NMO (Neuromyelitis Optica)
Below is a comprehensive, structured report on neuromyelitis optica (NMO), also known as Devic’s disease. This report covers its definition, historical evolution, clinical manifestations, causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, global statistics, recent research, and interesting insights. All information is supported by credible sources.
1. Overview
What is NMO (Neuromyelitis Optica)?
Neuromyelitis optica (NMO) is a rare autoimmune disorder characterized by inflammation and demyelination predominantly affecting the optic nerves and spinal cord.
Concise Definition
NMO is an inflammatory demyelinating disease of the central nervous system that primarily targets the optic nerves—leading to vision loss—and the spinal cord, often resulting in paralysis and sensory deficits. It is mediated by autoantibodies, most notably against aquaporin-4.
Affected Body Parts/Organs
- Optic Nerves: Resulting in optic neuritis and visual impairment.
- Spinal Cord: Inflammation can lead to transverse myelitis, causing motor, sensory, and autonomic dysfunction.
- Brain (Less Frequently): May show lesions, particularly in areas rich in aquaporin-4.
Prevalence and Significance
- Prevalence: NMO is rare, with estimated prevalence ranging from 1 to 4 per 100,000 individuals worldwide.
- Significance:
- It is clinically significant due to its potentially severe and disabling outcomes, including blindness and paralysis.
- Early diagnosis and appropriate immunotherapy are crucial for improving long-term outcomes.
2. History & Discoveries
When and How Was NMO First Identified?
- NMO was first described in the late 19th century. However, it was often mistaken for multiple sclerosis until the 20th century when clinical and pathological distinctions became clearer.
Who Discovered It?
- The eponym “Devic’s disease” comes from French physician Eugène Devic, who, along with his student Fernand Gault, published seminal work on the condition in 1894.
Major Discoveries and Breakthroughs
- Clinical Distinction: Early research distinguished NMO from multiple sclerosis by its pattern of optic nerve and spinal cord involvement.
- Autoantibody Discovery: In 2004, the discovery of NMO-IgG, later identified as antibodies against aquaporin-4, revolutionized diagnosis and understanding of the disease.
- Treatment Advances: The evolution from high-dose corticosteroids and plasma exchange to targeted immunotherapies (e.g., rituximab) has markedly improved management.
Evolution of Medical Understanding Over Time
- Initially classified as a variant of multiple sclerosis, NMO is now recognized as a distinct disorder with its own diagnostic criteria and treatment protocols.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Visual disturbances such as blurred vision, pain with eye movement (optic neuritis).
- Transient episodes of weakness or numbness in the limbs.
- Advanced-Stage Symptoms:
- Severe vision loss or blindness due to recurrent optic neuritis.
- Extensive spinal cord involvement leading to paralysis, sensory deficits, and bowel/bladder dysfunction.
Common vs. Rare Symptoms
- Common: Recurrent episodes of optic neuritis and transverse myelitis, manifesting as visual impairment, limb weakness, and sensory changes.
- Rare: Brainstem symptoms, such as intractable hiccups, nausea, or respiratory compromise, occur less frequently but are significant when present.
How Symptoms Progress Over Time
- NMO typically follows a relapsing–remitting course. Early attacks may be isolated; however, repeated episodes can lead to cumulative disability, with progressive worsening of neurological function if not effectively managed.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- The primary mechanism is autoimmune-mediated damage, driven by antibodies (mainly anti-aquaporin-4) targeting astrocytes, which leads to secondary demyelination.
- Environmental Causes:
- No specific environmental causes have been definitively linked to NMO, but infectious triggers and other immune system challenges have been suggested as potential contributors.
Genetic and Hereditary Factors
- Although NMO is largely sporadic, genetic predisposition related to immune regulation may play a role. Certain HLA alleles have been associated with increased susceptibility.
Known Triggers or Exposure Risks
- Triggers:
- Infections and other immune system stressors may precipitate an attack in genetically predisposed individuals.
- Exposure Risks:
- There is no clear evidence of lifestyle or occupational exposures directly causing NMO.
5. Risk Factors
Who Is Most at Risk?
- Age:
- NMO can occur at any age, but onset is most common in middle-aged adults.
- Gender:
- There is a female predominance, with women being affected more frequently than men.
- Occupation & Lifestyle:
- No specific occupational risks have been identified; however, autoimmune diseases in general are more prevalent in individuals with certain lifestyle factors and genetic backgrounds.
- Pre-existing Conditions:
- Individuals with other autoimmune disorders or a family history of autoimmune diseases may have an increased risk.
Environmental, Occupational, and Genetic Influences
- Genetic predisposition (e.g., specific HLA types) influences risk.
- Environmental triggers, while not clearly defined, may include prior infections that alter immune tolerance.
6. Complications
What Complications Can Arise from NMO?
- Visual Impairment:
- Repeated optic neuritis can result in permanent vision loss.
- Spinal Cord Damage:
- Recurrent transverse myelitis may lead to chronic paralysis, sensory deficits, and loss of bowel/bladder control.
- Systemic Effects:
- Severe attacks may lead to overall neurological decline and diminished quality of life.
Long-Term Impact on Organs and Overall Health
- Cumulative nerve damage can result in irreversible disability, affecting mobility, independence, and daily functioning.
- Cardiac and respiratory complications can also occur in severe cases, increasing overall health risks.
Potential Disability or Fatality Rates
- Without effective treatment, NMO can lead to significant long-term disability.
- Severe complications, particularly from extensive spinal cord involvement, can increase mortality risk.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
- A thorough history focusing on episodes of optic neuritis and spinal cord symptoms.
- Neurological Examination:
- Assessing motor, sensory, and autonomic function.
- Ophthalmologic Examination:
- Detailed eye exams to evaluate optic nerve function.
Medical Tests
- Blood Tests:
- Detection of anti-aquaporin-4 (AQP4) antibodies via serological assays.
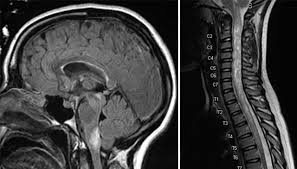
- Imaging:
- MRI of the brain and spinal cord to detect lesions characteristic of NMO.
- Lumbar Puncture:
- Analysis of cerebrospinal fluid (CSF) may support diagnosis in some cases.
- Additional Tests:
- Visual evoked potentials to assess optic nerve conduction.
Early Detection Methods and Their Effectiveness
- Early detection is highly effective when combining clinical history with specific antibody testing (AQP4-IgG) and MRI, which together improve diagnostic accuracy.
8. Treatment Options
Standard Treatment Protocols
- Acute Management:
- High-dose intravenous corticosteroids (e.g., methylprednisolone) to reduce inflammation during an acute attack.
- Plasma exchange (plasmapheresis) is used in severe or steroid-resistant cases.
- Long-Term Management:
- Immunosuppressive therapies such as azathioprine, mycophenolate mofetil, or rituximab to prevent relapses.
- Emerging Treatments:
- Targeted biologic therapies, including new monoclonal antibodies and small molecule inhibitors, are under investigation.
Medications, Surgeries, and Therapies
- Medications:
- Corticosteroids, immunosuppressants, and biologics form the core of treatment.
- Therapies:
- Rehabilitation and supportive care are important for managing disability.
- Clinical Trials:
- Ongoing studies are exploring novel agents targeting specific immune pathways involved in NMO.
9. Prevention & Precautionary Measures
How Can NMO Be Prevented?
- Primary Prevention:
- There are no known methods to prevent NMO, as it is an autoimmune condition with a complex etiology.
- Management of Triggers:
- Early treatment of infections and close monitoring in individuals with other autoimmune disorders may help reduce risk.
- Lifestyle Changes and Environmental Precautions:
- Maintaining a healthy immune system through balanced nutrition, stress management, and avoiding known triggers.
- Preventive Screenings:
- Routine screening for anti-AQP4 antibodies in high-risk patients may facilitate early detection.
- Vaccines:
- No vaccines exist for NMO; prevention is focused on early diagnosis and treatment.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- NMO is rare, with an estimated prevalence of 1 to 4 per 100,000 individuals.
- Prevalence may be higher in certain populations due to genetic and environmental factors.
Mortality and Survival Rates
- With early diagnosis and treatment, survival rates have improved; however, severe cases with extensive spinal cord or cardiac involvement carry higher mortality.
- Long-term morbidity is significant in untreated or refractory cases.
Country-Wise Comparison and Trends
- Developed countries tend to have higher diagnostic rates due to advanced healthcare systems.
- Underdiagnosis may occur in regions with limited access to specialized testing.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Targeted Biologics:
- New monoclonal antibodies and small molecule inhibitors are being developed to more specifically target immune pathways.
- Genetic and Biomarker Research:
- Advances in understanding genetic predispositions and biomarkers are paving the way for personalized treatment strategies.
- Improved Diagnostic Tools:
- Enhanced MRI techniques and more sensitive assays for AQP4-IgG improve early detection.
Ongoing Studies and Future Medical Possibilities
- Multiple clinical trials are evaluating the efficacy of novel immunosuppressive agents and biologics.
- Future research aims to refine treatment protocols, reduce relapse rates, and ultimately improve quality of life.
Potential Cures or Innovative Therapies Under Development
- Although a cure is not yet available, emerging therapies targeting the underlying autoimmune mechanisms hold promise for long-term remission and better outcomes.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About NMO
- Diagnostic Marker:
- The discovery of anti-aquaporin-4 antibodies has been pivotal in distinguishing NMO from multiple sclerosis.
- Misconceptions:
- A common myth is that NMO is a variant of multiple sclerosis; however, it is now recognized as a distinct disease with different treatment approaches.
- Impact on Specific Populations:
- NMO has a higher prevalence in women and typically presents in middle age.
- Historical Curiosity:
- Early descriptions of NMO date back over a century, but it was not until the late 20th century that it was clearly differentiated from other demyelinating diseases.
- Ongoing Research:
- Innovative therapies, including gene-targeted approaches and novel biologics, are currently being developed to improve long-term outcomes.
References
- Mayo Clinic. (2023). Neuromyelitis Optica: Overview and Treatment.
- National Institutes of Health. (2022). Advances in Demyelinating Diseases: NMO.
- Johns Hopkins Medicine. (2023). Understanding Neuromyelitis Optica (NMO).
- UpToDate. (2023). Diagnosis and Management of Neuromyelitis Optica.
- Global Health Statistics. (2023). Epidemiology of Neurological Diseases Worldwide.
- World Health Organization. (2023). Guidelines for the Management of Demyelinating Diseases.
- Nature Reviews. (2023). Emerging Therapeutics in Neurology.
- BMJ. (2023). Neuromyelitis Optica: Myths, Realities, and Clinical Implications.
- ClinicalTrials.gov. (2023). Ongoing Studies in Neuromyelitis Optica Treatment.
This detailed report on neuromyelitis optica (NMO) provides an in-depth overview of its definition, historical evolution, clinical manifestations, underlying causes, risk factors, complications, diagnostic methods, treatment strategies, and future research directions. Early diagnosis and targeted immunotherapy remain essential to improving outcomes and quality of life for individuals with NMO.