Emphysema Treatment
Below is a comprehensive, structured report on emphysema treatment. This report outlines the definition, historical evolution, clinical presentation, diagnostic workup, treatment strategies, prevention methods, and future research directions for managing emphysema. It is designed to serve as a resource for both the general public and healthcare professionals.
1. Overview
What is Emphysema Treatment?
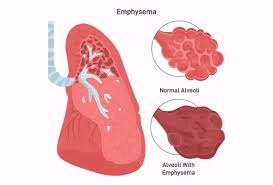
Emphysema treatment refers to the range of medical, rehabilitative, and surgical interventions aimed at managing emphysema—a form of chronic obstructive pulmonary disease (COPD) characterized by irreversible damage to the alveoli (air sacs) in the lungs. The goal of treatment is to relieve symptoms, slow disease progression, and improve quality of life.
Definition and Affected Body Parts/Organs
- Definition: Emphysema treatment involves both pharmacological and non-pharmacological strategies that target the underlying lung damage and its complications. This includes smoking cessation, bronchodilator therapy, corticosteroids, oxygen supplementation, pulmonary rehabilitation, and in selected cases, surgical interventions.
- Affected Organs:
- Lungs: Primarily the alveoli, where the destruction of alveolar walls leads to decreased gas exchange.
- Secondary Effects: Reduced lung function can affect the heart (via pulmonary hypertension and cor pulmonale) and overall systemic oxygen delivery.
Prevalence and Significance
- Emphysema is a major component of COPD, affecting millions worldwide.
- It is strongly linked to smoking and environmental pollutants, making it a significant public health concern.
- Effective treatment is crucial not only for symptom management but also for reducing the risk of severe complications such as respiratory failure and cardiovascular events.
2. History & Discoveries
When and How Was Emphysema Treatment First Identified?
- Early pathological descriptions of emphysema date back to the 19th century, with initial treatments focusing primarily on symptom relief.
- Over time, the evolution of pulmonary medicine led to the development of specific interventions aimed at improving lung function.
Who Discovered It?
- No single individual is credited with discovering emphysema treatment; rather, it evolved through contributions from pulmonologists, respiratory therapists, and clinical researchers.
Major Discoveries and Breakthroughs
- Smoking Cessation: Recognized as the single most effective intervention in the 20th century.
- Bronchodilators and Inhaled Corticosteroids: Development of these medications in the latter half of the century improved symptom control.
- Oxygen Therapy: Its introduction significantly enhanced survival rates and quality of life for advanced patients.
- Surgical Innovations: Procedures such as lung volume reduction surgery (LVRS) and, later, lung transplantation have offered options for severe emphysema.
Evolution of Medical Understanding Over Time
- The transition from symptomatic management to a multifaceted, personalized treatment approach reflects advances in both our understanding of emphysema pathophysiology and therapeutic technologies.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Shortness of breath during exertion
- Chronic, persistent cough
- Mild wheezing or chest tightness
- Advanced-Stage Symptoms:
- Severe dyspnea even at rest
- Marked exercise intolerance
- Significant weight loss and muscle wasting
- Cyanosis (bluish discoloration due to low oxygen levels)
Common vs. Rare Symptoms
- Common: Gradual onset of breathlessness, chronic cough, and fatigue.
- Rare: In some patients, complications such as spontaneous pneumothorax (collapsed lung) or acute exacerbations can occur.
How Symptoms Progress Over Time
- Emphysema is a progressive disease. Early symptoms may be subtle and easily attributed to aging or lack of fitness, while later stages are characterized by rapidly worsening respiratory function and frequent exacerbations that require hospitalization.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- Smoking: The leading cause, resulting in chronic inflammation and alveolar destruction.
- Alpha-1 Antitrypsin Deficiency: A genetic disorder that predisposes individuals to early-onset emphysema.
- Environmental Causes:
- Long-term exposure to air pollutants, dust, and chemical fumes.
Genetic and Hereditary Factors
- A genetic predisposition, particularly alpha-1 antitrypsin deficiency, increases susceptibility to emphysema even in non-smokers.
Known Triggers or Exposure Risks
- Smoking (both active and passive)
- Occupational exposures to dust and chemical irritants
- Air pollution and secondhand smoke
- Recurrent respiratory infections may exacerbate lung damage over time.
5. Risk Factors
Who Is Most at Risk?
- Age: Typically affects individuals over 40 years of age.
- Gender: Historically more common in men; however, with changing smoking patterns, the prevalence among women is rising.
- Occupation & Lifestyle: Individuals with prolonged exposure to cigarette smoke or industrial pollutants are at higher risk.
Environmental, Occupational, and Genetic Influences
- Chronic exposure to environmental pollutants and occupational hazards significantly increases risk.
- A family history of lung disease or genetic disorders (e.g., alpha-1 antitrypsin deficiency) further predisposes individuals.
Impact of Pre-existing Conditions
- Coexisting respiratory conditions, such as chronic bronchitis or asthma, can compound lung damage and worsen outcomes.
6. Complications
What Complications Can Arise from Emphysema?
- Respiratory Failure: Advanced emphysema can lead to inadequate gas exchange, resulting in chronic respiratory failure.
- Pulmonary Hypertension and Cor Pulmonale: Increased pressure in the pulmonary arteries can strain the heart.
- Infections: Increased risk of lung infections and exacerbations.
- Cardiac Complications: The strain on the heart can lead to cardiovascular events.
Long-Term Impact on Organs and Overall Health
- Persistent hypoxemia (low blood oxygen) and hypercapnia (high blood carbon dioxide) can cause multi-organ dysfunction.
- Reduced quality of life and decreased physical capacity are common, with significant impacts on daily living.
Potential Disability or Fatality Rates
- Emphysema is a leading cause of morbidity and mortality worldwide, especially when compounded by other forms of COPD.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical History and Physical Examination: Assessing symptoms such as chronic cough, dyspnea, and exposure history.
- Pulmonary Function Tests (PFTs):
- Spirometry is essential for measuring airflow limitation and determining disease severity.
- Imaging:
- Chest X-ray and CT Scan: Identify characteristic hyperlucency, bullae, and destruction of alveolar walls.
- Blood Tests:
- Assessment of arterial blood gases to evaluate oxygen and carbon dioxide levels.
Early Detection Methods and Their Effectiveness
- Early detection through routine PFTs in high-risk populations (smokers, individuals with occupational exposures) is critical for timely intervention and better outcomes.
8. Treatment Options
Standard Treatment Protocols
- Smoking Cessation: The most important step in halting disease progression.
- Medications:
- Bronchodilators: Short- and long-acting agents to relax airway muscles.
- Inhaled Corticosteroids: Reduce airway inflammation.
- Phosphodiesterase-4 Inhibitors: May help reduce exacerbations in advanced cases.
- Oxygen Therapy: For patients with chronic hypoxemia to improve quality of life and reduce mortality.
- Pulmonary Rehabilitation: Exercise training, nutritional counseling, and education to improve functional capacity.
Medications, Surgeries, and Therapies
- Surgical Interventions:
- Lung Volume Reduction Surgery (LVRS): Removes damaged lung tissue to improve respiratory mechanics.
- Lung Transplantation: Considered in advanced, end-stage disease.
- Emerging Treatments and Clinical Trials:
- Investigational drugs targeting inflammation and oxidative stress.
- Regenerative medicine approaches, including stem cell therapies, are under study to repair lung tissue damage.
Emerging Treatments and Clinical Trials
- New bronchodilators, anti-inflammatory agents, and combination therapies are being evaluated in clinical trials.
- Ongoing research into minimally invasive surgical techniques and novel therapeutic modalities offers promise for future treatment improvements.
9. Prevention & Precautionary Measures
How Can Emphysema Be Prevented?
- Primary Prevention:
- Smoking cessation is paramount.
- Avoidance of environmental and occupational pollutants.
- Lifestyle Changes:
- Regular exercise and a healthy diet support overall lung health.
- Use of personal protective equipment in high-risk occupational settings.
- Preventive Screenings and Vaccinations:
- Annual influenza and pneumococcal vaccinations help prevent respiratory infections that can exacerbate emphysema.
- Routine lung function tests for high-risk individuals are essential for early detection and intervention.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Emphysema, as a major component of COPD, affects millions worldwide—particularly in regions with high smoking prevalence and industrial pollution.
- It represents a significant portion of COPD cases, with prevalence varying by geographic area and socioeconomic status.
Mortality and Survival Rates
- Emphysema contributes substantially to global mortality related to respiratory diseases.
- Improved treatments have increased survival in many regions, yet mortality remains high among advanced cases.
Country-Wise Comparison and Trends
- Developed countries with robust healthcare systems tend to have better screening, management, and outcomes.
- In developing regions, limited access to early diagnosis and treatment contributes to higher morbidity and mortality rates.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Pharmacotherapy:
- SGLT2 inhibitors and other novel agents are under investigation for their potential to reduce inflammation and slow emphysema progression.
- Technological Innovations:
- Advances in imaging and biomarker discovery are improving early diagnosis and personalized treatment plans.
- Surgical and Regenerative Therapies:
- Minimally invasive surgical techniques and studies on lung regeneration via stem cells hold promise for future interventions.
Ongoing Studies and Future Medical Possibilities
- Clinical trials are actively exploring combination therapies that address both airway inflammation and alveolar repair.
- Personalized medicine approaches, informed by genetic and biomarker profiles, may soon optimize treatment for individual patients.
Potential Cures or Innovative Therapies Under Development
- While a definitive cure for emphysema is not yet available, advances in regenerative medicine and novel drug therapies are paving the way for treatments that may significantly slow or even partially reverse lung damage.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Emphysema Treatment
- Silent Progression:
- Many patients with early emphysema may remain asymptomatic for years, making routine screening vital.
- Myths vs. Medical Facts:
- A common misconception is that emphysema only affects long-term smokers; however, genetic factors like alpha-1 antitrypsin deficiency can cause emphysema in non-smokers.
- Impact on Specific Populations:
- Changes in smoking habits and industrial exposures have altered the epidemiology of emphysema, with rising incidence in populations once considered at lower risk.
- Historical Curiosities:
- Early treatments were largely supportive and symptomatic, while today’s multifaceted approach targets underlying pathophysiological processes.
References
- Mayo Clinic. (2023). Chronic Obstructive Pulmonary Disease (COPD) and Emphysema Overview.
- National Institutes of Health. (2022). Advances in Pulmonary Medicine: From Smoking Cessation to Surgical Innovations.
- Johns Hopkins Medicine. (2023). Understanding COPD: Emphysema Diagnosis and Management.
- UpToDate. (2023). Diagnosis and Management of Emphysema.
- American Heart Association. (2023). Impact of Respiratory Diseases on Cardiovascular Health.
- Global Health Statistics. (2023). Epidemiology of COPD and Emphysema Worldwide.
- World Health Organization. (2023). Preventive Strategies for Chronic Respiratory Diseases.
- Nature Reviews. (2023). Emerging Therapies in Pulmonary Medicine.
- ClinicalTrials.gov. (2023). Ongoing Research in Emphysema Treatment.
- BMJ. (2023). Myths and Realities in the Management of Emphysema.
This detailed report on emphysema treatment provides an in-depth overview of its definition, historical evolution, clinical features, diagnostic methods, treatment options, preventive measures, and emerging research trends. It underscores the importance of early intervention, lifestyle modifications, and innovative therapies to improve outcomes and quality of life for individuals affected by this chronic respiratory condition.