially in advanced stages, can lead to serious complications affecting both the organ systems involved and the body as a whole. These complications often arise from the tumor’s tendency to spread along surfaces and exert pressure on organs:
Respiratory Complications (Pleural Mesothelioma): As pleural mesothelioma grows, it encases and constricts the lung and can invade the chest wall. A very common complication is pleural effusion, a buildup of fluid around the lungs. The accumulating fluid compresses the lung, causing severe shortness of breath and a feeling of chest heaviness. Recurrent effusions may require frequent drainage or pleurodesis (sealing the pleural space). The tumor itself causes pleuritic chest pain – often a dull ache that can become sharp if the tumor irritates the chest wall or diaphragm. If the cancer invades the phrenic nerve or intercostal nerves, it can cause intractable pain or even diaphragmatic paralysis. Advanced pleural mesothelioma may also compress the esophagus, leading to dysphagia (trouble swallowing), or compress large veins (superior vena cava syndrome) causing swelling in the face and arms. Eventually, extensive tumor burden in the chest can lead to respiratory failure.
Abdominal Complications (Peritoneal Mesothelioma): The hallmark complication is ascites, which is fluid accumulation in the abdominal cavity. This fluid causes abdominal distension, discomfort, and pressure on internal organs, leading to loss of appetite and reduced lung capacity (making breathing harder). As tumors spread on peritoneal surfaces, they can obstruct the intestines; bowel obstruction is a serious complication in late-stage peritoneal mesothelioma. Patients with a bowel obstruction experience abdominal pain, bloating, vomiting, and inability to pass stool – this can be life-threatening and may require surgical intervention or stenting to relieve the blockage. Tumor nodules can also affect the liver or spleen, or rarely spread through the diaphragm into the pleural cavity (causing combined chest and abdominal issues).
Cardiac Complications (Pericardial Mesothelioma): Though rare, pericardial mesothelioma can cause a pericardial effusion (fluid around the heart) which leads to cardiac tamponade – the fluid compresses the heart, preventing it from filling properly. This results in low blood pressure, shortness of breath, and can be fatal if not relieved. The tumor can trigger arrhythmias (irregular heartbeats) and presents as chest pain mimicking a heart attack.
Systemic Effects: Mesothelioma often leads to general health decline. Many patients experience cachexia – a syndrome of weight loss, muscle wasting, and weakness. This results from the cancer’s effect on metabolism and the loss of appetite that many endure. Fatigue becomes nearly universal in advanced disease due to a combination of cancer burden, poor nutrition, and reduced lung function. Anemia (low red blood cells) is common and can worsen fatigue. Mesothelioma can also provoke a hypercoagulable state, meaning patients are prone to blood clots (deep vein thrombosis or pulmonary embolism), which can cause additional complications like stroke or clot in the lungs.
Local Invasion: Locally, mesothelioma tends to spread along surfaces rather than via the bloodstream. In the chest, it can invade the chest wall, ribs, or brachial plexus nerves, causing severe nerve pain and even arm disability if nerves are involved. In the abdomen, it can invade the abdominal wall or retroperitoneum. If pleural mesothelioma invades upward, it may affect the laryngeal nerve causing hoarseness or the vena cava causing upper body swelling.
Treatment-Related Complications: Sometimes the interventions for mesothelioma have risks. For example, surgery like extrapleural pneumonectomy carries risks of significant complications (infection, respiratory failure). Chemotherapy can weaken the immune system and cause kidney or nerve damage. While these are not complications of the disease per se, they impact the patient’s health during the mesothelioma journey.
Prognosis and Fatality: Unfortunately, mesothelioma’s complications often lead to fatal outcomes. The disease’s progression typically causes organ failure – commonly respiratory failure in pleural mesothelioma or intestinal failure in peritoneal mesothelioma (due to malnutrition or obstruction). Without treatment, mesothelioma is rapidly fatal (median survival ~1 year). Even with treatment, the overall 5-year survival remains around 10% or less. Thus, mesothelioma is often described as an aggressive cancer with high complication and mortality rates.
Despite these dire complications, aggressive symptom management and modern therapies can improve quality of life. For instance, regular drainage of effusions, pain control (often requiring strong analgesics), and nutritional support can help manage complications. Some patients live longer with a combination of treatments and supportive care, but long-term survivors are rare. The complications underscore why mesothelioma is such a feared disease – it progressively impairs vital organ functions and is usually incurable once it has spread.
7. Diagnosis & Testing
Diagnosing mesothelioma can be challenging because its symptoms mimic more common conditions and it is a rare disease. There is no routine screening test for mesothelioma in people without symptoms, so diagnosis usually begins when a patient presents with concerning symptoms and has a history of asbestos exposure.
Initial Evaluation: A detailed medical history and physical exam are critical first steps. Doctors will ask about occupational history (exposure to asbestos or similar materials) and any related symptoms. During the exam, signs like fluid in the chest or abdomen may be detected by tapping (percussion) or listening with a stethoscope (reduced breath sounds can indicate a pleural effusion). If mesothelioma is suspected based on history (e.g., an ex-shipyard worker with chest pain and fluid on the lung), further testing is ordered.
Imaging Studies: These are crucial to detect abnormalities and guide further tests:
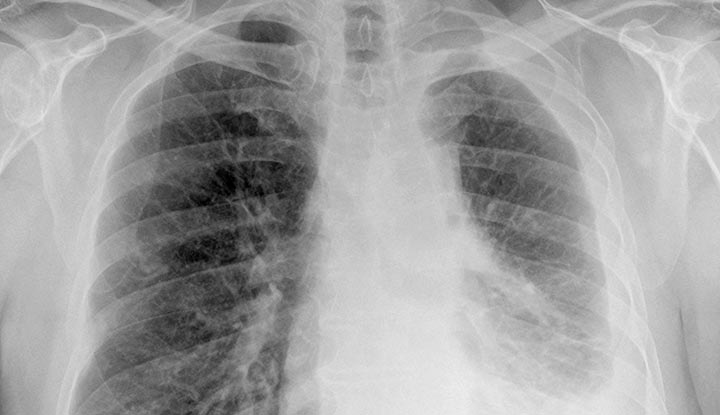
- Chest X-ray: Often the first imaging test if pleural mesothelioma is suspected. An X-ray might show pleural effusion or pleural thickening/calcifications (sometimes seen as a result of asbestos exposure). While an X-ray cannot confirm mesothelioma, it can reveal clues such as irregular pleural masses or fluid that warrant more investigation.
- Computed Tomography (CT) Scan: CT scans provide detailed cross-sectional images of the chest or abdomen and are a key tool. A CT can reveal the presence, size, and extent of tumors in the pleura or peritoneum. For pleural mesothelioma, CT helps show if the tumor is confined or has invaded the chest wall, diaphragm, or lymph nodes, which is essential for staging. CT of the abdomen is similarly used for peritoneal disease. CT scans are also used to guide biopsy needles to the right location.
- Magnetic Resonance Imaging (MRI): MRI is sometimes used to better visualize the tumor’s relationship with soft tissues. In mesothelioma, MRI can be helpful if there’s suspicion of tumor invading the diaphragm, blood vessels, or spine, due to its superior soft tissue contrast. It’s not always routine but can be valuable in surgical planning.
- Positron Emission Tomography (PET) Scan: Often combined with CT (PET-CT), this nuclear medicine test uses a radioactive sugar to highlight metabolically active cells (like cancer cells). Mesothelioma typically shows up as PET “hot spots.” PET-CT is very useful in determining the cancer’s stage – for example, to see if it has spread to lymph nodes or other organs not obvious on CT. It can sometimes detect metastases that CT missed. PET-CT is also used to evaluate the whole body to ensure the cancer is localized (important when considering surgery).
- Ultrasound/Echocardiogram: An ultrasound of the chest can identify pleural effusions and guide thoracentesis (fluid draw). An echocardiogram (ultrasound of the heart) is used if pericardial mesothelioma or pericardial effusion is suspected, to see fluid around the heart and check cardiac function. For abdominal mesothelioma, ultrasound can help detect ascites and guide fluid removal (paracentesis).
Imaging results might show, for example, a diffuse thickening of the pleura encasing the lung – a classic sign of pleural mesothelioma. But imaging alone cannot definitively diagnose mesothelioma; it can only suggest it.
Fluid Analysis (Cytology): If there is fluid buildup (effusion or ascites), doctors often remove a sample with a needle:
- Thoracentesis: Drawing fluid from the chest effusion.
- Paracentesis: Drawing fluid from abdominal ascites.
- Pericardiocentesis: Drawing fluid from around the heart.
The fluid is examined under a microscope for cancer cells. If malignant mesothelial cells are seen, it can point to mesothelioma. However, mesothelioma cells can be hard to distinguish from other cancer cells in fluid. Often, fluid cytology is not sufficient for a conclusive diagnosis. In many cases, fluid analysis comes back as “suspicious” or even false-negative, so a tissue biopsy is needed.
Biopsy (Tissue Sampling): A biopsy – taking a piece of the suspected tumor for pathological examination – is the gold standard for diagnosing mesothelioma. Types of biopsies include:
- Needle Biopsy: Using a long needle (sometimes under CT or ultrasound guidance) to extract a core of tissue from the tumor or lymph node. For pleural mesothelioma, a CT-guided needle biopsy through the chest wall can sample the pleural thickening. Needle biopsies are minimally invasive, but they have a risk of sampling error (the sample might be too small or miss the tumor). If a needle biopsy is non-diagnostic and suspicion remains high, more invasive biopsy is needed.
- Thoracoscopy (Pleuroscopy): This is a minimally invasive surgery where a scope (camera) is inserted through the chest wall to directly visualize the pleura and take multiple biopsies. It’s usually done under sedation or general anesthesia. Thoracoscopy allows the doctor to see tumor deposits and take larger tissue samples from different areas. It has a high diagnostic yield for pleural mesothelioma and also allows fluid drainage in the same procedure.
- Laparoscopy: Similar to thoracoscopy, but for the abdomen. A camera goes into the abdominal cavity (through a small incision) to inspect the peritoneum and obtain biopsy samples from any suspicious nodules or thickening.
- Open Surgical Biopsy: In some cases, a mini-thoracotomy (open chest) or laparotomy (open abdomen) is performed to get a biopsy if less invasive methods were inconclusive. This is more invasive but provides the largest tissue sample.
- Mediastinoscopy: If imaging shows enlarged lymph nodes in the mediastinum (center of chest), doctors might biopsy them via mediastinoscopy (inserting a scope at the base of the neck). This can check if pleural mesothelioma has spread to lymph nodes, which helps in staging; it’s not for initial diagnosis of the primary tumor but for staging purposes.
Once a tissue sample is obtained, a pathologist examines it under the microscope. Special staining techniques called immunohistochemistry are used to differentiate mesothelioma from other cancers (like lung adenocarcinoma) which can look similar under the microscope. Mesothelioma cells often test positive for markers like calretinin, WT-1, D2-40, and cytokeratin 5/6, and negative for lung carcinoma markers like CEA or TTF-1. If the panel of stains fits mesothelioma, it confirms the diagnosis.
Blood Tests: There is no blood test that can definitively diagnose mesothelioma, but researchers have identified some biomarkers that tend to be elevated in mesothelioma patients:
- Soluble Mesothelin-Related Peptides (SMRP): Mesothelin is a protein released by mesothelioma cells; SMRPs are fragments detectable in blood. Many mesothelioma patients have high SMRP levels.
- Fibulin-3: Another protein that can be elevated in mesothelioma.
While these markers are of research interest, they are not accurate enough to serve as standalone diagnostic tests. For example, SMRP can be normal in some mesotheliomas and elevated in some other conditions. Thus, blood tests are not routinely used for diagnosis outside of clinical trials or specialist centers. They might be used as an adjunct – if someone with asbestos exposure has high SMRP, it raises suspicion – but a biopsy is still required.
Pulmonary Function Tests (PFTs): If pleural mesothelioma is confirmed, doctors often perform PFTs to assess how well the lungs are working. This is especially important if surgery is being considered, to ensure the patient can tolerate removal of a lung or a portion of it. PFTs measure lung capacity and breathing strength. While not diagnostic of mesothelioma, PFT results help guide treatment decisions.
Diagnosis Challenges: Because early symptoms are nonspecific, the average time from first symptoms to diagnosis can be several months. Patients often go through evaluations for more common issues (like pneumonia or arthritis for chest pain) before mesothelioma is suspected. Physicians must connect the dots between a patient’s symptom profile and their asbestos exposure risk. Even on imaging, mesothelioma can resemble other diseases (e.g., pleural thickening might be misread as benign scarring). High suspicion is needed in at-risk individuals. One study noted an average of about 122 days from first symptoms to a correct diagnosis, illustrating delays.
There are no approved screening programs for mesothelioma in asymptomatic people, even those with asbestos exposure. However, some experts recommend that individuals with known heavy asbestos exposure be followed periodically with chest X-rays or CT scans to catch disease earlier. Research is ongoing into better blood biomarkers or imaging techniques (like advanced CT/PET algorithms) that could enable earlier detection in high-risk groups.
In summary, diagnosing mesothelioma typically involves imaging to detect suspicious lesions, followed by a confirmatory biopsy. It requires a multidisciplinary approach – radiologists, pulmonologists or gastroenterologists (for scoping and biopsies), and pathologists all play a role. Early diagnosis improves the chances of effective treatment, but unfortunately, most cases are diagnosed at a late stage due to the diagnostic difficulties discussed.
8. Treatment Options
Mesothelioma treatment is complex and often requires a multimodal approach – combining surgery, chemotherapy, and radiation – tailored to the patient’s case. The rarity of mesothelioma means there have been relatively few large clinical trials, but standard care has evolved in recent decades. Key treatment modalities include:
1. Surgery: Surgery can offer the best chance of long-term control for early-stage mesothelioma, particularly pleural mesothelioma that is confined to one side of the chest. The goal is to remove as much tumor as possible (macroscopic complete resection). Two main surgical procedures are:
Extrapleural Pneumonectomy (EPP): An aggressive surgery where the entire lung on the affected side is removed along with the pleura, diaphragm (replaced with a patch), and pericardium (also reconstructed). This aims to excise all visible tumor in the chest en bloc. EPP is a very extensive operation with high risk; it’s usually offered to a small subset of patients who are fit enough and have disease not yet spread to lymph nodes.
Pleurectomy/Decortication (P/D): A lung-sparing surgery where surgeons remove all visible tumor and the pleural lining but leave the lung intact. They “decorticate” the lung by peeling the tumor off. P/D may also involve removing parts of the diaphragm or pericardium if those are involved, but it attempts to preserve lung function. It has lower mortality and morbidity than EPP and has become increasingly favored at specialty centers, as some studies show similar survival outcomes to EPP with better quality of life.
Surgery is more often an option in epithelioid subtype (less aggressive cell type) and if the mesothelioma is in an early stage (no distant spread). If lymph nodes or other organs are already involved, surgery alone cannot cure it, but sometimes surgery is still done for cytoreduction (debulking) in combination with other treatments.
For peritoneal mesothelioma, the surgical approach is Cytoreductive Surgery (CRS). Surgeons remove as many tumor implants from the abdominal cavity as possible – this can involve resecting parts of organs or stripping the peritoneum. Because peritoneal mesothelioma often spreads diffusely, the surgery can be extensive, but complete gross removal of tumor is the goal. CRS is almost always paired with heated chemotherapy delivered to the abdomen during surgery (see HIPEC below).
2. Chemotherapy: Systemic chemotherapy is a cornerstone for mesothelioma treatment, especially when surgery isn’t possible. The standard first-line chemotherapy regimen for pleural mesothelioma (established since 2004) is pemetrexed (Alimta) plus a platinum drug (cisplatin or carboplatin). Pemetrexed is an antifolate that, when combined with cisplatin, was shown to improve survival by a few months over cisplatin alone. Patients on pemetrexed receive vitamin B12 and folic acid supplements to reduce side effects. If cisplatin is too hard on a patient’s kidneys or overall health, carboplatin is substituted with slightly less toxicity (at some cost to efficacy). This chemo combination can shrink tumors or slow their growth in a significant subset of patients, improving symptoms and survival time.
In some cases (especially in epithelioid mesothelioma), adding an anti-angiogenesis drug like bevacizumab (which inhibits VEGF, a blood vessel growth factor) to pemetrexed-cisplatin has shown additional benefit. Bevacizumab plus chemo has become part of standard care in certain countries for patients who can tolerate it, as it extended median survival in a clinical trial.
For peritoneal mesothelioma, after cytoreductive surgery, a special chemotherapy technique called HIPEC (Heated Intraperitoneal Chemotherapy) is used. During the surgery, after removing visible tumors, a heated chemotherapy solution (often containing cisplatin and other drugs) is circulated in the abdominal cavity for about 60-90 minutes and then drained. HIPEC delivers high chemo concentrations directly to any remaining cancer cells in the abdomen and the heat helps enhance the drug’s effect. This approach has significantly improved outcomes in peritoneal mesothelioma compared to chemo given by vein alone – some patients achieve multiple years of disease control with CRS + HIPEC.
If initial treatment fails or the cancer returns, second-line chemotherapies may be tried (gemcitabine, vinorelbine, or newer agents in trials), but effective second-line options are limited.
3. Immunotherapy: In recent years, immunotherapy has become a breakthrough for mesothelioma. In 2020, the FDA approved a combination of two immunotherapy checkpoint inhibitors – nivolumab (Opdivo) and ipilimumab (Yervoy) – as a first-line treatment for unresectable malignant pleural mesothelioma. Nivolumab blocks the PD-1 pathway and ipilimumab blocks CTLA-4, both of which are “brakes” on T-cells; blocking them helps the immune system attack cancer cells. A clinical trial showed this combo improved overall survival in mesothelioma patients who weren’t candidates for surgery, compared to chemotherapy alone. Now, this immunotherapy regimen is an alternative to chemo for many patients, especially non-epithelioid subtypes which respond poorly to chemo.
Other immunotherapy approaches under investigation or in use include:
- Pembrolizumab (Keytruda): A PD-1 inhibitor that has shown some success in mesothelioma patients after chemotherapy, with a fraction experiencing tumor shrinkage. It’s not formally approved for mesothelioma yet (as of 2025) but is used off-label or in trials for those who have progression after standard treatments.
- CAR T-cell Therapy: Experimental trials are using Chimeric Antigen Receptor T-cells engineered to target mesothelioma cells (for example, CAR T-cells targeting mesothelin, a protein often overexpressed in mesothelioma). Early-phase trials have shown this is feasible, though still in research stages.
- Cancer Vaccines and Dendritic Cell Therapy: These attempt to “teach” the patient’s immune system to recognize mesothelioma. For instance, dendritic cell vaccines have been tested in Europe: patient immune cells are loaded with mesothelioma antigens and re-injected. Results so far are preliminary.
- Other Checkpoint Inhibitors: Trials combining checkpoint inhibitors with chemotherapy or with each other are ongoing to see if outcomes can improve further.
4. Radiation Therapy: Radiation has a role but must be used carefully because mesothelioma often involves a wide area and vital organs.
- Adjuvant Radiation: After surgery (especially after EPP, where an entire lung is removed), radiation can be applied to the hemithorax to kill residual microscopic disease. Techniques like Intensity-Modulated Radiation Therapy (IMRT) are used to focus radiation on the pleura while sparing the remaining lung or other organs. Postoperative radiation can reduce local recurrence in the chest, though it carries risks of lung inflammation or heart injury if not precisely delivered.
- Palliative Radiation: Radiation is very useful for symptom relief. Even if curing the disease is not possible, radiating a focal painful area (for example, a tumor mass invading the chest wall causing pain) can shrink that tumor and alleviate pain. Radiation can also help relieve superior vena cava syndrome or shrink tumors compressing airways to improve breathing. Doses in the palliative setting are lower and aimed at quality of life.
One challenge is mesothelioma tends to wrap around surfaces, so delivering a lethal dose to all tumor areas without harming normal tissue is difficult. Still, in specialized centers, radiation is a key component of multimodal therapy for select patients.
5. Emerging and Targeted Therapies: Researchers are testing novel treatments:
- Tumor Treating Fields (TTF): This is an FDA-approved device therapy for unresectable pleural mesothelioma. It involves wearing a device on the chest that emits low-intensity alternating electric fields which disrupt cancer cell division. TTF (marketed as Optune Lua) combined with chemotherapy showed improved survival in a trial, leading to its approval. Patients wear it for many hours a day. It’s a newer modality and not yet widely available, but it represents a non-drug, non-radiation treatment option.
- Targeted Therapy: Because mesothelioma doesn’t usually have the kind of mutations (like EGFR or ALK) seen in other cancers, traditional targeted therapy has been challenging. However, trials are looking at drugs targeting mesothelin (an antigen on mesothelioma cells) – for example, anetumab ravtansine (an anti-mesothelin antibody-drug conjugate) and amatuximab (a mesothelin antibody). Other targets like the angiogenesis pathway (VEGF inhibitors like bevacizumab, as mentioned) and pathways related to BAP1 mutations or PI3K signaling are in study. Thus far, no targeted small-molecule drug is standard yet.
- Gene Therapy: Experimental approaches include delivering genes into the tumor to fight the cancer. One approach used a modified virus to deliver the gene for interferon-alpha into mesothelioma tumors, hoping the tumors would then produce this immune-stimulating protein. Another futuristic idea is CRISPR-based gene editing to correct or disrupt genes in the tumor microenvironment, but this is still theoretical.
6. Supportive/Palliative Care: Regardless of curative treatment, symptom management is crucial:
- Pleural Effusion Management: Doctors may perform pleurodesis (instilling talc or chemicals in the pleural space to stick the lung to chest wall and prevent fluid re-accumulation). Alternatively, an indwelling pleural catheter can be placed so patients can drain fluid at home periodically. These measures significantly improve breathing comfort.
- Ascites Management: Repeated paracentesis (draining abdominal fluid) or, occasionally, a peritoneal catheter can help with comfort in peritoneal mesothelioma. In some cases, HIPEC as a treatment also addresses ascites for a time.
- Pain Control: Mesothelioma can cause severe pain. High-dose analgesics, including opioids, nerve blocks, or even procedures like an epidural or nerve cordotomy, may be used to control pain. Palliative radiation as mentioned also helps pain in some cases.
- Other Symptoms: Oxygen therapy for breathlessness, nutritional support and appetite stimulants for weight loss, and counseling/support groups for psychological impact are all parts of comprehensive care.
Multidisciplinary Approach: Treatment planning for mesothelioma is ideally done by a team of specialists (surgeons, medical oncologists, radiation oncologists, pulmonologists, etc.) at experienced centers. Because mesothelioma is rare, outcomes are generally better at high-volume centers that have expertise in these multimodal treatments. Clinical trial enrollment is strongly encouraged whenever available, as new therapies are continually being investigated.
Clinical Outcomes: With modern multimodal therapy, select patients (particularly those with early-stage epithelioid mesothelioma) have achieved extended survival. Some have lived 3-5 years or more, especially if a good surgical resection was achieved and followed by chemo/radiation. For instance, adding immunotherapy can push some unresectable cases to 18+ months median survival vs ~12 months on chemo. However, for advanced cases that cannot be resected, treatment is often palliative – aiming to prolong life modestly and relieve symptoms. No treatment is yet curative for most mesotheliomas, but the combination of therapies can improve quality and quantity of life in many cases.
In summary, standard treatment for mesothelioma might involve surgery (if feasible) plus chemotherapy, with radiation or newer therapies as adjuncts. Each patient’s plan is individualized based on their cancer’s stage and their health. The field is evolving, with immunotherapy and other innovations offering new hope where conventional therapies have had limited success.
9. Prevention & Precautionary Measures
There is no guaranteed way to prevent mesothelioma, but since the primary cause is known, preventive efforts focus on eliminating or reducing asbestos exposure. Key measures include:
Avoid or Limit Asbestos Exposure: The most effective prevention is simply not being around asbestos. Asbestos use has been banned or strictly regulated in many countries. For individuals, this means:
- Workplace Safety: If you work in industries with potential asbestos (construction, ship maintenance, old building renovation, brake repair, etc.), follow all safety protocols. Employers are required (in many jurisdictions) to identify asbestos hazards and provide training and protective equipment. Wear protective gear such as approved respirators when handling asbestos or disturbing old insulation. Use proper ventilation and containment procedures. Do not eat or drink in areas where asbestos dust may be present.
- Hygiene Practices: Workers should change out of work clothes and shower before going home if they’ve been in an asbestos-contaminated environment. Work clothes should be left at the worksite or washed separately to avoid bringing fibers home. These practices prevent secondary exposure to family members.
- Occupational Health Monitoring: In some regions, workers with known asbestos exposure undergo regular health check-ups, including chest X-rays or lung function tests, to catch early signs of asbestos-related disease. While no screening guarantees catching mesothelioma early, monitoring can detect changes like pleural plaques or effusions that prompt further investigation.
- Regulatory Compliance: Employers and contractors must comply with laws on asbestos. For example, in the UK the Control of Asbestos Regulations 2012 mandate surveying buildings for asbestos and safely removing it by licensed professionals. Awareness of and adherence to such regulations is critical in prevention.
Safer Home Environments: Many homes and buildings (especially built mid-20th century) contain asbestos in insulation, floor tiles, siding, or ceiling materials. Do not disturb asbestos-containing materials if they are in good condition – undisturbed asbestos usually isn’t dangerous. If you plan renovations:
- Professional Asbestos Inspection: Have a trained inspector check for asbestos before demolition or remodeling. Materials like popcorn ceilings, old linoleum, pipe insulation, and boiler insulation are common culprits.
- Professional Removal: If asbestos needs to be removed, hire licensed asbestos abatement professionals. Never attempt to remove asbestos yourself by scraping or breaking it; this can release large amounts of fibers. Professionals use techniques like wetting the material (to minimize dust) and special HEPA vacuums, as well as proper disposal methods.
- If Asbestos is Present but Intact: Often the advice is to leave it alone or encapsulate it (seal it with a specialized coating) rather than remove it, because removal can create an exposure risk if not done properly. Ensure family members know not to disturb such material.
Public Health and Policy: On a larger scale, prevention involves legislation. Many countries have banned asbestos (e.g., all forms banned in the EU, UK by 1999, Australia by 2003, etc.). However, some countries still use it. Advocating for global bans and enforcement of existing regulations is important to reduce future mesothelioma cases. Additionally, tracking and safe disposal of existing asbestos (like in old buildings and ship graveyards) is a societal challenge.
Precautionary Medical Measures: Currently, no vaccine or medication exists to prevent mesothelioma. Unlike infectious diseases, cancer isn’t something you can vaccinate against (aside from viruses that cause cancer, which is not the case for mesothelioma). Researchers are exploring chemoprevention – for example, whether certain anti-inflammatory drugs or other agents could be given to asbestos-exposed individuals to reduce cancer risk, but nothing definitive has been established. One experimental approach has been studying whether high-dose antioxidants or interferon therapies could mitigate the asbestos effects, but evidence is not conclusive.
Lifestyle Factors: While lifestyle (smoking, diet, etc.) doesn’t directly cause mesothelioma, maintaining good lung health and general health can be precautionary in a broad sense. If someone has a history of asbestos exposure, not smoking is crucial – not because of mesothelioma, but because the combination of smoking and asbestos dramatically raises the risk of lung cancer, compounding health issues. A healthy lifestyle can also improve lung reserve, possibly helping one better tolerate early disease or treatments should mesothelioma occur.
Awareness and Early Action: People who know they’ve been exposed to asbestos should inform their doctors and be vigilant for symptoms. There is no formal screening, but some doctors might perform periodic imaging for peace of mind. Being aware of mesothelioma’s early signs and informing healthcare providers of past asbestos exposure can lead to earlier diagnosis. For example, if a person with asbestos exposure develops a persistent cough or chest pain, they should mention their exposure history so that mesothelioma is considered, not just routine bronchitis.
Future Preventive Strategies: Research is ongoing to find ways to intervene during the long latency period of mesothelioma. Some animal studies suggest that certain interventions (even something as simple as regular aerobic exercise was studied in mice) might slow down carcinogenesis after asbestos exposure. Also, scientists like those at Fox Chase Cancer Center are investigating **drug candidates that could be given after asbestos exposure to delay or prevent mesothelioma. While promising, these are not yet available to the public.
In conclusion, the best precaution is strict avoidance of asbestos. For those already exposed, minimizing additional exposure and closely monitoring health is key. Mesothelioma cases today largely stem from past asbestos use; by preventing exposure now, we protect future generations from this disease. The impact of asbestos bans will be seen in coming decades as mesothelioma incidence hopefully declines.
10. Global & Regional Statistics
Mesothelioma incidence and outcomes vary around the world, reflecting historical asbestos use patterns and regulatory actions. Here are key global and regional statistics:
Global Incidence: In 2020, there were an estimated 30,000+ new cases of mesothelioma diagnosed worldwide. This makes mesothelioma a very rare cancer globally (for comparison, lung cancer cases are in the millions). The global incidence rate was about 0.30 cases per 100,000 population per year (or 0.3 per 100k) around that time. Although rare, mesothelioma is significant due to its strong link with industrial exposure and its severity.
Global Mortality: Mesothelioma caused roughly 26,000–30,000 deaths per year worldwide in recent years. The mortality closely tracks incidence because of the cancer’s high lethality. The World Health Organization (WHO) has noted over 30,000 mesothelioma deaths annually, with many cases likely underreported in countries where cancer registries are less developed.
Trends: Globally, mesothelioma incidence rose throughout the late 20th century as a result of widespread asbestos use after World War II. However, in some Western countries, incidence has plateaued or begun to decline after asbestos bans. For example, the United States saw mesothelioma rates increase from the 1970s, peak in the early 1990s, and then level off or slightly decrease in men by the 2010s. This reflects reduced occupational exposure due to regulations. In contrast, many developing countries (and some developed ones that were late to regulate asbestos) are still seeing increasing mesothelioma rates. Countries like China, India, Russia, and some in Southeast Asia, which continued using asbestos extensively into the 21st century, may face rising mesothelioma cases in coming decades.
High-Incidence Regions: The highest incidence rates (age-adjusted) have been reported in countries with heavy asbestos use in the past:
- United Kingdom: The UK, which used large amounts of crocidolite and amosite asbestos, has one of the world’s highest mesothelioma incidence rates. About 2,500 mesothelioma deaths occur annually in the UK (population ~66 million). This is roughly 40 per million (or 4 per 100,000) per year – very high. The UK’s incidence peaked around 2012 and is expected to gradually decline since asbestos was banned in 1999, but it remains a significant burden.
- Australia: Similar to the UK, Australia had high asbestos consumption (including mining its own asbestos at Wittenoom). Mesothelioma rates in Australia are among the highest globally, on par with the UK. With a smaller population (25 million), Australia sees about 700 mesothelioma cases a year, which is about 28 per million annually.
- Belgium and The Netherlands: Also report high incidences (~30 per million) due to heavy use in industries like shipyards and manufacturing.
- Italy: Certain areas (like Casale Monferrato, home to an Eternit asbestos cement factory) have high localized incidence. Italy overall has several hundred cases per year and banned asbestos in 1992.
- United States: The U.S. incidence is lower than the UK/Australia, partly due to different asbestos types used and earlier regulatory action. The U.S. has about 3,000 cases per year (roughly 10 per million, or 1 per 100,000). Incidence is higher in coastal areas with shipyards (e.g., around Seattle or Norfolk) and industrial areas.
- Japan: Japan had later asbestos bans (early 2000s) and is seeing rising cases, with an expected peak around the 2020s-2030s. Current cases are in the low thousands per year.
Low-Incidence Regions: Countries with minimal asbestos use or poor data may report very low incidence:
- Many African and some Latin American countries have <1 case per million (though asbestos use in these places was lower, and under-diagnosis is possible).
- For instance, Tunisia and Morocco were cited with incidence less than 1 per million.
- Some countries may not even have mesothelioma listed separately in cancer registries, potentially masking true numbers.
Gender Differences: Globally, about 80% of mesothelioma cases are in men. For example, U.S. CDC data in 2021 showed of ~2,800 cases, about 1,973 were men and 830 women. This reflects historical occupational exposure patterns. However, in some populations where environmental exposure (like erionite in Turkey) was common, women comprise a larger share.
Survival Rates: Mesothelioma has poor survival worldwide. The 5-year survival rate for pleural mesothelioma is around 5–10% in most studies. According to U.S. SEER data, the 5-year relative survival for all pleural mesothelioma is about 12%. If caught at a localized stage (which is uncommon), 5-year survival might be ~20–24%. Regional spread drops that to ~16%, and distant metastatic disease to ~7%. These numbers are similar across high-income countries. In lower-income countries, survival might be worse due to later diagnosis and less access to specialized care. Notably, peritoneal mesothelioma has seen improved survival in specialized centers using CRS/HIPEC, with some reports of median survival 3-5 years and 5-year survival of 50% in select patients – better than pleural form (because of effective local treatment). But globally, pleural mesothelioma dominates cases.
Regional Trends:
- North America & Western Europe: Many of these countries are now on the downturn of the mesothelioma epidemic, thanks to asbestos regulations. For example, U.S. mesothelioma deaths have slightly declined in men since the 1990s, but interestingly have remained steady or slightly increased in women (possibly due to second-hand exposure or longer lifespan).
- Eastern Europe & Russia: Some Eastern European countries still have increasing rates and a substantial burden, as asbestos was used extensively (often without adequate protection) and bans came later or not at all.
- Asia: A significant concern is that countries like China, India, Indonesia, and others have used asbestos in recent decades and some continue to import/use it. The mesothelioma incidence in these places is currently reported as low, but many cases might be missed or the boom is yet to come, given the latency. It’s feared that a wave of mesothelioma could occur mid-21st century in these regions if precautions aren’t taken.
- Oceania: Australia and New Zealand are managing high rates from past use. Australia’s rates might start declining after the 2020s due to the ban in 2003 and removal programs.
- Latin America: Brazil, once a major asbestos producer (until banning in 2017), still sees cases and likely will for decades. Other Latin countries with less industrialization have lower incidence but also may have under-reporting.
Global Burden and Disability: Mesothelioma also contributes to global disability-adjusted life years (DALYs) lost, though as a rare cancer its global share is small. However, for affected individuals, the personal and occupational disease burden is enormous. Many countries recognize mesothelioma as an occupational disease with compensation systems (e.g., worker’s compensation or specialized funds, like in the US and some European countries).
Unreported Cases: It’s worth noting that some analyses (e.g., by the International Agency for Research on Cancer) suggest a number of mesothelioma cases (especially in the developing world) go unreported or misdiagnosed (as lung cancer or other diseases). The true global incidence might be higher than current data, meaning the continued use of asbestos could be sowing seeds for future cases we’ll only see years later.
In summary, mesothelioma remains a global issue but with very uneven distribution. Developed nations that used asbestos heavily in the last century are dealing with (or just past) peak incidence and gradually seeing declines due to preventive measures. Meanwhile, developing nations might see rising numbers if asbestos exposure is not curtailed. Globally, tens of thousands are diagnosed and die from this disease each year, making prevention efforts critical worldwide.
11. Recent Research & Future Prospects
Research into mesothelioma is active, aiming to improve treatment outcomes and ultimately find a cure or effective prevention. Some of the latest advancements and future prospects include:
Improved Systemic Therapies: The recent introduction of immunotherapy is a major advancement. The combination of nivolumab + ipilimumab (dual checkpoint inhibition) approved in late 2020 was a breakthrough after years with no new drugs. Ongoing studies are looking at combining immunotherapy with chemotherapy as first-line treatment to see if that yields even better outcomes. For example, trials like DREAM (adding durvalumab, a PD-L1 inhibitor, to chemo) showed promising early results. Future protocols may involve triplet therapy (chemo + two immunotherapy agents) for fit patients if toxicity is manageable.
Personalized Medicine & Genomics: Scientists are performing genomic sequencing of mesothelioma tumors to identify targetable mutations or pathways. While mesotheliomas often have complex chromosomal losses (p16, BAP1, NF2 are commonly lost), targeted drugs are being tested. One example is tazemetostat, an EZH2 inhibitor, which has been tried in mesotheliomas with BAP1 mutations (BAP1 loss leads to EZH2 dependency). Early-phase trials show some activity. As our understanding of the tumor genetics improves, there is hope for precision medicine approaches – tailoring treatment based on a tumor’s molecular profile.
CAR-T and Cell Therapies: As mentioned, CAR-T cell therapy targeting mesothelin or other antigens is a cutting-edge research area. A recent small trial of anti-mesothelin CAR-T cells in advanced mesothelioma demonstrated it’s feasible and showed some tumor control, especially when combined with checkpoint inhibitors. This is still experimental, but future improvements in CAR-T design (e.g., armoring CAR-T cells to overcome the immunosuppressive tumor environment) might yield better results. Additionally, TIL (tumor-infiltrating lymphocyte) therapy, where a patient’s own immune cells from the tumor are expanded and re-infused, is being explored.
Tumor Microenvironment & Combination Therapies: Mesothelioma tumors create an immunosuppressive microenvironment. Research by Hiltbrunner et al. and others has described how asbestos-exposed mesothelial cells release certain chemokines (like CCL2) that attract tumor-promoting macrophages, and molecules like HMGB1 that drive inflammation and tumor growth. This understanding opens paths for therapy: for instance, drugs that block CCL2 or macrophage recruitment may help. Some trials are testing CD40 agonists (to activate macrophages to kill cancer) or CSF-1R inhibitors (to reduce immunosuppressive macrophages) in mesothelioma in combination with immunotherapy.
Novel Agents and Targets: Researchers are investigating a variety of new agents:
- Mesothelin-targeted therapies: Since mesothelioma cells often express mesothelin, new therapies include monoclonal antibodies, antibody-drug conjugates (like anetumab ravtansine), and immunotoxins (an example was SS1P, an anti-mesothelin immunotoxin). While none have made it to standard use yet due to mixed trial results, they continue to be optimized.
- Vaccines: Several approaches, such as a WT1 peptide vaccine (WT1 is a protein often expressed in mesothelioma) or dendritic cell vaccines, have shown some hints of efficacy. A Dutch trial of dendritic cell vaccine reported a few long-term survivors, which encourages further research.
- Oncolytic Viruses: These are viruses engineered to selectively infect and kill cancer cells and stimulate immunity. An oncolytic virus delivering the interferon-beta gene was studied in mesothelioma patients (the ONCOS-102 trial) and showed immune activation. Such viruses might be combined with other treatments for synergy.
- Epigenetic Therapy: Drugs that reverse epigenetic changes (like DNA methylation or histone deacetylation) are being examined. The idea is to restore expression of silenced tumor suppressor genes or make the tumor more recognizable to the immune system.
Better Diagnosis and Screening: Future prospects include developing improved biomarkers for earlier detection. Beyond SMRP and fibulin-3, researchers are looking at panels of markers or even new technologies like detecting circulating tumor DNA (ctDNA) in blood. If a reliable blood test can be found, it could potentially be used to screen high-risk populations (like asbestos-exposed workers) for early signs of mesothelioma before symptoms develop. Imaging advancements, like low-dose CT screening (effective in lung cancer for smokers), might also be evaluated in the future for asbestos-exposed individuals, though cost-effectiveness is an issue given mesothelioma’s rarity.
Genetic Risk and Prevention: The discovery of the BAP1 mutation’s role has led to the concept of a cancer predisposition syndrome. In the future, families known to carry BAP1 mutations could undergo enhanced surveillance for mesothelioma (and other cancers). There’s also exploration into chemoprevention for such high-risk groups – for example, could giving periodic anti-inflammatory drugs or other agents to someone with BAP1 mutation who was exposed to asbestos reduce their chance of mesothelioma? These questions are yet unanswered.
Multimodal Therapy Optimization: Current research is also refining how best to combine treatments. For instance, what is the optimal timing and sequencing of surgery, chemotherapy, and immunotherapy? Some trials are giving immunotherapy before surgery (neoadjuvant) to see if it can shrink tumors and kill microscopic disease, making surgery more effective. Others are focusing on maintenance therapy – e.g., after initial chemo or immunotherapy, should patients continue on a single immunotherapy drug for maintenance to prolong control? The role of prophylactic radiation to tract sites (to prevent tumor seeding at biopsy scars) is also being re-evaluated; historically it was done, but newer evidence has questioned its necessity.
Gene Editing and Future Tech: While still largely theoretical for direct therapy, CRISPR gene editing technology might one day be used to modify patients’ immune cells to better fight mesothelioma or even to correct genetic susceptibilities. Also, identifying why some people exposed to asbestos never get mesothelioma could reveal natural protective mechanisms that might be mimicked in therapy.
Robotic and Advanced Surgery: In the realm of surgery, some centers are adopting minimally invasive or robotic-assisted techniques for pleurectomy/decortication, which might reduce recovery time. Also, there is research into better ways to deliver intraoperative therapy, such as pressurized intrathoracic aerosol chemotherapy (PITAC) – essentially spraying chemotherapy in the chest during surgery to coat surfaces after tumor removal.
Quality of Life and Survivorship: Another important area is improving life for mesothelioma patients. Research into better pain control methods, management of breathlessness (like novel drugs or respiratory therapies), and supportive interventions (exercise programs, nutritional supplements) can significantly impact patient well-being.
Potential for Cure: Currently, a true cure (complete eradication of mesothelioma) is extremely rare. However, there are documented cases of long-term remission, especially in peritoneal mesothelioma treated aggressively with CRS/HIPEC and in occasional pleural cases treated with multimodality therapy. As treatments improve, the hope is that more patients will achieve long-term survival and possibly cure. For instance, a combination of surgery, targeted therapy (for microscopic disease), and immunotherapy might one day render a patient cancer-free if all goes perfectly.
In summary, the future of mesothelioma treatment is focused on harnessing the immune system, targeting tumor biology more precisely, and catching the disease earlier. With global mesothelioma incidence still rising in some areas, these advancements are urgently needed. The integration of emerging therapies like CAR-T cells, gene therapy, and personalized medicine offers a hopeful outlook that mesothelioma outcomes will continue to improve. Researchers around the world – from oncology labs to clinical trial consortia – are dedicated to changing mesothelioma from a near-certain fatal diagnosis to a more manageable, and one day perhaps curable, condition.
12. Interesting Facts & Lesser-Known Insights
Beyond the standard information, mesothelioma has several fascinating and lesser-known aspects:
Not Just a “Lung Cancer”: A common misconception is that mesothelioma is a type of lung cancer. In fact, it is a distinct cancer of the lining of organs, not the lung tissue itself. Lung cancers occur inside the lungs and are usually linked to smoking, whereas pleural mesothelioma surrounds the lung and is linked to asbestos. This distinction is important because they are treated differently. Mesothelioma can also occur in places where lung cancer doesn’t (abdomen, heart lining, etc.), which surprises many.
Long Latency – A Time Capsule Disease: Mesothelioma often appears 20 to 50 years after asbestos exposure. This extremely long latency is longer than many other environmentally caused diseases. It means that mesothelioma cases we see today may be due to exposures in the 1960s-1980s. Likewise, people exposed in the 2000s might not develop disease until 2040s-2050s. This “time capsule” effect has made it challenging to track and also allowed the asbestos industry in the past to downplay health effects (since the cause and effect were so separated in time).
Familial Mesothelioma: While mesothelioma itself is not contagious or directly inherited, there are families with multiple members having mesothelioma due to shared exposures and genetics. The discovery of the BAP1 mutation in some families showed a hereditary component in a subset of cases. People with BAP1 tumor predisposition syndrome often develop mesothelioma (usually at a younger age and sometimes with less asbestos exposure than typical). They might also develop other cancers like uveal (eye) melanoma, skin melanomas, and kidney cancer. This is a rare scenario but interesting as it provides a genetic link to an otherwise exposure-driven disease.
Testicular Mesothelioma: Mesothelioma of the tunica vaginalis (testicular lining) is extremely rare and accounts for less than 1% of cases. Fewer than a few hundred cases have ever been documented. Often it presents as a hydrocele (fluid around the testicle) or a testicular lump and is usually found during surgery for what is thought to be something else. Because of its rarity, there’s no standardized treatment, but it typically involves removing the affected testis and cord (orchiectomy). Some patients also receive chemotherapy similar to pleural mesothelioma if there’s spread. Its cause isn’t as clearly linked to asbestos as pleural/peritoneal mesotheliomas, but about half the patients report asbestos exposure. This is a reminder that mesothelioma can occur in unusual locations.
Erionite and “Turkey’s Mesothelioma Villages”: In certain villages in Cappadocia, Turkey, an astonishingly high rate of mesothelioma was observed – in some families, 50% of deaths were due to mesothelioma. This was eventually traced not to commercial asbestos, but to a natural fiber called erionite present in local white volcanic rock used to build homes. Erionite is even more potent than asbestos in causing mesothelioma. This discovery in the 1970s-80s was a dramatic epidemiological story and led to relocation of affected villages. It also highlighted that other fibrous silicates can cause mesothelioma, and genetic susceptibility played a role too (certain families were more affected, suggesting an interaction of genetics with erionite exposure).
Legal and Societal Impact: Mesothelioma has had a profound impact outside medicine – particularly in law and occupational safety. It has been at the center of countless lawsuits against asbestos manufacturers and employers. The famous “Mesothelioma – you may be entitled to compensation” ads in the U.S. are a reflection of how mesothelioma is almost always considered an industrial disease. Companies have paid billions in settlements, and many went bankrupt (some set up trust funds for victims). This legal aspect is unique; few cancers are so tightly linked to workplace negligence and have seen such courtroom attention. The first mesothelioma lawsuits emerged in the 1960s and by the 1970s, they were widespread in the U.S.. These cases greatly raised public awareness about asbestos hazards.
All Types of Asbestos Are Dangerous: A myth propagated by the asbestos industry was that some forms of asbestos (notably white asbestos, or chrysotile) are “safer” and do not cause mesothelioma. While blue (crocidolite) and brown (amosite) asbestos are indeed more carcinogenic, evidence shows chrysotile also causes mesothelioma. Chrysotile fibers, when inhaled, can eventually reach the mesothelium (some may translocate as smaller fibrils). So, no asbestos type is “safe.” Additionally, even low levels of exposure can in some cases cause disease – there have been mesothelioma cases in people with apparently minimal asbestos contact (though often deeper investigation finds some exposure in the environment or a summer job, etc.).
Mesothelioma in Women and Children: It’s less common, but mesothelioma can and does occur in women and even, rarely, in children. Women often have had second-hand exposure (like washing a spouse’s clothes or living near an asbestos factory). What’s intriguing is that a higher proportion of women have no known asbestos exposure compared to men. Some of these could be due to unidentified environmental contact, but it raises questions about other causes or hormonal factors that are not fully understood. Childhood mesothelioma is extremely rare; when it happens, it’s usually not linked to asbestos. Researchers have looked for other causes (like genetic mutations or prior radiation) in these cases. One speculation for sporadic cases (especially peritoneal in younger patients) is a possible role of spontaneous genetic changes or even maternal asbestos exposure (if a mother had fibers in her body that transplacentally reached the fetus – not proven, but hypothesized).
Myths Debunked: A few myths:
- Myth: “Smoking causes mesothelioma.” Fact: Smoking by itself does not cause mesothelioma. However, because many asbestos workers also smoked, people conflate the risks. Smoking does cause lung cancer and the combination of smoking+asbestos mainly yields lung cancer or asbestosis, not mesothelioma.
- Myth: “Mesothelioma can be cured by alternative therapies.” Unfortunately, because of the poor prognosis, many patients search for alternative cures. While good nutrition, supplements, or practices like meditation can help well-being, there is no evidence that any alternative treatment can cure mesothelioma. Approaches like high-dose vitamin C, special diets, or herbal remedies have been tried anecdotally, but none have proven to control the disease. Patients should be cautious of unproven claims.
- Myth: “Everyone exposed to asbestos will get mesothelioma.” Fact: Only a minority of those heavily exposed get mesothelioma (for example, 20% or less of heavily exposed insulation workers developed it). Many more will get lung scarring or lung cancer. Mesothelioma risk seems influenced by individual susceptibility. However, because we cannot predict who among the exposed will get it, all asbestos exposure is considered unsafe.
- Myth: “Mesothelioma is immediately fatal.” Fact: While prognosis is poor on average, it’s not instant. Many patients live a year or more, and some live several years, especially with treatment. Each case is individual. There are rare stories of near-complete responses to treatment and long-term remission.
Occupational Shifts: Interestingly, as primary asbestos use has dropped, the profile of at-risk occupations has subtly shifted. While traditional jobs (like shipyard or mining) are still relevant for older generations, today’s mesothelioma patients may include those with indirect exposures. For example, disaster responders (like those at the World Trade Center site in 2001) were exposed to pulverized asbestos; some of them have developed mesothelioma years later. Another example: teachers or office workers in old buildings with crumbling asbestos insulation can develop mesothelioma – an occupation not classically “at risk” but due to building environment they were exposed. This broadens the need for awareness beyond just industrial workers.
Research Curiosities: One interesting line of research is the role of iron in mesothelioma. Asbestos fibers can carry iron (especially amosite which is iron-rich), and deposits of iron in tissues (as seen by “asbestos bodies” in the lung) might contribute to carcinogenesis via generating free radicals. There was even a trial of an iron-chelating drug (deferoxamine) to see if removing iron slows mesothelioma – it didn’t have much effect, but it shows the creative angles researchers explore.
Mesothelioma in Animals: It’s not just humans – animals can get mesothelioma too. Notably, some pet dogs have developed mesothelioma from exposure to asbestos (e.g., living in the same home as an exposed worker). Veterinary cases are rare but documented. Additionally, certain simian (monkey) populations used in lab research that were incidentally exposed to SV40 or asbestos also developed mesotheliomas, which helped in understanding the disease.
Each of these facts underscores mesothelioma’s uniqueness: from its strong environmental cause and long latency to its legal implications and ongoing scientific puzzles. As awareness increases, myths are dispelled and both prevention and early diagnosis can improve. Mesothelioma’s story – entwined with industrial history, medicine, law, and personal tragedy – makes it a particularly compelling and important disease to understand and combat.
Sources:
- Syed HA, Wallen JM. Malignant Mesothelioma. StatPearls. 2025 – “Malignant mesothelioma is a rare and aggressive tumor arising from mesothelial cells forming the lining layers of the body’s viscera… While mesothelioma can develop in any mesothelial layer, such as the peritoneum or pericardium, the pleural layer is most commonly affected”.
- Tipu SA et al. Malignant mesothelioma. PMC. 2013 – “Malignant Mesothelioma (MM) is a rare but rapidly fatal and aggressive tumor of the pleura and peritoneum… The earliest mention of a possible tumor of the chest wall (the pleura) was made in 1767 by Joseph Lieutaud… Peritoneal mesothelioma was first described in 1908 by Miller and Wynn.”.
- StatPearls – Epidemiology – “Malignant pleural mesothelioma has an incidence of ~2500 new cases annually in the US… The disease predominantly affects males… average age at diagnosis of 72. There is usually a latency period of 20 to 40 years between asbestos exposure and diagnosis.”.
- Asbestos.com (Mesothelioma History) – “J.G. Adami coined the term ‘mesothelioma’ to classify this rare cancer (1909).”; “1960: J.C. Wagner published a study of 33 mesothelioma cases linked to an asbestos mine in South Africa. It confirmed the causal relationship beyond a reasonable doubt.”.
- Cancer Research UK – “Asbestos is the biggest cause of mesothelioma… In the UK, exposure to asbestos causes more than 95% of mesothelioma in men, almost 85% in women.”.
- StatPearls – Etiology – “Inhaling asbestos fiber can lead to repeated pleural inflammation, disruption of cellular mitosis, activation of proto-oncogenes, and the generation of free radicals… some studies suggest links between malignant pleural mesothelioma and other risk factors, including ionizing radiation (e.g., mantle radiation for Hodgkin lymphoma) and genetic predispositions: germline BAP1 mutations.”.
- StatPearls – Occupational exposure – “Occupational asbestos exposure is a key determinant… Professions associated with high asbestos exposure include shipbuilding, mining, ceramics manufacturing, cement manufacturing involving asbestos, auto parts production (brake lining), insulation work, railroad repair.”.
- American Cancer Society – Signs & Symptoms – Lists pleural symptoms (chest pain, shortness of breath, cough, trouble swallowing, hoarseness, swelling of face/arms); peritoneal symptoms (abdominal pain, swelling, nausea/vomiting, constipation); pericardial (chest pain, irregular heartbeat, murmur, short breath); general symptoms (fever, sweating, fatigue, weight loss, blood clots, appetite loss).
- Cancer Research UK – Symptoms – “Early stage mesothelioma doesn’t usually cause many symptoms. But mesothelioma can cause symptoms as it grows… Symptoms of pleural mesothelioma include chest pain, shortness of breath, tiredness (fatigue), sweating and high temperatures, persistent cough, losing weight when not dieting, loss of appetite, difficulty swallowing, hoarse voice, finger clubbing.”. Symptoms of peritoneal mesothelioma include “pain in the abdomen, swelling in the abdomen, feeling or being sick, poor appetite, losing weight, diarrhoea or constipation.”.
- Mayo Clinic – Complications – “As pleural mesothelioma spreads in the chest, it puts pressure on structures in that area. This can cause complications such as trouble breathing, chest pain, trouble swallowing, pain caused by pressure on nerves and spinal cord, buildup of fluid in the chest (pleural effusion) that can press on the lung and make breathing hard.”.
- Canadian Cancer Society – Supportive Care – “Pleural effusion is common with pleural mesothelioma… fluid can press on the lung making it hard to breathe… fluid may be drained (thoracentesis) or surgery to seal the pleura (pleurodesis) so fluid can’t build up.”. “Ascites… Most people with peritoneal mesothelioma develop ascites… fluid may be drained (paracentesis)… chemotherapy drugs put directly into abdomen (catheter).”. “Peritoneal mesothelioma can cause bowel obstructions… symptoms include pain, cramps, abdominal swelling, no bowel movements, nausea and vomiting.”. Also notes loss of appetite leading to weight loss and cachexia, and fatigue is very common.
- American Cancer Society – How is Mesothelioma Diagnosed? – “Mesothelioma can be hard to diagnose… tests must be done to find out what’s causing symptoms… These could include imaging tests, blood tests, and/or biopsies.”. “Chest x-ray: findings that might suggest mesothelioma include pleural thickening, calcium deposits on pleura, fluid between lungs and chest wall, or lung changes from asbestos exposure.”. “CT scans are often used to help look for mesothelioma and to find the exact location… show if cancer has spread to other organs… help decide if surgery is an option.”. “Echocardiogram may be done if fluid around heart is suspected.”.
- American Cancer Society – Blood tests – “Blood levels of certain substances are often higher in people with mesothelioma: Fibulin-3, Soluble mesothelin-related peptides (SMRPs). Mesothelioma can’t be diagnosed with these blood tests alone, but high levels make the diagnosis more likely. These tests are not routinely used because of limited value.”.
- American Cancer Society – Biopsy – “The actual diagnosis is made by removing cells from an abnormal area and looking under a microscope. This is called a biopsy… If fluid buildup is present, a sample of fluid can be removed via thoracentesis, paracentesis, or pericardiocentesis and examined for cancer cells… If cancer cells are found, special tests are done to see if it’s mesothelioma… Even if no cancer cells are found in fluid, a person might still have cancer. Often doctors need an actual sample of the mesothelium (pleura, peritoneum, or pericardium) to know if it’s mesothelioma.”. “Needle biopsies… a long needle is passed through the skin into pleura, often CT-guided, to take small samples… Needle biopsies are less invasive but sometimes the sample isn’t big enough to make an accurate diagnosis, especially true for mesothelioma.”.
- American Cancer Society – Key Statistics – “Mesothelioma is fairly rare in the United States. About 3,000 new cases are diagnosed each year… Rate increased from 1970s to early 1990s, but since then leveled off and even gone down slightly (in men, likely due to changes in workplace asbestos exposure)… Rate in women is lower and has been steady. In many other countries, the rate of mesothelioma is still increasing.”. “Mesotheliomas are much more common in older people than younger… average age in chest is 72.”.
- StatPearls – Treatment/Management – “Management typically involves a multimodal approach, incorporating surgery, systemic therapies, radiation, and supportive care. The plan is tailored to stage, subtype, and patient’s performance status.”. “Surgery: indicated for early-stage to achieve complete resection. Extrapleural pneumonectomy (radical, removes pleura, lung, pericardium, diaphragm) – high morbidity, reserved for select patients. Pleurectomy and decortication – lung-sparing alternative, removes pleura/tumor, preserving lung; lower complication rates and comparable survival, increasingly favored.”. “Systemic therapy: Chemo – standard is pemetrexed with cisplatin or carboplatin, with folic acid/B12 to reduce toxicity. In eligible patients, addition of bevacizumab (VEGF inhibitor) may enhance efficacy. Immunotherapy – combination checkpoint inhibitors (nivolumab + ipilimumab) are FDA-approved for unresectable mesothelioma, showing improved survival; single-agent pembrolizumab may be considered in refractory cases.”. “Radiation: Adjuvant IMRT post-op is used to reduce local recurrence, especially after EPP. Palliative radiation for symptom management (chest wall pain, dyspnea).”. “Emerging therapies: Tumor Treating Fields – novel therapy using alternating electric fields, approved in combination with chemo for unresectable pleural mesothelioma. Targeted therapies – research into agents targeting mesothelin, BAP1 mutations, etc., showing promising results. Gene and cell therapies – trials exploring CAR-T cells and gene-editing strategies.”. “Supportive care: Pleural interventions (indwelling catheters or pleurodesis) for recurrent effusions. Symptom management (pain control, nutrition, psychosocial care) is essential for quality of life.”. “Multidisciplinary team at a high-volume center is advised for optimal outcomes; clinical trials encouraged for eligible patients.”.
- Annals of Translational Medicine (Kim et al. 2017) – Peritoneal Mesothelioma Review – “Untreated, life expectancy <1 year. Cytoreductive surgery (CRS) with heated intraperitoneal chemotherapy (HIPEC) has become the mainstay of therapy… systemic therapies still being developed.”.
- MDPI Cancers (Dolzan et al. 2022) – Novel Future Treatments Review – “Traditionally, treatment is trimodal (surgery, chemo, radiotherapy). Introduction of chemotherapy improved OS. However, pemetrexed/cisplatin regimen hasn’t changed since 2004. Novel combo of ipilimumab + nivolumab approved in late 2020. Review summarizes novel approaches in immunotherapy, vaccines, CAR-T… Immunotherapy that was swift in other thoracic malignancies was slow to reach desirable endpoints in mesothelioma, possibly due to limited patient numbers. Novel approaches like CAR-T being investigated. As incidence still rising globally, novel options based on better understanding of microenvironment and genetics are needed for future precision therapies.”. “Mesothelioma is a rare disease with over 30,000 new cases worldwide in 2020. Mortality was over 26,000, representing 45% of all new cases in Europe in 2020. Incidence has risen due to asbestos exposure. Latency over 25 years. Under-reporting in middle/lower income countries means rise may be higher in some places.”.
- Asbestos.com – Mesothelioma Statistics – “A recent study found an estimated 30,000 deaths occur globally from mesothelioma each year.”. “In 2021 CDC data, out of 2,803 diagnosed cases in US, 1,973 were men and 830 women.”.
- American Cancer Society – Survival Statistics – “5-year relative survival for pleural mesothelioma (2012-2018 diagnoses): Localized = 24%; Regional = 16%; Distant = 7%; All stages combined = 12%. (These are relative to normal population and based on earlier patients; current patients may have better outlook with improved treatments.)”