Hepatitis D
Below is a comprehensive, structured report on Hepatitis D (also known as Delta Hepatitis) that covers its definition, history, clinical features, causes, risk factors, complications, diagnosis, treatment options, prevention strategies, global epidemiology, recent research, and interesting insights. This report is intended for both medical professionals and the general public.
1. Overview
What is Hepatitis D?
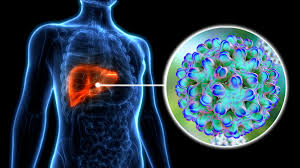
Hepatitis D is a liver infection caused by the hepatitis D virus (HDV), a unique defective RNA virus that requires the presence of hepatitis B virus (HBV) for its replication. HDV can lead to a more severe course of liver disease compared with HBV infection alone.
Definition & Affected Body Parts/Organs
- Definition:
- Hepatitis D is defined as an infection of the liver that occurs only in individuals who are also infected with HBV, since HDV depends on HBV surface antigen (HBsAg) for its viral assembly and infectivity.
- Affected Organs:
- Liver: The primary organ affected, where HDV causes inflammation, necrosis, and fibrosis, leading to cirrhosis and potentially hepatocellular carcinoma.
Prevalence and Significance
- Prevalence:
- It is estimated that 5–20 million people worldwide are co-infected with HBV and HDV. Prevalence is highest in parts of Africa, the Middle East, Eastern Europe, and the Amazon basin.
- Significance:
- Hepatitis D is clinically significant because co-infection with HDV accelerates the progression of liver disease, increases the risk of cirrhosis and liver cancer, and is associated with higher mortality rates compared with HBV infection alone.
2. History & Discoveries
When and How Was Hepatitis D First Identified?
- Early Recognition:
- The existence of a delta agent was first postulated in the 1970s when clinicians observed that some patients with HBV developed more severe liver disease.
- Modern Identification:
- In 1977, the delta antigen (HDAg) was discovered, and the hepatitis D virus was subsequently identified as the causative agent.
Who Discovered It?
- Key Contributors:
- The work of Dr. Mario Rizzetto and colleagues in Italy was central to the discovery of the delta antigen and the identification of HDV as a distinct pathogen.
Major Discoveries and Breakthroughs
- Delta Antigen Discovery: The identification of the delta antigen confirmed the existence of a separate viral entity associated with HBV.
- Molecular Characterization: Subsequent genetic sequencing of HDV revealed its unique RNA genome and dependence on HBV for replication.
- Clinical Impact: Research established that HDV co-infection leads to more aggressive liver disease, prompting changes in screening and management practices.
Evolution of Medical Understanding Over Time
The understanding of hepatitis D has evolved from initial observations of severe liver disease in HBV patients to detailed molecular insights into HDV’s structure, replication, and its synergistic effects with HBV. This evolution has informed improved diagnostic methods and the development of targeted treatment strategies.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Fatigue, weakness, loss of appetite, nausea, and mild jaundice.
- Some patients may be asymptomatic during the early phase.
- Advanced-Stage Symptoms:
- Worsening jaundice, abdominal pain, dark urine, and pale stools.
- Signs of advanced liver disease, such as ascites, confusion (hepatic encephalopathy), and easy bruising.
- Rapid progression to cirrhosis in many co-infected patients.
Common vs. Rare Symptoms
- Common:
- General malaise, jaundice, and gastrointestinal discomfort.
- Rare:
- Acute liver failure may occur in some cases, particularly with superinfection (HDV infection in a chronic HBV carrier), though it is less common.
How Symptoms Progress Over Time
In many patients, symptoms begin subtly and progress as the virus accelerates liver damage. Co-infection with HBV and HDV often leads to a more rapid progression from chronic hepatitis to cirrhosis and liver failure compared with HBV infection alone.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- Hepatitis D is caused by infection with the hepatitis D virus, which requires the presence of HBV for its life cycle. It can occur as a co-infection (simultaneous infection with HBV and HDV) or as a superinfection (HDV infecting an individual with chronic HBV).
- Environmental Factors:
- Transmission is primarily via blood and bodily fluids, often in settings with inadequate infection control practices.
Genetic and Hereditary Factors
- Genetic Factors:
- There are no direct genetic causes of HDV infection. However, genetic predisposition to severe liver disease in HBV carriers may influence outcomes in those co-infected with HDV.
Any Known Triggers or Exposure Risks
- Triggers:
- Exposure to infected blood through unsafe injections, blood transfusions, or needle sharing.
- Exposure Risks:
- Living in or traveling to areas with high HBV/HDV prevalence.
- Occupational exposure in healthcare settings without proper infection control measures.
5. Risk Factors
Who Is Most at Risk?
- Age:
- Individuals of all ages are at risk, but the consequences are particularly severe in adults.
- Gender:
- Both genders are affected equally; however, outcomes may vary with individual health status.
- Occupation & Lifestyle:
- Healthcare workers and individuals with high-risk behaviors (e.g., intravenous drug use) are at increased risk.
- Pre-existing Conditions:
- Chronic HBV infection is a prerequisite for HDV infection. Individuals with pre-existing liver disease are at higher risk for severe outcomes.
Environmental, Occupational, and Genetic Factors
- Environmental:
- Regions with high HBV prevalence and inadequate healthcare resources.
- Occupational:
- Healthcare professionals and laboratory workers are at risk if infection control is insufficient.
- Genetic:
- Genetic predisposition does not cause HDV infection, though host genetic factors may influence disease severity.
Impact of Pre-existing Conditions
Pre-existing chronic HBV infection is necessary for HDV infection. Additionally, any condition that weakens the immune system can worsen the prognosis in co-infected patients.
6. Complications
What Complications Can Arise from Hepatitis D?
- Liver Disease:
- Accelerated progression to cirrhosis.
- Increased risk of hepatocellular carcinoma (liver cancer).
- Acute liver failure, particularly in superinfections.
- Systemic Complications:
- Portal hypertension leading to variceal bleeding.
- Hepatic encephalopathy due to advanced liver dysfunction.
Long-Term Impact on Organs and Overall Health
Chronic co-infection with HDV and HBV can lead to rapid liver scarring, decreased liver function, and systemic complications that significantly impact overall health and quality of life.
Potential Disability or Fatality Rates
- The combination of HBV and HDV is associated with higher mortality rates compared with HBV alone.
- Many patients progress to end-stage liver disease requiring transplantation, and the overall case-fatality rate is high without timely intervention.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
- Detailed patient history focusing on risk factors (e.g., HBV infection, exposure history) and clinical signs of liver disease.
- Serologic Testing:
- Tests for hepatitis B surface antigen (HBsAg) to confirm HBV infection.
- Specific assays for HDV antibodies (IgM and IgG) and HDV RNA using PCR.
- Liver Function Tests:
- Blood tests to assess levels of liver enzymes, bilirubin, and albumin.
- Imaging:
- Ultrasound, CT, or MRI to evaluate liver structure and detect signs of cirrhosis.
- Biopsy:
- Liver biopsy may be performed to assess the extent of liver damage.
Medical Tests and Early Detection Methods
- Early Detection:
- Routine screening in patients known to be HBsAg-positive is crucial to detect HDV co-infection early.
- Effectiveness:
- Combining serological tests with molecular assays (PCR) is highly effective in confirming diagnosis and guiding treatment decisions.
8. Treatment Options
Standard Treatment Protocols
- Antiviral Therapy:
- Treatment options are limited; pegylated interferon-alpha has been used to treat HDV infection, though responses vary.
- Management of Liver Disease:
- Supportive care for cirrhosis, including management of complications such as ascites and portal hypertension.
- Liver Transplantation:
- In cases of advanced liver failure, transplantation may be necessary.
- Emerging Treatments:
- New agents targeting viral replication and host immune responses are under investigation in clinical trials.
Medications, Surgeries, and Therapies
- Medications: Interferon-based therapies are currently the main treatment option.
- Emerging Therapies:
- Ongoing clinical trials are exploring novel antiviral agents and immunomodulatory therapies aimed at improving response rates and reducing liver damage.
9. Prevention & Precautionary Measures
How Can Hepatitis D Be Prevented?
- Primary Prevention:
- Since HDV requires HBV for replication, vaccination against hepatitis B is the most effective preventive measure.
- Screening and Early Detection:
- Routine screening for HDV in individuals with chronic HBV infection.
- Infection Control:
- Implementing proper infection control practices in healthcare settings to prevent blood-borne transmission.
- Lifestyle and Environmental Precautions:
- Avoiding behaviors that increase the risk of blood-borne infections (e.g., needle sharing, unsafe sex).
Vaccines (if Applicable) or Preventive Screenings
- Vaccination:
- The hepatitis B vaccine indirectly prevents HDV infection by preventing HBV.
- Preventive Screenings:
- Regular screening of HBV carriers for HDV co-infection is recommended in endemic areas.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Incidence:
- HDV co-infection occurs in a significant proportion of HBV carriers, with estimates varying widely by region.
- Prevalence:
- High prevalence in parts of Africa, the Middle East, and Eastern Europe. Globally, millions are affected by chronic HBV, and among these, up to 10–20% may be co-infected with HDV.
Mortality and Survival Rates
- Mortality:
- Co-infection with HDV increases the risk of rapid progression to cirrhosis and liver cancer, leading to higher mortality rates compared with HBV alone.
- Survival:
- With early detection and management, survival can be improved, but advanced liver disease remains a significant challenge.
Country-Wise Comparison and Trends
- Endemic Regions: Higher rates of HDV are found in countries with high HBV prevalence and limited vaccination programs.
- Developed Countries: Better vaccination coverage has led to lower rates of HDV co-infection among HBV carriers.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Novel Antiviral Agents:
- Investigational therapies targeting HDV replication and host immune modulation are under clinical trials.
- Immunomodulatory Therapies:
- New approaches using biologics and interferon alternatives are being studied.
- Vaccine Development:
- Research into therapeutic vaccines specifically targeting HDV is ongoing.
- Genomic Studies:
- Advances in genomics and molecular biology are improving the understanding of disease progression and potential treatment targets.
Ongoing Studies and Future Medical Possibilities
- Clinical Trials: Several trials are evaluating new drug candidates and combination therapies for HDV.
- Future Possibilities:
- Advances in personalized medicine and targeted therapies hold promise for better outcomes.
- Integration of global vaccination programs may further reduce the burden of HDV.
Potential Cures or Innovative Therapies Under Development
- While a definitive cure for hepatitis D is not yet available, emerging treatments and improved management strategies continue to evolve, offering hope for reducing liver-related morbidity and mortality.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Hepatitis D
- Unique Viral Nature:
- HDV is considered the smallest virus and is unique because it is a “defective” virus that requires HBV for its life cycle.
- Impact on Liver Disease:
- Co-infection with HDV leads to a more aggressive course of liver disease compared with HBV infection alone.
- Global Health Impact:
- Despite its relatively low prevalence compared to HBV, HDV significantly increases the burden of liver disease in endemic regions.
Myths and Misconceptions vs. Medical Facts
- Myth: HDV can infect people without hepatitis B.
Fact: HDV requires HBV co-infection to replicate. - Myth: Hepatitis D is common in all HBV patients.
Fact: The prevalence of HDV co-infection varies widely by region, depending largely on local HBV epidemiology and vaccination coverage. - Myth: There is no hope for those with HDV.
Fact: Advances in antiviral therapies and global HBV vaccination programs are steadily improving outcomes for HDV patients.
Impact on Specific Populations or Professions
- At-Risk Populations:
- Individuals with chronic HBV infection, particularly in regions with low vaccination rates.
- Healthcare Providers:
- Medical professionals involved in the management of viral hepatitis play a critical role in screening and treatment.
- Public Health Officials:
- Efforts to expand HBV vaccination have a direct impact on reducing HDV co-infection.
- Economic Impact:
- HDV contributes significantly to the healthcare burden in regions with high HBV prevalence, emphasizing the need for improved prevention and treatment strategies.
References
- World Health Organization (WHO). Hepatitis D Fact Sheet.
- Centers for Disease Control and Prevention (CDC). Hepatitis D Virus: Information and Prevention.
- Mayo Clinic. Hepatitis D: Symptoms, Causes, and Treatment.
This report integrates historical insights, clinical guidelines, and emerging research to provide a detailed and balanced overview of Hepatitis D. Emphasizing early detection, vaccination against hepatitis B, and innovative treatment strategies, the report aims to enhance understanding and improve outcomes for individuals affected by this challenging liver infection.