Ulcerative Colitis Diet
Below is a comprehensive, well-organized report on the “Ulcerative Colitis Diet,” which examines the dietary strategies and nutritional management approaches recommended for individuals with ulcerative colitis. This report also integrates background information on ulcerative colitis itself to better understand how diet plays a role in symptom management and overall health.
1. Overview
What is the Ulcerative Colitis Diet?
The Ulcerative Colitis Diet refers to a range of dietary strategies and nutritional modifications specifically designed to help manage the symptoms and inflammation associated with ulcerative colitis (UC), a chronic inflammatory bowel disease affecting the colon.
Definition:
This diet involves adjusting food choices and meal patterns to reduce intestinal irritation, support gut healing, and minimize flare-ups. It is not a one-size-fits-all prescription but rather a personalized approach that may include low-residue diets, elimination of trigger foods, and nutritional supplementation.
Affected Body Parts/Organs:
- Colon: The primary site affected by ulcerative colitis where inflammation and ulcerations occur.
- Rectum: Often involved in the inflammatory process, contributing to common symptoms.
- Small Intestine (in some cases): While UC mainly affects the colon, dietary choices can impact the overall gastrointestinal tract and microbiome.
Prevalence and Significance:
- Ulcerative colitis affects millions globally and is a significant cause of morbidity among young and middle-aged adults.
- Effective dietary management is an essential component of overall treatment, helping to reduce symptoms, improve quality of life, and potentially decrease reliance on medications during remission periods.
2. History & Discoveries
Initial Recognition of Dietary Impact:
- While ulcerative colitis as a clinical entity has been recognized for over a century, the role of diet in managing its symptoms gained attention in the mid-20th century.
- Early observations noted that certain foods could trigger flare-ups, leading clinicians to recommend dietary modifications.
Key Figures and Breakthroughs:
- Gastroenterologists and nutrition researchers have contributed to the evolution of dietary strategies over the decades.
- The development of the low-residue diet in the 1970s was one major milestone, designed to reduce stool volume and minimize colon irritation during active inflammation.
- More recently, diets such as the Specific Carbohydrate Diet (SCD) and low FODMAP approaches have been studied for their potential to modulate gut microbiota and reduce symptoms.
Evolution of Medical Understanding:
- Early dietary recommendations were based on trial and error; however, advances in nutritional science and a better understanding of the gut microbiome have led to more targeted and individualized dietary interventions.
- Modern studies now examine how food components, such as fiber types, fats, and carbohydrates, interact with the immune system and intestinal lining in UC patients.
3. Symptoms
Note: This section reviews the symptoms of ulcerative colitis—understanding these symptoms is crucial for tailoring dietary recommendations.
Early Symptoms:
- Mild Diarrhea: Often with occasional blood or mucus.
- Abdominal Cramping and Urgency: Discomfort may begin subtly.
- Fatigue and Loss of Appetite: Related to chronic inflammation and nutrient malabsorption.
Advanced-Stage Symptoms:
- Severe and Frequent Diarrhea: Can lead to dehydration and electrolyte imbalances.
- Intense Abdominal Pain and Cramping: Reflecting significant colon inflammation.
- Rectal Bleeding and Weight Loss: Indicative of ongoing intestinal damage.
- Systemic Symptoms: Such as fever or joint pain due to extraintestinal manifestations.
Symptom Progression and Dietary Impact:
- The intensity of symptoms can vary over time, with flare-ups often linked to dietary triggers.
- Adjusting dietary patterns can help mitigate early symptoms and may prevent progression to more severe stages.
4. Causes
Note: Although the diet itself does not cause ulcerative colitis, certain foods may exacerbate the condition.
Biological and Environmental Causes of Ulcerative Colitis:
- Immune-Mediated Inflammation: UC is believed to arise from an abnormal immune response in genetically predisposed individuals.
- Gut Microbiome Dysbiosis: An imbalance in intestinal bacteria may trigger or worsen inflammation.
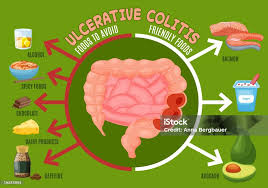
- Dietary Triggers: Certain foods (e.g., high-fiber, spicy foods, dairy in lactose-sensitive individuals) can irritate the colon and promote flare-ups.
Genetic and Hereditary Factors:
- A family history of inflammatory bowel disease increases the risk of developing UC.
- Genetic variations may influence how an individual responds to specific dietary components.
Known Triggers and Exposure Risks:
- Stress and Infections: These factors can interact with dietary habits to trigger UC flares.
- Environmental Exposures: Pollution and lifestyle factors may contribute indirectly by affecting gut health.
5. Risk Factors
Who Is Most at Risk?
- Age and Gender: UC commonly manifests in individuals between 15 and 35 years of age, though it can occur at any age; both genders are affected, with slight regional variations.
- Family History: Those with relatives who have inflammatory bowel diseases are at a higher risk.
- Lifestyle Factors: Diet, smoking (though paradoxically, smoking has been associated with a lower risk of UC compared to Crohn’s disease), and stress levels can influence disease onset and progression.
Environmental and Occupational Factors:
- Urban Living: Higher incidence rates have been observed in developed countries, possibly related to diet and lifestyle.
- Occupational Stress: High-stress jobs may indirectly impact disease management through stress-related dietary changes.
Impact of Pre-existing Conditions:
- Individuals with other autoimmune or metabolic conditions may experience more severe symptoms and may need more tailored dietary interventions.
6. Complications
Complications Associated with Ulcerative Colitis (and the Role of Diet):
- Colon Cancer: Long-standing inflammation increases the risk; dietary antioxidants and anti-inflammatory foods may have a protective role.
- Severe Bleeding and Perforation: Active flares can lead to life-threatening complications.
- Malnutrition and Vitamin Deficiencies: Poor nutrient absorption and restrictive diets can exacerbate deficiencies, affecting overall health.
- Osteoporosis: Chronic inflammation and corticosteroid use can contribute to bone density loss, where dietary calcium and vitamin D play important roles.
Long-Term Impact on Health:
- Effective dietary management may help reduce the severity and frequency of complications, thereby improving long-term outcomes and quality of life.
7. Diagnosis & Testing
Note: While diagnosis of ulcerative colitis is primarily clinical and endoscopic, dietary assessment is a critical component of overall management.
Common Diagnostic Procedures for Ulcerative Colitis:
- Colonoscopy: Visual examination of the colon to assess inflammation and ulceration.
- Biopsy: Tissue samples help confirm diagnosis and rule out other conditions.
- Blood Tests: Check for anemia, inflammation markers (C-reactive protein), and liver function.
- Stool Tests: To exclude infections and evaluate for inflammatory markers.
Role of Dietary Assessment:
- Nutritional Evaluations: Dietitians conduct detailed assessments to identify trigger foods and nutritional deficiencies.
- Food Diaries: Patients may keep records of dietary intake and symptom patterns to help tailor dietary modifications.
Early Detection Methods and Their Effectiveness:
- Routine screenings and prompt endoscopic evaluation in symptomatic individuals are key.
- Early dietary interventions, when combined with medical treatments, can help manage symptoms more effectively.
8. Treatment Options
Standard Treatment Protocols:
- Medical Management: Includes anti-inflammatory medications (e.g., 5-aminosalicylic acid), immunosuppressants, and biologics to control inflammation.
- Surgical Interventions: In severe cases or when complications occur, surgery to remove affected portions of the colon may be necessary.
Dietary Management and Nutritional Therapies:
- Low-Residue Diet: Often recommended during flare-ups to reduce stool volume and ease inflammation.
- Elimination Diets: Identifying and removing specific trigger foods (e.g., dairy, gluten, high-fiber items) may help control symptoms.
- Nutritional Supplementation: Addressing deficiencies (e.g., iron, vitamin D, calcium) is critical, especially during active disease.
- Emerging Dietary Approaches:
- Specific Carbohydrate Diet (SCD): Emphasizes simple, unprocessed foods to reduce gut bacterial imbalance.
- Low FODMAP Diet: Reduces fermentable oligo-, di-, monosaccharides and polyols that can exacerbate symptoms.
Clinical Trials and Future Directions:
- Ongoing research is investigating the role of prebiotics, probiotics, and even fecal microbiota transplantation as adjuncts to dietary therapy.
- Personalized nutrition based on genetic and microbiome analyses is an emerging field aimed at optimizing dietary recommendations for UC patients.
9. Prevention & Precautionary Measures
Diet-Related Preventive Strategies:
- Avoidance of Trigger Foods: Based on individual sensitivity, avoiding spicy foods, high-fat items, or certain fibers during active flares can help reduce symptoms.
- Balanced Nutrition: Maintaining a well-rounded diet with adequate calories, protein, and micronutrients supports overall health and may help prevent malnutrition.
- Hydration: Adequate fluid intake is essential, particularly during diarrhea and flare-ups.
Lifestyle Changes and Environmental Precautions:
- Stress Management: Techniques such as mindfulness, exercise, and adequate sleep can indirectly improve dietary habits and reduce flare risk.
- Regular Medical Follow-Up: Ongoing monitoring allows for timely adjustments in both medication and diet.
Preventive Screenings:
- Nutritional Counseling: Early involvement of dietitians helps tailor dietary plans.
- Routine Colonoscopies: For early detection of dysplasia or colon cancer in long-standing disease.
10. Global & Regional Statistics
Incidence and Prevalence:
- Ulcerative colitis is most common in North America, Europe, and other developed regions, with rising incidence noted in some developing countries as lifestyles and diets westernize.
- Prevalence rates vary by region, reflecting differences in genetics, environment, and dietary patterns.
Mortality and Survival Rates:
- Although UC itself is rarely directly fatal, complications such as colon cancer and severe malnutrition contribute to mortality.
- Early intervention, including appropriate dietary management, has significantly improved survival and quality of life.
Country-Wise Comparison and Trends:
- Developed Countries: Benefit from advanced diagnostic and nutritional management strategies, leading to better outcomes.
- Developing Regions: Limited access to specialized care and nutritional counseling can result in higher complication rates.
11. Recent Research & Future Prospects
Latest Advancements in Dietary Management and Research:
- Microbiome Studies: Research continues to unravel how diet alters gut bacteria, influencing inflammation and symptom severity.
- Personalized Nutrition: Genetic and metabolomic profiling is being explored to customize diets that best suit individual patient needs.
- Innovative Nutritional Therapies: Studies are examining the potential benefits of specific supplements, anti-inflammatory nutrients, and novel dietary patterns tailored for UC patients.
Ongoing Studies and Future Medical Possibilities:
- Clinical trials are assessing the efficacy of combining conventional therapies with specialized diets.
- Future research may lead to the development of “precision diets” that adjust not only to disease activity but also to the patient’s unique metabolic and microbial profile.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about the Ulcerative Colitis Diet:
- Historical Diets: Prior to modern medications, dietary modification was one of the few available treatments and remains a cornerstone of supportive care.
- Individual Variability: No single diet works for all patients; food triggers can be highly individual, highlighting the importance of personalized dietary approaches.
- Role of Fiber: While high-fiber foods are generally beneficial for gut health, during an active flare, certain fibers can aggravate symptoms, prompting the temporary use of low-residue diets.
Myths and Misconceptions vs. Medical Facts:
- Myth: “There is one universal ulcerative colitis diet.”
Fact: Dietary needs vary widely among individuals, and personalized approaches are key. - Myth: “Diet alone can cure ulcerative colitis.”
Fact: While diet is essential for managing symptoms and improving quality of life, it is used in conjunction with medications and other treatments.
Impact on Specific Populations or Professions:
- Pediatric Patients: Children with UC require tailored dietary plans to ensure proper growth and development while managing symptoms.
- Athletes and Active Individuals: Special attention to nutritional balance and hydration is crucial to manage energy levels and recovery while minimizing flare-ups.
References and Further Reading
- Crohn’s & Colitis Foundation: Provides comprehensive guidelines and research updates on dietary management in ulcerative colitis.
- Mayo Clinic: Offers patient-centered information on ulcerative colitis, including dietary recommendations and treatment options.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Details the latest research on inflammatory bowel diseases and nutritional interventions.
- Recent Medical Journals: Publications such as Inflammatory Bowel Diseases and The American Journal of Gastroenterology provide ongoing updates on diet-related studies in UC management.
This report aims to provide a detailed, structured overview of the Ulcerative Colitis Diet, blending insights from historical practices, modern research, and clinical applications. The goal is to offer both the general public and healthcare professionals a clear understanding of how dietary strategies can play a pivotal role in managing ulcerative colitis and improving patient outcomes.