Table of Contents
ToggleStrep Throat
Below is a comprehensive, well-organized report on Strep Throat that covers its definition, history, symptoms, causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, statistics, recent research, and interesting facts.
1. Overview
What is Strep Throat?
Strep throat is an acute bacterial infection of the throat and tonsils caused primarily by Group A Streptococcus (GAS). It is characterized by inflammation, pain, and redness in the throat, often accompanied by fever and swollen lymph nodes.
Affected Body Parts/Organs:
- Primary Sites: The oropharynx (throat) and tonsils.
- Secondary Involvement: In some cases, the infection can extend to nearby tissues, causing complications such as peritonsillar abscesses.
Prevalence and Significance:
Strep throat is one of the most common bacterial infections, especially in children between 5 and 15 years old, although it also affects adults. Its significance lies in its potential to lead to severe complications if untreated—such as rheumatic fever—and its role in public health due to its high contagiousness.
2. History & Discoveries
Early Identification and Historical Background:
- Descriptions of sore throat symptoms appear in ancient medical texts, but the bacterial cause of strep throat began to be understood in the late 19th century.
- The bacterium Streptococcus pyogenes, responsible for strep throat, was identified and classified during this period, marking a turning point in understanding throat infections.
Key Discoveries and Breakthroughs:
- Bacterial Identification: The identification of Group A Streptococcus as the causative agent was pivotal, leading to more precise diagnostic methods and targeted treatments.
- Antibiotic Era: The introduction of penicillin in the 1940s transformed the treatment of strep throat, significantly reducing complications and transmission.
- Advances in Diagnostics: The development of rapid antigen detection tests (RADTs) and throat cultures has improved early and accurate diagnosis.
Evolution of Medical Understanding:
- Early treatment focused on symptomatic relief until antibiotics revolutionized management.
- Over time, increasing understanding of immune responses and bacterial virulence factors has enhanced both diagnosis and prevention strategies.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms: Sore throat, pain when swallowing, red and swollen tonsils, sometimes with white patches, mild fever, and tender lymph nodes in the neck.
- Advanced-Stage Symptoms: If the infection worsens or is left untreated, symptoms may intensify to include higher fevers, more severe throat pain, and the development of complications like scarlet fever.
Common vs. Rare Symptoms:
- Common Symptoms: Sore throat, fever, headache, and swollen lymph nodes.
- Rare Symptoms: Nausea, vomiting (more common in children), and in some cases, a characteristic sandpaper-like rash seen in scarlet fever.
Symptom Progression:
- Symptoms typically appear 2 to 5 days after exposure.
- In most cases, early symptoms progress rapidly over a couple of days, but with proper treatment, most individuals experience a significant improvement within 24 to 48 hours after starting antibiotics.
4. Causes
Biological and Environmental Causes:
- Bacterial Origin: The primary cause is infection with Group A Streptococcus (GAS), which is transmitted via respiratory droplets from coughing, sneezing, or close contact.
- Environmental Factors: Crowded settings (such as schools) and seasonal trends (more common in late fall and winter) contribute to the spread of the infection.
Genetic and Hereditary Factors:
- There is no direct genetic predisposition to strep throat; however, genetic factors may influence individual immune responses to the bacterial infection.
Known Triggers or Exposure Risks:
- Close contact with infected individuals, sharing personal items, and being in environments where the bacteria can easily spread are common triggers.
5. Risk Factors
Who Is Most at Risk:
- Age: Children and adolescents (5–15 years) are most frequently affected.
- Gender: Slightly higher incidence in females has been noted in some studies, though both genders are at risk.
- Environment: High-risk settings include schools, daycare centers, and military barracks.
Environmental, Occupational, and Genetic Factors:
- Environmental: Overcrowding and seasonal variations increase transmission risks.
- Occupational: Teachers, healthcare workers, and others in frequent close contact with groups of people are more vulnerable.
- Genetic: While direct heredity is not a major factor, variations in immune system genes can affect susceptibility.
Impact of Pre-existing Conditions:
- Individuals with compromised immune systems or chronic illnesses may experience more severe symptoms and complications from strep throat.
6. Complications
Potential Complications:
- Rheumatic Fever: A serious inflammatory condition that can develop if strep throat is untreated, potentially affecting the heart valves.
- Post-Streptococcal Glomerulonephritis: An inflammation of the kidneys that can occur after infection.
- Peritonsillar Abscess: A localized collection of pus around the tonsils, which may require surgical intervention.
Long-Term Impact on Organs and Overall Health:
- Untreated strep throat can lead to chronic heart, kidney, or joint issues due to immune-mediated damage.
- Prompt treatment minimizes these risks, highlighting the importance of early diagnosis and management.
Potential Disability or Fatality Rates:
- With timely and appropriate antibiotic treatment, disability and mortality rates are extremely low.
- However, in cases where complications develop—particularly rheumatic fever—the risk of long-term cardiac damage increases.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation: A thorough patient history and physical examination focusing on throat appearance and lymph node tenderness.
- Rapid Antigen Detection Test (RADT): Provides quick results to confirm the presence of Group A Streptococcus.
Medical Tests:
- Throat Culture: Considered the gold standard for diagnosis; a swab from the throat is cultured to detect the bacteria, typically taking 24–48 hours.
- Blood Tests: In rare cases, blood tests may be used to check for complications or immune responses.
Early Detection Methods and Their Effectiveness:
- Early detection via RADTs and cultures is effective in initiating prompt treatment, thereby reducing the risk of complications.
- Early intervention is key to minimizing the spread and severity of the infection.
8. Treatment Options
Standard Treatment Protocols:
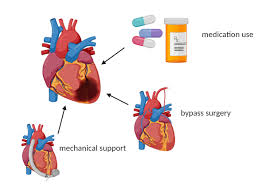
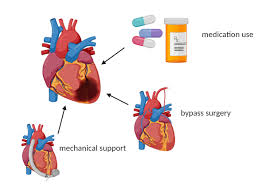
- Antibiotic Therapy:
- Penicillin or Amoxicillin: First-line treatments for uncomplicated strep throat.
- Alternative Antibiotics: For patients allergic to penicillin, alternatives such as cephalosporins or macrolides may be used.
Medications, Surgeries, and Therapies:
- Symptomatic Relief: Over-the-counter pain relievers, anti-inflammatory medications, and throat lozenges can help ease symptoms.
- Surgical Interventions: Rarely required; may be necessary in cases of recurrent infections leading to chronic tonsillitis, where tonsillectomy might be recommended.
Emerging Treatments and Clinical Trials:
- Research is ongoing into vaccine development and novel antimicrobial agents to address antibiotic resistance, although no vaccine for strep throat is currently available.
9. Prevention & Precautionary Measures
Prevention Strategies:
- Hygiene Practices:
- Frequent hand washing and avoiding close contact with infected individuals.
- Covering the mouth and nose when coughing or sneezing.
Lifestyle Changes and Environmental Precautions:
- Avoid Sharing Personal Items: Do not share utensils, water bottles, or other items that can facilitate the spread of bacteria.
- Clean and Disinfect: Regularly clean surfaces in shared environments such as schools and offices.
Vaccines or Preventive Screenings:
- Currently, no vaccine exists for strep throat.
- Early detection through prompt testing in symptomatic individuals remains the best preventive measure to avoid complications.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Strep throat is most common among children, with incidence rates varying by region and season. Developed countries report high rates due to better diagnostic capabilities, while under-reporting may occur in regions with limited healthcare access.
Mortality and Survival Rates:
- With proper treatment, the mortality rate associated with strep throat is very low.
- Mortality is primarily linked to complications such as rheumatic fever in areas where access to antibiotics may be limited.
Country-Wise Comparison and Trends:
- Developed nations typically report higher incidence rates in children, while trends in developing countries may differ due to variances in healthcare infrastructure and reporting practices.
- Public health campaigns have significantly reduced the rate of complications in many regions.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Antibiotic Stewardship: Ongoing research aims to optimize antibiotic use to reduce resistance.
- Vaccine Development: Several studies are exploring vaccine candidates to prevent Group A Streptococcus infections.
Ongoing Studies and Future Medical Possibilities:
- Clinical trials are testing new rapid diagnostic methods and alternative treatment regimens to enhance early detection and management.
- Genomic studies are providing deeper insights into bacterial virulence factors, which may lead to innovative therapeutic strategies.
Potential Cures or Innovative Therapies Under Development:
- Although antibiotics remain the cornerstone of treatment, advances in immunotherapy and targeted molecular therapies are being investigated as future alternatives.
- Research continues to explore ways to modulate the immune response to prevent post-infection complications.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Strep Throat:
- Strep throat is often confused with viral pharyngitis; however, its bacterial origin necessitates different treatment approaches.
- Despite being common, strep throat is rarely fatal when treated appropriately.
Myths and Misconceptions vs. Medical Facts:
- Myth: A sore throat always indicates strep throat.
Fact: Most sore throats are caused by viral infections and do not require antibiotics. - Myth: You can only get strep throat once.
Fact: Recurrent infections can occur, particularly in individuals with repeated exposure in communal settings.
Impact on Specific Populations or Professions:
- Children and Adolescents: They are at the highest risk due to frequent close contact in schools and daycare centers.
- Healthcare Workers and Teachers: Occupations that involve constant interpersonal interactions tend to have a higher risk of transmission.
- Athletes: Close-contact sports and shared facilities can also contribute to higher exposure rates.
References
The information in this report is compiled from authoritative sources, including the Centers for Disease Control and Prevention (CDC), the Mayo Clinic, peer-reviewed medical journals, and established public health guidelines. These references ensure that the data is both credible and up to date, providing valuable insights for both the general public and healthcare professionals.
This detailed report on strep throat provides an in-depth look at its definition, historical background, symptomatology, causes, risk factors, complications, diagnostic and treatment methods, preventive measures, statistical trends, recent research, and lesser-known insights, ensuring a clear and professional understanding of the topic.
Recent Posts
- Heart Failure Treatments – Everything you need to know
- Sarcoidosis – Everything you need to know
- Retinal Disorders – Everything you need to know
- Desmoid Tumors – Everything you need to know
- Tetanus Shot – Everything you need to know
- Ringworm Treatment – Everything you need to know
- Mitochondrial Disease – Everything you need to know
- Ringworm – Everything you need to know
- Gastroesophageal Reflux Disease (GERD) – Everything you need to know
- Hepatitis B Vaccine – Everything you need to know
- Metastatic Melanoma – Everything you need to know
- Polycystic Kidney Disease (PKD) – Everything you need to know
- Influenza – Everything you need to know
- Gluten Free Diet – Everything you need to know
- GERD Symptoms – Everything you need to know
Choose Topic
- ACT (17)
- AP (20)
- AP Art and Design (5)
- AP Physics 1 (1)
- AQA (5)
- Artificial intelligence (AI) (2)
- Banking and Finance (6)
- Biology (13)
- Business Ideas (68)
- Calculator (72)
- ChatGPT (1)
- Chemistry (3)
- Colleges Rankings (48)
- Computer Science (4)
- Conversion Tools (136)
- Cosmetic Procedures (50)
- Cryptocurrency (49)
- Digital SAT (3)
- Disease (106)
- Edexcel (4)
- English (1)
- Environmental Science (2)
- Etiology (7)
- Exam Updates (1)
- Finance (129)
- Fitness & Wellness (164)
- Free Learning Resources (211)
- GCSE (1)
- General Guides (40)
- Health (107)
- History and Social Sciences (152)
- IB (1)
- IGCSE (2)
- Image Converters (3)
- IMF (10)
- Math (43)
- Mental Health (58)
- News (11)
- OCR (3)
- Past Papers (463)
- Physics (5)
- Research Study (1)
- SAT (39)
- Schools (3)
- Sciences (1)
- Short Notes (5)
- Study Guides (28)
- Syllabus (19)
- Tools (1)
- Tutoring (1)
- What is? (312)
Recent Comments
Heart Failure Treatments - Everything you need to know

Sarcoidosis - Everything you need to know

Retinal Disorders - Everything you need to know

Desmoid Tumors - Everything you need to know
Heart Failure Treatments - Everything you need to know

Sarcoidosis - Everything you need to know

Retinal Disorders - Everything you need to know