Table of Contents
ToggleHypertension Symptoms
Below is a comprehensive, structured report on hypertension symptoms. This report reviews the clinical manifestations of hypertension alongside its historical background, causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, and emerging research. It is designed to serve both the general public and medical professionals.
1. Overview
What are Hypertension Symptoms?
Hypertension symptoms refer to the clinical signs and manifestations associated with high blood pressure. Often dubbed the “silent killer,” hypertension may remain asymptomatic for years before causing severe health complications.
Definition and Affected Body Parts/Organs
- Definition: Hypertension is a chronic medical condition characterized by persistently elevated arterial blood pressure. The symptoms result primarily from the strain on blood vessels and target organs due to prolonged high pressure.
- Affected Organs:
- Cardiovascular System: Heart, arteries, and blood vessels.
- Kidneys: Can lead to chronic kidney disease.
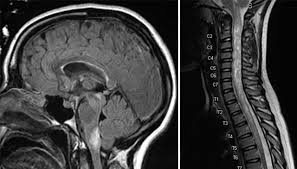
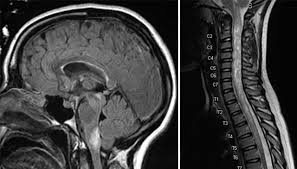
- Brain: Increases the risk of stroke.
- Eyes: May cause retinopathy.
Prevalence and Significance
- Hypertension affects over 1.3 billion people globally, with many unaware of their condition due to its often asymptomatic nature.
- Its significance is underscored by its role as a major risk factor for heart disease, stroke, and kidney failure.
2. History & Discoveries
When and How Was It First Identified?
- Early descriptions of high blood pressure date back to the 19th century when physicians began correlating elevated arterial tension with cardiovascular events.
- Initial blood pressure measurements using mercury sphygmomanometers allowed for objective diagnosis, evolving clinical practice.
Who Discovered It?
- No single individual “discovered” hypertension; rather, it emerged from cumulative clinical observations. Key contributors include early physiologists who refined blood pressure measurement techniques.
Major Discoveries and Breakthroughs
- The introduction of the sphygmomanometer in the late 1800s revolutionized diagnosis.
- Identification of risk factors such as salt intake, obesity, and stress in the 20th century contributed to targeted treatment.
- Development of antihypertensive medications (ACE inhibitors, beta-blockers, diuretics) transformed management and outcomes.
Evolution of Medical Understanding Over Time
- Initially considered a disease of older age, hypertension is now recognized across age groups.
- Modern medicine emphasizes early detection and treatment to prevent end-organ damage.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Often asymptomatic or may include subtle signs such as headaches, lightheadedness, or occasional dizziness.
- Some patients report fatigue or short episodes of blurred vision.
- Advanced-Stage Symptoms:
- When complications occur, symptoms may include chest pain, severe headaches, confusion, and visual disturbances.
- In cases with end-organ damage, patients might experience symptoms related to heart failure, kidney dysfunction, or stroke.
Common vs. Rare Symptoms
- Common: Most individuals experience no overt symptoms until blood pressure reaches very high levels; when symptoms are present, headache and dizziness are among the most frequent.
- Rare: Symptoms like epistaxis (nosebleeds), palpitations, or even anxiety episodes may occur but are not reliable indicators of hypertension.
How Symptoms Progress Over Time
- Hypertension is often called “silent” because most early stages are asymptomatic.
- As blood pressure remains uncontrolled, the cumulative stress on vessels and organs leads to noticeable clinical signs and complications.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- Elevated blood pressure can result from increased cardiac output or heightened systemic vascular resistance.
- Environmental Causes:
- High salt intake, sedentary lifestyle, chronic stress, and excessive alcohol consumption.
- Exposure to environmental pollutants has also been linked to vascular inflammation.
Genetic and Hereditary Factors
- A family history of hypertension greatly increases one’s risk.
- Genetic predispositions affect salt sensitivity and vascular responsiveness, influencing blood pressure regulation.
Known Triggers or Exposure Risks
- Triggers include dietary factors (high sodium), stress, obesity, and physical inactivity.
- Some medications (e.g., NSAIDs, corticosteroids) can elevate blood pressure.
5. Risk Factors
Who Is Most at Risk?
- Age: Risk increases with age.
- Gender: While both men and women are affected, younger men are at greater risk, whereas postmenopausal women experience a rise in incidence.
- Occupation & Lifestyle: High-stress jobs, sedentary behavior, and poor dietary habits contribute significantly.
Environmental, Occupational, and Genetic Influences
- Environmental stressors, urbanization, and exposure to pollution contribute to higher rates of hypertension.
- Occupational factors—especially jobs involving high stress—can predispose individuals to elevated blood pressure.
Impact of Pre-existing Conditions
- Conditions such as diabetes, obesity, and chronic kidney disease exacerbate hypertension risk and severity.
6. Complications
What Complications Can Arise from Hypertension?
- Cardiovascular Complications: Heart attack, heart failure, and left ventricular hypertrophy.
- Cerebrovascular Complications: Stroke and transient ischemic attacks (TIAs).
- Renal Complications: Chronic kidney disease and eventual kidney failure.
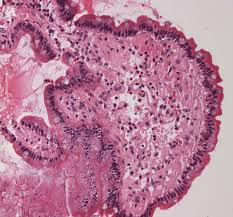
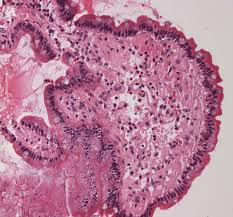
- Ophthalmic Complications: Retinopathy, which can lead to vision loss.
Long-Term Impact on Organs and Overall Health
- Persistent high blood pressure leads to arterial damage, reducing blood flow to vital organs.
- Over time, these complications significantly impair quality of life and contribute to premature death.
Potential Disability or Fatality Rates
- Hypertension is a major contributor to global mortality, with cardiovascular and cerebrovascular events being the leading causes of death.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation: Routine blood pressure measurements in both clinical and home settings.
- Ambulatory Blood Pressure Monitoring (ABPM): Provides 24-hour blood pressure readings to assess variability.
Medical Tests
- Blood Tests: Evaluate cholesterol, kidney function, and electrolyte levels.
- Electrocardiogram (ECG): To check for cardiac changes associated with long-standing hypertension.
- Imaging: Echocardiograms may be used to detect heart damage due to high blood pressure.
Early Detection Methods and Their Effectiveness
- Regular screening is key—many guidelines recommend yearly measurements, especially in individuals over 40 or with risk factors.
- Home blood pressure monitors have improved early detection and ongoing management.
8. Treatment Options
Standard Treatment Protocols
- Lifestyle Modifications:
- Dietary changes (e.g., reduced sodium intake, DASH diet).
- Increased physical activity, weight management, and stress reduction.
- Medications:
- ACE Inhibitors and ARBs: To relax blood vessels.
- Calcium Channel Blockers and Diuretics: Common first-line therapies.
- Beta-Blockers: Often used in patients with additional cardiovascular conditions.
Medications, Surgeries, and Therapies
- While no surgical cure exists for hypertension, procedures such as renal denervation are under investigation for resistant cases.
- Combination therapy is common when a single medication is insufficient.
Emerging Treatments and Clinical Trials
- Research continues on novel antihypertensive agents that target different molecular pathways.
- Ongoing clinical trials are exploring gene therapy and personalized medicine approaches for better management of hypertension.
9. Prevention & Precautionary Measures
How Can Hypertension Be Prevented?
- Primary Prevention:
- Adopting a healthy lifestyle including a balanced diet, regular exercise, and stress management.
- Avoiding excessive alcohol and tobacco use.
- Lifestyle Changes and Environmental Precautions:
- Regular monitoring and early intervention in individuals with predisposing factors.
- Preventive Screenings and Vaccinations:
- Routine blood pressure checks; although vaccines do not prevent hypertension, immunizations (like influenza vaccines) can reduce complications in hypertensive patients.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Hypertension affects approximately 1.3 billion people worldwide, with substantial variations between regions due to lifestyle, economic factors, and healthcare access.
Mortality and Survival Rates
- Hypertension is a leading contributor to cardiovascular mortality globally. Effective management has improved survival, yet untreated high blood pressure remains a major public health concern.
Country-Wise Comparison and Trends
- Developed nations benefit from robust screening programs, resulting in earlier diagnosis and treatment.
- In developing countries, rising urbanization and dietary changes have led to increasing prevalence.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Innovative Pharmacotherapy:
- New classes of drugs targeting inflammatory pathways and endothelial function.
- Personalized Medicine:
- Genetic and biomarker research is paving the way for individualized treatment plans.
- Technological Advances:
- Improvements in digital health and remote monitoring are enhancing blood pressure management.
Ongoing Studies and Future Medical Possibilities
- Clinical trials continue to investigate the efficacy of combination therapies and novel treatment targets.
- Research into non-pharmacological interventions, such as device-based therapies like renal denervation, is ongoing.
Potential Cures or Innovative Therapies Under Development
- While a cure for hypertension remains elusive, advances in lifestyle interventions, medication adherence strategies, and emerging therapies promise to further reduce complications and improve patient outcomes.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Hypertension Symptoms
- Silent Nature:
- Many individuals remain unaware of their high blood pressure until complications arise, which is why hypertension is often labeled the “silent killer.”
- Myths vs. Medical Facts:
- A common misconception is that hypertension always causes noticeable symptoms; however, most patients are asymptomatic until end-organ damage occurs.
- Impact on Specific Populations:
- Ethnic minorities and economically disadvantaged populations often have higher rates of uncontrolled hypertension due to barriers in access to healthcare.
- Historical Curiosities:
- The evolution of blood pressure measurement has been pivotal; early instruments were rudimentary compared to today’s digital and ambulatory monitors that allow precise management.
References
- Mayo Clinic. (2023). High Blood Pressure (Hypertension) Overview.
- National Institutes of Health. (2022). Hypertension: Advances in Understanding and Management.
- Johns Hopkins Medicine. (2023). Hypertension: Symptoms, Diagnosis, and Treatment.
- UpToDate. (2023). Diagnosis and Management of Hypertension.
- American Heart Association. (2023). Risk Factors and Impact of Hypertension.
- Global Health Statistics. (2023). Epidemiology of Hypertension Worldwide.
- World Health Organization. (2023). Preventive Strategies for Noncommunicable Diseases.
- Nature Reviews. (2023). Emerging Therapies in Cardiovascular Medicine.
- ClinicalTrials.gov. (2023). Ongoing Research in Hypertension Management.
- BMJ. (2023). Debunking Myths in Hypertension Management.
This detailed report on hypertension symptoms offers an in-depth overview of its definition, historical background, clinical presentation, underlying causes, risk factors, complications, diagnostic and treatment approaches, and future research directions. Early detection and proactive management are critical for reducing the long-term impact of hypertension on individual and public health.
Recent Posts
- Transverse Myelitis – Everything you need to know
- O Level Exam Dates 2025
- NMO (Neuromyelitis Optica) – Everything you need to know
- GCSE Exam Dates & Timetable 2025
- Mastocytosis – Everything you need to know
- IGCSE Exam Dates & Timetable 2025
- 2025 IB Examination Schedule
- Amyloid – Everything you need to know
- Types of Asthma – Everything you need to know
- Dengue – Everything you need to know
- Rotavirus – Everything you need to know
- 2025 AP Exam Schedule
- Vaginitis Treatments – Everything you need to know
- Arthritis in the Fingers – Everything you need to know
- High Cholesterol Foods – Everything you need to know
Choose Topic
- ACT (17)
- AP (20)
- AP Art and Design (5)
- AP Physics 1 (1)
- AQA (5)
- Artificial intelligence (AI) (2)
- Banking and Finance (6)
- Biology (13)
- Business Ideas (68)
- Calculator (72)
- ChatGPT (1)
- Chemistry (3)
- Colleges Rankings (48)
- Computer Science (4)
- Conversion Tools (136)
- Cosmetic Procedures (50)
- Cryptocurrency (49)
- Digital SAT (3)
- Disease (225)
- Edexcel (4)
- English (1)
- Environmental Science (2)
- Etiology (7)
- Exam Updates (6)
- Finance (129)
- Fitness & Wellness (164)
- Free Learning Resources (211)
- GCSE (1)
- General Guides (40)
- Health (107)
- History and Social Sciences (152)
- IB (8)
- IGCSE (2)
- Image Converters (3)
- IMF (10)
- Math (43)
- Mental Health (58)
- News (9)
- OCR (3)
- Past Papers (463)
- Physics (5)
- Research Study (6)
- SAT (39)
- Schools (3)
- Sciences (1)
- Short Notes (5)
- Study Guides (28)
- Syllabus (19)
- Tools (1)
- Tutoring (1)
- What is? (312)
Recent Comments

Transverse Myelitis - Everything you need to know
NMO (Neuromyelitis Optica) - Everything you need to know

Mastocytosis - Everything you need to know
Amyloid - Everything you need to know

Transverse Myelitis - Everything you need to know
NMO (Neuromyelitis Optica) - Everything you need to know

Mastocytosis - Everything you need to know