Acne
What is Acne?
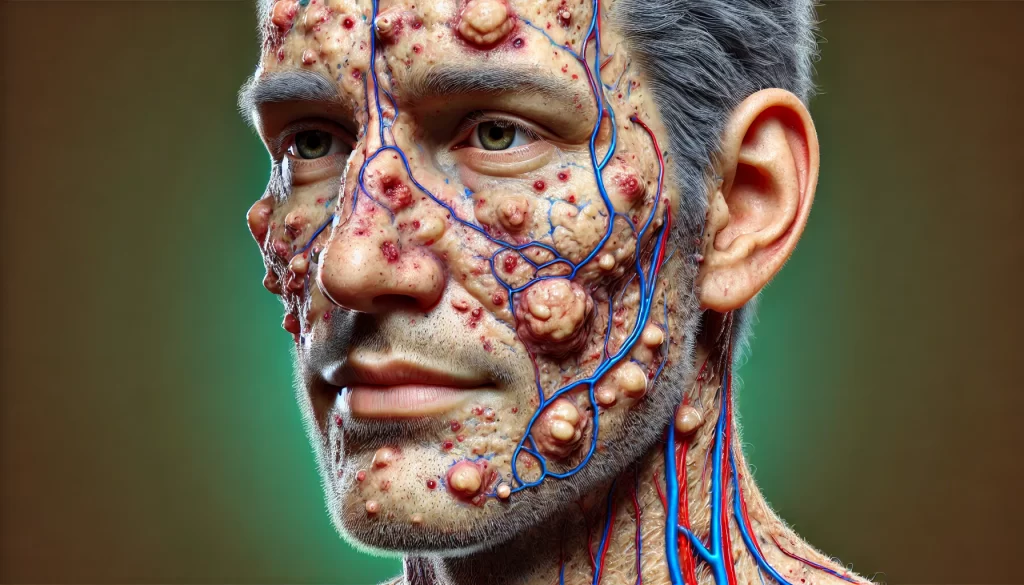
Acne is a common skin condition that affects most people at some stage of life. It leads to the development of spots, oily skin, and, in some cases, skin that is warm or painful to touch. Acne commonly appears on the:
- Face – affecting nearly everyone with acne.
- Back – impacting more than half of acne sufferers.
- Chest – affecting around 15% of people with acne.
Types of Spots Caused by Acne
Acne can cause different types of spots, including:
- Blackheads: Small black or yellowish bumps that form on the skin. They aren’t caused by dirt but appear dark due to pigmentation from the inner lining of the hair follicle.
- Whiteheads: Similar in appearance to blackheads but firmer and won’t empty when squeezed.
- Papules: Small red bumps that may be tender or sore.
- Pustules: Papules with a white tip caused by pus buildup.
- Nodules: Hard, painful lumps beneath the surface of the skin.
- Cysts: The most severe form of acne, cysts are large pus-filled lumps resembling boils and carry the greatest risk of permanent scarring.

Causes of Acne
Acne is primarily linked to hormonal changes, particularly during puberty. However, it can start at any age due to several factors:
- Hormonal Fluctuations: Increased hormone levels can stimulate the oil-producing glands next to hair follicles, causing excess sebum production. This leads to blocked pores and the growth of P. acnes bacteria, causing inflammation.
- Genetics: Acne often runs in families. If both parents had acne, there is a higher chance you will also experience it.
- Hormonal Changes in Women: Menstruation, pregnancy, and hormonal conditions can trigger episodes of acne.
Contrary to common myths, diet, poor hygiene, or sexual activity are not proven to cause acne.
Who is Affected?
- Acne commonly affects 80% of people aged 11 to 30.
- Girls are most affected between ages 14 to 17 and boys between ages 16 to 19.
- While most people outgrow acne by their mid-twenties, 5% of women and 1% of men continue to experience it into adulthood.
Managing and Treating Acne
Acne can’t be cured but can be controlled with effective treatment. Here are some self-help tips to manage symptoms:
- Wash gently: Cleanse affected areas no more than twice a day with mild soap and lukewarm water.
- Avoid squeezing: Do not try to “clean out” blackheads or pop spots, as this can worsen the condition and lead to scarring.
- Use non-comedogenic products: Opt for water-based cosmetics that are less likely to block pores.
- Completely remove makeup before bed.
- Stay active: While exercise doesn’t directly improve acne, it can boost mood and self-esteem. Be sure to shower immediately after sweating.
Topical treatments, creams, and gels are available at pharmacies. Treatment may take up to three months to show results. For severe cases, your pharmacist can recommend whether a visit to your GP is needed for stronger medication like antibiotics or prescription creams.
When to Seek Professional Advice
If your acne includes nodules or cysts or if it affects your chest and back, see your GP to avoid permanent scarring. For immediate advice, visit your local Pharmacy First Scotland service.
Further Support
Organisations like Changing Faces provide support and counseling for people affected by visible skin conditions.
Causes of Acne
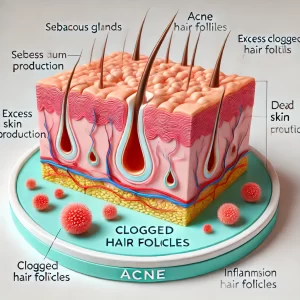
Acne occurs when small openings in the skin known as hair follicles become blocked. Sebaceous glands, located near the skin’s surface and connected to hair follicles, produce an oily substance called sebum to lubricate hair and skin. In people with acne, these glands produce excessive sebum. The excess sebum combines with dead skin cells to form a plug within the follicle, leading to:
- Whiteheads: When the plugged follicle bulges outwards near the skin’s surface.
- Blackheads: When the plugged follicle is open and exposed, creating a darkened surface due to pigmentation.
Harmless skin bacteria can also infect the blocked follicles, resulting in papules, pustules, nodules, or cysts.
Role of Hormones (Testosterone)
Teenage acne is often triggered by rising levels of testosterone during puberty. This hormone plays a crucial role in the development of male sexual characteristics and muscle and bone strength in females. Increased testosterone makes the sebaceous glands more sensitive, leading to higher sebum production.
Genetic Factors and Acne
Family history plays a significant role in acne development. If your parents had acne, there is a higher likelihood that you will also experience it. Studies suggest that having parents with adult acne increases the risk of developing more severe or persistent acne yourself.
Acne in Women
Over 80% of adult acne cases occur in women, often linked to hormonal changes, including:
- Menstrual cycle: Many women experience flare-ups just before their period.
- Pregnancy: Acne is common during the first three months of pregnancy.
- Polycystic ovary syndrome (PCOS): This condition can cause acne, weight gain, and ovarian cysts.
Other Acne Triggers
Additional factors that may trigger or worsen acne include:
- Cosmetic products: While rare, certain products can contribute to acne unless they are labeled as non-comedogenic.
- Medications: Steroid medications, lithium (for depression and bipolar disorder), and some anti-epileptic drugs can trigger acne.
- Pressure on the skin: Regularly wearing items like headbands or backpacks.
- Smoking: This can contribute to acne, especially in older individuals.
Common Acne Myths
Despite being widespread, acne is often misunderstood. Here are some common myths:
“Acne is caused by a poor diet”
Research hasn’t identified specific foods that cause acne. A balanced diet is beneficial for overall health but does not directly cause or cure acne.
“Acne is due to dirty skin and poor hygiene”
Acne is triggered by biological processes beneath the skin, not by surface dirt. Washing more than twice daily may irritate the skin.
“Squeezing spots helps remove acne”
Squeezing spots can worsen symptoms and lead to scarring.
“Sexual activity affects acne”
Sexual activity, including masturbation, does not influence acne.
“Sun exposure improves acne”
No evidence supports sunbathing, sunbeds, or sunlamps as acne remedies. Some acne treatments increase sensitivity to light, making sun exposure risky and potentially harmful.
“Acne is contagious”
Acne cannot be passed from one person to another.
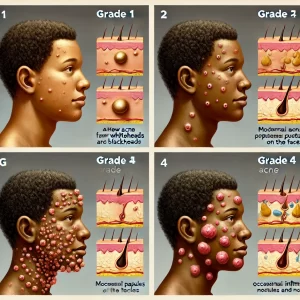
Diagnosing Acne: Understanding Severity and Hormonal Factors
How is Acne Diagnosed?
Acne diagnosis typically involves a physical examination of the skin. A pharmacist or healthcare professional will inspect areas like the face, chest, and back to identify different types of spots, including blackheads, whiteheads, papules, pustules, and nodules. The number, size, and severity of spots help determine the acne grade, which plays a key role in planning effective treatment.
Acne Severity Grading System
Acne severity is often classified into four grades:
- Grade 1 (Mild):
Predominantly whiteheads and blackheads with a few papules and pustules. - Grade 2 (Moderate):
Multiple papules and pustules, primarily confined to the face. - Grade 3 (Moderately Severe):
A large number of papules and pustules, with occasional inflamed nodules. Acne may also appear on the back and chest. - Grade 4 (Severe):
Characterized by numerous large, painful pustules and nodules that can affect the back, chest, and neck.
Hormonal Acne in Women
When acne suddenly develops in adult women, it may indicate a hormonal imbalance, especially if accompanied by other symptoms like:
- Excessive body hair (hirsutism).
- Irregular or light periods.
The most common cause of hormonal imbalances in women is polycystic ovary syndrome (PCOS), which can be diagnosed through ultrasound scans and blood tests.
Treating Acne: Options and Recommendations
Overview of Acne Treatment
Treatment for acne depends on its severity and may take several months before noticeable improvements occur. Here’s a comprehensive guide to available treatment options:
Over-the-Counter Treatments
For mild acne with a few blackheads, whiteheads, or spots, you can start with over-the-counter topical treatments containing benzoyl peroxide, which helps reduce bacteria and inflammation.

Prescription Treatments from Your GP
If your acne is more severe or if over-the-counter treatments haven’t worked, visit your GP. Prescription options include:
- Topical retinoids: These exfoliate dead skin cells to prevent clogged pores.
- Topical antibiotics: Reduce bacteria on the skin.
- Azelaic acid: An alternative to benzoyl peroxide and retinoids.
- Antibiotic tablets: For more severe acne.
- Combined oral contraceptive pill: For women with hormonal acne.
- Isotretinoin tablets: Reserved for severe acne.
Severe Acne Management
Your GP may refer you to a dermatologist if you have severe acne involving a large number of papules, pustules, or painful nodules on your chest, back, and face. Initial treatment often combines antibiotic tablets and topical treatments. If this approach doesn’t work, isotretinoin may be prescribed.
For women with acne, hormonal therapies such as the combined oral contraceptive pill can be effective. However, note that the progestogen-only pill or contraceptive implants may exacerbate acne.
Common Acne Treatments
1. Topical Treatments (Gels, Creams, and Lotions)
Benzoyl Peroxide
- Reduces bacteria, whiteheads, and blackheads.
- Use sparingly, as it can irritate and dry the skin.
- Avoid sunlight exposure and wear sunscreen.
Topical Retinoids
- Exfoliate dead skin cells.
- Apply once daily before bed.
- Not suitable for pregnancy due to potential birth defects.
Topical Antibiotics
- Kill skin bacteria causing acne.
- Use for 6 to 8 weeks to prevent bacterial resistance.
Azelaic Acid
- Effective for sensitive skin and less irritating.
- Usually applied once or twice daily.
2. Antibiotic Tablets
Oral antibiotics are often combined with topical treatments for moderate to severe acne. Tetracyclines are common, except for pregnant or breastfeeding women who are prescribed erythromycin. Treatment duration is typically 4 to 6 months.
3. Hormonal Therapies
Effective for women with acne related to hormonal changes, the combined oral contraceptive pill can help, though it may take up to a year for full benefits. Co-cyprindiol may also be prescribed for severe cases.
Co-cyprindiol Risks
- Slightly increased risk of breast cancer and blood clots.
- Not suitable during pregnancy.
4. Isotretinoin (Severe Cases)
Isotretinoin normalizes sebum production, prevents clogged pores, and reduces bacteria. Due to potential severe side effects, it is only prescribed by a dermatologist. Women of childbearing age must use contraception and have regular pregnancy tests during treatment.
Side Effects
- Common: Dry skin, cracked lips, irritation.
- Rare: Liver or pancreas inflammation, mood changes.
Non-Pharmaceutical Treatments
Alternative treatments include:
- Comedone extractor: Clears blackheads and whiteheads.
- Chemical peels: Removes the top layer of skin.
- Photodynamic therapy: Light-based treatment to improve symptoms.
However, these methods may have limited effectiveness and are not routinely recommended.
Important Tips for Acne Treatment
- Be patient; many treatments take 2-3 months to show results.
- Always follow your healthcare provider’s recommendations and persist with the treatment even if improvement isn’t immediate.
Complications of Acne: Scarring and Emotional Impact
Acne Scarring
Acne scarring can occur as a result of any type of acne spot, but it’s more common when nodules and cysts burst and damage surrounding skin. Picking or squeezing spots increases the risk of scarring.

Types of Acne Scars:
- Ice Pick Scars: Small, deep holes that look like punctures from a sharp object.
- Rolling Scars: Caused by bands of scar tissue under the skin, giving it a rolling, uneven appearance.
- Boxcar Scars: Round or oval depressions, or craters, in the skin.
Treating Acne Scarring
Acne scar treatments are usually considered cosmetic procedures and may not be covered by the NHS unless it is shown to cause severe psychological distress. Private treatments are available but can range widely in cost, from £500 to over £10,000.
It’s important to have realistic expectations—treatment can improve the appearance of scars but may not remove them completely. Most people experience a 50-75% improvement.
Common Treatments:
- Dermabrasion: Removes the top layer of skin using lasers or a wire brush, with several months of healing required.
- Laser Treatment:
- Ablative: Removes skin around the scar to create a smooth surface.
- Non-ablative: Stimulates collagen growth to repair damaged skin.
- Punch Techniques: Treats ice pick and boxcar scars through methods like punch excision, punch elevation, and punch grafting.
- Subcision: A surgical treatment for rolling scars that separates the upper skin layer from underlying scar tissue.
Emotional Impact: Depression and Anxiety
Acne can lead to feelings of anxiety, stress, and depression, potentially causing social withdrawal. If you or someone you know has been feeling down, hopeless, or uninterested in daily activities over the past month, consider speaking with a GP.
Treatment Options for Depression:
- Talking therapies like Cognitive Behavioural Therapy (CBT).
- Antidepressants such as Selective Serotonin Reuptake Inhibitors (SSRIs).