Ulcerative Colitis Treatment: A Comprehensive Report
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Over the past decades, treatment strategies have evolved significantly to improve patient quality of life and manage disease progression. This report outlines key aspects of ulcerative colitis treatment, including historical milestones, symptomatology, causative factors, risk profiles, complications, diagnostic procedures, standard and emerging therapies, preventive measures, global trends, recent research, and interesting insights.
1. Overview
What is Ulcerative Colitis Treatment?
Ulcerative colitis treatment encompasses the various medical and surgical interventions used to manage inflammation, control symptoms, induce and maintain remission, and improve long-term outcomes in patients with UC.
Concise Yet Detailed Definition
- Definition: Ulcerative colitis treatment involves a multidisciplinary approach that includes anti-inflammatory drugs, immunosuppressive agents, biologic therapies, and, in advanced cases, surgical interventions to remove diseased portions of the colon.
- Goals: The primary objectives are to reduce inflammation, alleviate symptoms, prevent flare-ups, and minimize complications.
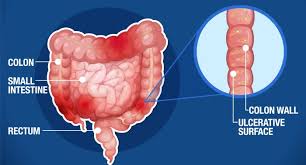
Affected Body Parts/Organs
- Primary Organs: The colon and rectum are the main sites affected by ulcerative colitis.
- Secondary Impact: Inflammation can also indirectly affect overall nutritional status and, through systemic inflammation, other organ systems.
Prevalence and Significance of the Disease
- Prevalence: UC affects millions worldwide, with higher incidence in North America and Europe. Its prevalence has been rising in newly industrialized countries.
- Significance: Due to its chronic nature, ulcerative colitis significantly impacts quality of life and healthcare systems. Effective treatment is essential to prevent complications such as colon cancer, strictures, and severe bleeding. cite
2. History & Discoveries
When and How Was Ulcerative Colitis Treatment First Identified?
- Early Descriptions: Historical texts from the 19th century first described ulcerative lesions in the colon, though the disease was often confused with other gastrointestinal disorders.
- Modern Diagnosis: The advent of colonoscopy and histopathological techniques in the 20th century allowed for more precise identification of UC.
Who Discovered It?
- Pioneers: Early gastroenterologists and pathologists helped delineate ulcerative colitis as a distinct clinical entity, but its exact origins remain multifactorial with contributions from many researchers over time.
Major Discoveries and Breakthroughs in Research and Treatment
- Medical Advancements: The introduction of corticosteroids in the 1950s was a breakthrough in managing acute flares.
- Immunosuppressants: The later development of drugs such as azathioprine and 6-mercaptopurine revolutionized long-term management.
- Biologic Therapies: More recently, biologic agents (e.g., anti-TNF drugs, integrin inhibitors, interleukin inhibitors) have provided targeted approaches to control inflammation and induce remission.
Evolution of Medical Understanding Over Time
- Shifting Paradigms: Initial treatment focused on symptomatic relief and dietary modification. Over time, the understanding of immune dysregulation in UC has shifted treatment toward immunomodulation and targeted biologics.
- Personalized Care: Ongoing research has led to a more personalized approach, taking into account genetic, microbial, and environmental factors in disease management. cite
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Abdominal pain and cramping
- Frequent, small-volume bloody stools
- Urgency and tenesmus (the sensation of incomplete evacuation)
- Advanced-Stage Symptoms:
- Severe, persistent diarrhea
- Significant rectal bleeding
- Weight loss, fatigue, and malnutrition
- Systemic symptoms such as fever in cases of severe flare-ups
Common vs. Rare Symptoms
- Common Symptoms: Include diarrhea, rectal bleeding, abdominal pain, and urgency.
- Rare Symptoms: Some patients may experience extraintestinal manifestations like joint pain, skin lesions (e.g., erythema nodosum), and eye inflammation (uveitis).
How Symptoms Progress Over Time
- Intermittent Flares: UC is characterized by periods of remission interspersed with flare-ups. Early symptoms can gradually worsen during a flare, with potential long-term complications developing if inflammation is not controlled.
4. Causes
Biological and Environmental Causes
- Biological Causes: Although the exact cause remains unclear, ulcerative colitis is believed to result from an inappropriate immune response to intestinal microbiota in genetically susceptible individuals.
- Environmental Influences: Diet, stress, and exposure to certain pathogens have been implicated in triggering disease flares.
Genetic and Hereditary Factors
- Genetic Predisposition: Family history is a known risk factor, with several susceptibility genes identified (e.g., variants in the IL-23 receptor gene).
- Hereditary Factors: Genetic studies suggest a complex inheritance pattern that influences disease onset and severity.
Known Triggers or Exposure Risks
- Triggers: Antibiotic use, diet high in fat and low in fiber, smoking (paradoxically, smoking appears protective in UC but harmful in Crohn’s disease), and stress can trigger flares.
- Exposure Risks: Changes in gut microbiota and exposure to environmental toxins may also contribute.
5. Risk Factors
Who Is Most at Risk?
- Age: UC can develop at any age but commonly presents in young adults between 15 and 35 years.
- Gender: Both genders are affected, although some studies suggest slight differences in incidence and severity.
- Lifestyle: Diet, stress, and use of certain medications may influence risk.
Environmental, Occupational, and Genetic Factors
- Environmental: Urban living and industrialized diets are associated with higher UC rates.
- Occupational: There is no specific occupational risk; however, lifestyle factors linked to occupation (e.g., stress) may play a role.
- Genetic: A positive family history increases the likelihood of developing the condition.
Impact of Pre-Existing Conditions
- Comorbidities: Patients with other autoimmune conditions may have an increased risk, and the presence of primary sclerosing cholangitis is a known risk factor for more severe disease.
6. Complications
What Complications Can Arise from Ulcerative Colitis Treatment?
- Surgical Complications: Long-term treatment may lead to surgery, which carries risks such as infection, bleeding, or pouchitis following an ileal pouch-anal anastomosis.
- Medication Side Effects: Long-term use of corticosteroids or immunosuppressants can lead to osteoporosis, increased infection risk, and other systemic effects.
Long-Term Impact on Organs and Overall Health
- Colon Cancer Risk: Chronic inflammation increases the risk of colorectal cancer.
- Quality of Life: Ongoing symptoms and treatment side effects can lead to significant morbidity, impacting physical, emotional, and social well-being.
Potential Disability or Fatality Rates
- Disability: Severe cases and complications may lead to long-term disability, while the mortality rate is generally low if managed properly.
- Fatality: Mortality is most commonly linked to complications such as severe infections or cancer, rather than the disease itself.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation: Detailed patient history and symptom assessment.
- Colonoscopy: Gold standard for visualizing mucosal inflammation and obtaining biopsy samples.
- Imaging: CT scans or MRI may be used in specific circumstances to assess the extent of inflammation or complications.
Medical Tests
- Blood Tests: To detect anemia, elevated inflammatory markers (CRP, ESR), and to monitor medication side effects.
- Stool Tests: To rule out infectious causes of colitis.
Early Detection Methods and Their Effectiveness
- Screening: Colonoscopy is essential for early diagnosis and cancer surveillance in long-standing ulcerative colitis.
- Biomarkers: Research into fecal calprotectin and other noninvasive biomarkers has improved early detection and monitoring of disease activity. cite
8. Treatment Options
Standard Treatment Protocols
- Medications:
- Aminosalicylates (5-ASA): Used for mild to moderate disease to reduce inflammation.
- Corticosteroids: Short-term use for acute flare-ups.
- Immunomodulators: Such as azathioprine or 6-mercaptopurine for maintaining remission.
- Biologics: Anti-TNF agents (infliximab, adalimumab), integrin inhibitors, and interleukin inhibitors for moderate to severe disease.
- Surgical Options: In cases refractory to medical therapy, total proctocolectomy with ileal pouch-anal anastomosis may be necessary.
Medications, Surgeries, and Therapies
- Medications: Combination therapy is often used to induce remission and then maintain it.
- Surgical Interventions: Surgery is considered when complications arise or if medical management fails.
- Emerging Therapies: Novel small-molecule inhibitors (e.g., JAK inhibitors) and newer biologics are being tested in clinical trials.
Emerging Treatments and Clinical Trials
- Innovative Approaches: Research into stem cell therapy, personalized medicine, and microbiome-targeted treatments shows promise.
- Clinical Trials: Ongoing studies are evaluating combination regimens and next-generation biologic agents to improve outcomes and minimize side effects.
9. Prevention & Precautionary Measures
How Can Ulcerative Colitis Treatment Be Prevented or Optimized?
- Early Intervention: Timely diagnosis and appropriate treatment initiation can prevent complications.
- Regular Monitoring: Surveillance colonoscopies and monitoring of inflammatory markers are crucial for early detection of complications.
- Lifestyle Modifications: Diet, stress management, and smoking cessation (even though smoking appears protective in UC, cessation is advised for overall health) can help mitigate flares.
Lifestyle Changes and Environmental Precautions
- Dietary Adjustments: A balanced diet tailored to individual tolerance may reduce symptom severity.
- Stress Management: Techniques such as mindfulness and counseling can improve quality of life.
- Patient Education: Ongoing education about disease management and adherence to treatment regimens is critical.
Vaccines or Preventive Screenings
- Preventive Screenings: While there is no vaccine for ulcerative colitis, regular colonoscopic surveillance helps in early cancer detection.
- Immunizations: Patients on immunosuppressive therapy should stay updated with vaccinations (e.g., influenza, pneumococcal) to prevent infections.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Global Impact: Ulcerative colitis is most prevalent in North America and Europe, with increasing rates in Asia and other developing regions.
- Prevalence Trends: Incidence rates have been rising, possibly due to improved diagnostic techniques and lifestyle changes.
Mortality and Survival Rates
- Mortality: While UC itself is rarely fatal, long-term complications such as colorectal cancer can affect survival.
- Survival: With effective treatment and regular monitoring, most patients maintain a good quality of life.
Country-Wise Comparison and Trends
- Developed Regions: Countries with advanced healthcare systems report better outcomes and lower complication rates.
- Developing Countries: Limited access to specialized care may contribute to higher complication rates and delayed diagnoses. cite
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Biologic Agents: Continuous improvements in biologic therapies have provided better control of inflammation and maintenance of remission.
- Targeted Therapies: The development of JAK inhibitors and other small molecules offers promising alternatives for patients who do not respond to conventional treatments.
- Microbiome Research: Studies exploring the gut microbiota’s role in UC pathogenesis are paving the way for novel therapeutic approaches.
Ongoing Studies and Future Medical Possibilities
- Precision Medicine: Research is focusing on tailoring treatment based on genetic, immunologic, and microbial profiles.
- Innovative Clinical Trials: Trials are underway to assess combination therapies and new drug classes that aim to improve long-term outcomes with fewer side effects.
Potential Cures or Innovative Therapies Under Development
- Stem Cell Therapy: Early studies into mesenchymal stem cell therapy offer potential for tissue regeneration and immune modulation.
- Next-Generation Biologics: Advances in biologic engineering may lead to more effective, durable therapies with a lower risk of adverse effects.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Ulcerative Colitis Treatment
- Surgical “Cure”: For many patients with refractory disease, surgery (total proctocolectomy) is considered curative for colonic symptoms, though it comes with its own challenges.
- Microbiota Connection: Research is increasingly highlighting how alterations in the gut microbiome may not only contribute to UC pathogenesis but also serve as targets for treatment.
- Extraintestinal Manifestations: Beyond gastrointestinal symptoms, ulcerative colitis can affect the skin, eyes, and joints, necessitating a holistic treatment approach.
Myths and Misconceptions vs. Medical Facts
- Myth: “Surgery is always a last resort.”
- Fact: In certain severe or refractory cases, surgery can significantly improve quality of life and reduce long-term cancer risk.
- Myth: “Ulcerative colitis treatment only involves medication.”
- Fact: A multidisciplinary approach—including lifestyle modification, psychosocial support, and surgical intervention when needed—is essential.
Impact on Specific Populations or Professions
- Age and Gender: UC often begins in young adulthood, impacting career and personal life. Both men and women are affected, though disease severity can vary.
- Occupational Challenges: Chronic symptoms can lead to work absences and reduced productivity; thus, supportive workplace policies are important.
- Global Disparities: Access to advanced treatment varies worldwide, highlighting the need for global health initiatives to address disparities in IBD care.
References & Further Reading
- American College of Gastroenterology (ACG): Guidelines on the diagnosis and management of inflammatory bowel disease.
- Mayo Clinic: Comprehensive patient information on ulcerative colitis treatment options and management strategies.