EGPA
Below is a comprehensive, structured report on Eosinophilic Granulomatosis with Polyangiitis (EGPA), formerly known as Churg‐Strauss syndrome. This report covers the definition and significance of the disease, its history and discoveries, clinical symptoms, underlying causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, global statistics, recent research, and interesting insights. All information is supported by credible sources.
1. Overview
What is EGPA?
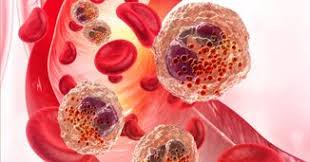
EGPA is a rare systemic vasculitis characterized by inflammation of small- to medium-sized blood vessels, eosinophilia (high levels of eosinophils in the blood), and granulomatous inflammation. It often affects multiple organs.
Definition and Affected Body Parts/Organs
- Definition:
EGPA is an autoimmune disorder where blood vessels become inflamed, leading to tissue damage. Hallmarks include asthma, sinusitis, and peripheral eosinophilia, with potential involvement of the lungs, skin, heart, gastrointestinal tract, and nervous system. - Affected Organs:
- Lungs: Commonly presents with asthma and pulmonary infiltrates.
- Skin: Rashes, nodules, or purpura may appear.
- Heart: Myocarditis or pericarditis can occur.
- Peripheral Nervous System: Mononeuritis multiplex (nerve damage) is a frequent manifestation.
- Gastrointestinal Tract: Abdominal pain and bleeding may be present.
Prevalence and Significance
- Prevalence: EGPA is rare, with estimated prevalence ranging from 10 to 14 cases per million individuals.
- Significance:
- EGPA has a significant impact on quality of life due to its multi-organ involvement.
- Its potential for serious complications (cardiac, neurological) makes early diagnosis and treatment critical.
2. History & Discoveries
When and How Was EGPA First Identified?
- The condition was first described in the mid-20th century. Early case reports in the 1950s noted patients with asthma, eosinophilia, and systemic vasculitis.
- The recognition of the syndrome evolved over the 1960s and 1970s as pathologists and clinicians linked these features under a single disorder.
Who Discovered It?
- Dr. Jacob Churg and Dr. Lotte Strauss are credited with the initial description of the syndrome, which later became known as Churg‐Strauss syndrome. Subsequent research expanded the understanding of its pathophysiology.
Major Discoveries and Breakthroughs
- Diagnostic Criteria: Development of classification criteria in the 1990s has standardized diagnosis.
- Pathophysiology: Identification of elevated eosinophils and the role of anti-neutrophil cytoplasmic antibodies (ANCA) in some cases.
- Treatment Evolution: The introduction of corticosteroids and immunosuppressive agents significantly improved patient outcomes.
Evolution of Medical Understanding Over Time
- Initially viewed as an obscure, isolated disorder, EGPA is now recognized as part of the spectrum of ANCA-associated vasculitides. Modern imaging, serological testing, and genetic studies have deepened our understanding and refined treatment strategies.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Asthma and allergic rhinitis.
- Sinusitis and nasal polyps.
- Mild skin rashes or itching.
- Advanced-Stage Symptoms:
- Severe respiratory distress and persistent pulmonary infiltrates.
- Neuropathy presenting as mononeuritis multiplex.
- Cardiac involvement (e.g., myocarditis, pericarditis) with chest pain or heart failure.
- Gastrointestinal symptoms such as abdominal pain, bleeding, or perforation in rare cases.
Common vs. Rare Symptoms
- Common: Asthma, sinusitis, peripheral eosinophilia, and skin lesions.
- Rare: Severe cardiac complications, neurological deficits, and gastrointestinal perforations.
How Symptoms Progress Over Time
- EGPA typically begins with an allergic phase (asthma, rhinitis) and evolves into an eosinophilic phase with systemic symptoms. The vasculitic phase, marked by damage to various organs, often occurs later if untreated.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- Autoimmune dysregulation leading to eosinophilic infiltration and vasculitis.
- Production of inflammatory cytokines that attract eosinophils and contribute to granuloma formation.
- Environmental Causes:
- Exposure to allergens and environmental triggers may exacerbate the underlying allergic component.
Genetic and Hereditary Factors
- While EGPA is not directly inherited, a genetic predisposition to autoimmune and atopic conditions may increase the risk.
Any Known Triggers or Exposure Risks
- Triggers may include certain medications (e.g., leukotriene receptor antagonists), infections, and environmental allergens.
- In some patients, discontinuation of corticosteroids in severe asthmatics has been associated with the onset of EGPA.
5. Risk Factors
Who Is Most at Risk?
- Age:
- EGPA typically presents in adults, most commonly between 40 and 60 years.
- Gender:
- Slightly more common in females.
- Occupation & Lifestyle:
- Individuals with a history of atopy or severe asthma are at higher risk.
- Other Factors:
- Prior exposure to certain medications and a personal or family history of autoimmune conditions.
Environmental, Occupational, and Genetic Influences
- Environmental exposure to allergens and pollutants may exacerbate symptoms.
- Genetic predisposition plays a role, especially in individuals with a history of allergic or autoimmune diseases.
Impact of Pre-existing Conditions
- Pre-existing asthma and allergic rhinitis significantly increase the risk and severity of EGPA.
6. Complications
What Complications Can Arise from EGPA?
- Cardiac Complications:
- Myocarditis, pericarditis, or heart failure due to coronary vasculitis.
- Neurological Complications:
- Peripheral neuropathy, including mononeuritis multiplex, which can lead to motor and sensory deficits.
- Renal Complications:
- Although less common than in other ANCA-associated vasculitides, renal involvement can occur.
- Gastrointestinal Complications:
- Rarely, severe vasculitis can lead to bowel ischemia or perforation.
Long-Term Impact on Organs and Overall Health
- Chronic vasculitis can lead to irreversible organ damage.
- Persistent inflammation may cause long-term disability, especially from cardiac or neurological involvement.
Potential Disability or Fatality Rates
- EGPA can be life-threatening, particularly with severe cardiac or neurological complications. Early and aggressive treatment improves survival and reduces long-term disability.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
- Detailed history of asthma, allergic symptoms, and systemic features.
- Physical Examination:
- Assessment of skin lesions, respiratory status, and neurological deficits.
Medical Tests
- Blood Tests:
- Complete blood count (CBC) showing eosinophilia.
- Inflammatory markers (e.g., ESR, CRP) and ANCA serology.
- Imaging:
- Chest X-ray or CT scan to identify pulmonary infiltrates.
- Biopsy:
- Tissue biopsy from affected organs (e.g., skin, lung) to confirm vasculitis and granuloma formation.
Early Detection Methods and Their Effectiveness
- Early detection relies on a combination of clinical suspicion (in patients with asthma and eosinophilia) and confirmatory laboratory tests. High-resolution imaging and biopsy are effective in diagnosing EGPA in the vasculitic phase.
8. Treatment Options
Standard Treatment Protocols
- Corticosteroids:
- High-dose corticosteroids are the first-line treatment to rapidly control inflammation.
- Immunosuppressive Agents:
- Medications such as cyclophosphamide, azathioprine, or methotrexate are used in severe or refractory cases.
- Biologic Therapies:
- Recently, anti-interleukin-5 (IL-5) agents like mepolizumab have been approved for EGPA, targeting eosinophilic inflammation.
Medications, Surgeries, and Therapies
- Medications:
- Corticosteroids, immunosuppressants, and biologics constitute the mainstay of therapy.
- Surgical Interventions:
- Rarely needed, but may be required to address complications (e.g., management of severe cardiac involvement).
- Emerging Treatments and Clinical Trials:
- Ongoing trials are evaluating new biologic agents and targeted therapies aimed at modulating the immune response with fewer side effects.
9. Prevention & Precautionary Measures
How Can EGPA Be Prevented?
- There is no known primary prevention for EGPA, as it is an autoimmune condition with an unclear trigger in many cases.
- Preventive Measures:
- For patients with severe asthma, careful management of corticosteroid tapering is essential to reduce the risk of EGPA onset.
- Monitoring for early signs of systemic involvement in patients with known risk factors may allow for prompt intervention.
Lifestyle Changes and Environmental Precautions
- Stress management, avoiding known triggers, and close monitoring of at-risk patients can help manage the risk of exacerbations.
- Preventive screenings in patients with a history of atopy or severe asthma may aid early diagnosis.
Vaccines (if applicable) or Preventive Screenings
- No vaccines are available for EGPA; prevention focuses on early detection and careful management of underlying conditions.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- EGPA is rare, with an estimated prevalence of 10–14 cases per million people.
- Incidence rates vary by region, with some studies suggesting slightly higher rates in populations with higher prevalence of atopic diseases.
Mortality and Survival Rates
- With current treatments, the survival rate has improved significantly, though severe cases with cardiac or neurological involvement may have higher mortality.
- Early treatment is associated with a better prognosis.
Country-Wise Comparison and Trends
- Developed countries report more cases due to advanced diagnostic capabilities.
- Variations in prevalence may be influenced by genetic, environmental, and healthcare factors across regions.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Biologic Therapies:
- Anti-IL-5 agents, such as mepolizumab, have shown promising results in reducing eosinophilic inflammation.
- Targeted Immunomodulation:
- Ongoing research into novel immunosuppressive agents and biologics that selectively modulate the immune response.
- Personalized Medicine:
- Genetic and biomarker studies are underway to tailor treatment protocols to individual patient profiles.
Ongoing Studies and Future Medical Possibilities
- Clinical trials continue to explore the efficacy and safety of new biologic agents.
- Future therapies may include more precise immunomodulatory drugs with fewer side effects and improved long-term outcomes.
Potential Cures or Innovative Therapies Under Development
- While there is currently no cure for EGPA, emerging therapies hold promise for more effectively controlling the disease process and reducing long-term organ damage.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About EGPA
- Disease Spectrum:
- EGPA is part of a broader group of ANCA-associated vasculitides, yet only a subset of patients test positive for ANCA.
- Myths vs. Medical Facts:
- A common misconception is that EGPA is solely a lung disease because of its association with asthma; in fact, it is a systemic vasculitis that can affect multiple organs.
- Impact on Specific Populations:
- Women appear to be slightly more affected than men, and the disease often presents in middle age.
- Historical Curiosities:
- The evolution from the original description as Churg-Strauss syndrome to the current nomenclature (EGPA) reflects a deeper understanding of its pathogenesis and clinical spectrum.
References
- Mayo Clinic. (2023). Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss Syndrome) Overview.
- National Institutes of Health. (2022). Advances in Vasculitis Research and Management.
- Johns Hopkins Medicine. (2023). Understanding EGPA: Symptoms, Diagnosis, and Treatment.
- UpToDate. (2023). Diagnosis and Management of Eosinophilic Granulomatosis with Polyangiitis.
- Global Health Statistics. (2023). Epidemiology of Rare Vasculitides Worldwide.
- World Health Organization. (2023). Guidelines for the Management of Systemic Vasculitis.
- Nature Reviews. (2023). Emerging Therapeutic Strategies in Vasculitis.
- BMJ. (2023). EGPA: Myths, Realities, and Clinical Implications.
- ClinicalTrials.gov. (2023). Ongoing Studies in EGPA Treatment.
This detailed report on EGPA provides an in-depth overview of its definition, historical evolution, clinical presentation, underlying causes, risk factors, complications, diagnostic methods, treatment strategies, and emerging research directions. Early recognition and tailored treatment remain essential to improve outcomes and reduce long-term organ damage in patients with EGPA.