Table of Contents
ToggleStage 3 Kidney Disease
Below is a comprehensive, well-organized report on Stage 3 Kidney Disease that covers all essential aspects from clinical definition and history to current research trends.
1. Overview
What is Stage 3 Kidney Disease?
Stage 3 kidney disease, also known as moderate chronic kidney disease (CKD), is characterized by a significant loss of kidney function. At this stage, the kidneys are damaged and their ability to filter waste products and excess fluids from the blood is moderately reduced.
Definition:
Stage 3 kidney disease is defined by an estimated glomerular filtration rate (eGFR) of 30–59 mL/min/1.73 m². It is a critical phase where symptoms might begin to appear and complications may arise if the disease is not managed properly.
Affected Body Parts/Organs:
- Kidneys: The primary organs affected; their function is compromised.
- Cardiovascular System: Reduced kidney function can lead to fluid overload, high blood pressure, and increased cardiovascular risks.
- Other Systems: The buildup of toxins may affect various body systems, including the nervous and skeletal systems.
Prevalence and Significance:
- An estimated 10–15% of the adult population in developed countries has some form of CKD, with Stage 3 being one of the most common.
- Stage 3 is significant because early intervention can slow progression to more severe stages, reducing the risk of complications such as cardiovascular events and end-stage renal disease (ESRD).
2. History & Discoveries
Initial Identification and Recognition:
- Kidney disease has been recognized for centuries, but the modern classification and staging system evolved during the 20th century as laboratory testing (such as serum creatinine and eGFR) became available.
- Stage 3 was delineated as part of the broader CKD staging guidelines introduced in the early 2000s by kidney health organizations.
Key Figures and Breakthroughs:
- National Kidney Foundation (NKF): Played a key role in establishing the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines, which standardized CKD staging.
- Advances in Diagnostic Methods: The introduction of eGFR calculations using creatinine levels revolutionized early diagnosis and risk stratification of kidney disease.
Evolution of Medical Understanding:
- Initially, kidney dysfunction was primarily diagnosed in its late stages. With improved diagnostic techniques, clinicians now identify moderate kidney impairment (Stage 3) earlier.
- This evolution has led to a greater focus on preventive care, lifestyle interventions, and the management of comorbidities to slow disease progression.
3. Symptoms
Early Symptoms:
- Subtle or No Symptoms: Many patients may remain asymptomatic in early Stage 3.
- Mild Fatigue: A general sense of tiredness or reduced energy may be noted.
Advanced-Stage Symptoms (Within Stage 3):
- Edema: Swelling in the hands, feet, or around the eyes may occur due to fluid retention.
- Hypertension: High blood pressure is common and may become more difficult to control.
- Changes in Urine: Foamy or discolored urine, though this is less specific.
Common vs. Rare Symptoms:
- Common: Fatigue, loss of appetite, and fluid retention are frequently observed.
- Less Common: Some patients may experience muscle cramps or mild cognitive changes as toxins accumulate.
Symptom Progression:
- As kidney function declines within Stage 3, symptoms may become more noticeable. Monitoring and early management are critical to prevent further progression and complications.
4. Causes
Biological Causes:
- Diabetes and Hypertension: These are the leading causes of CKD and contribute significantly to the progression to Stage 3.
- Glomerulonephritis: Inflammatory diseases of the kidney can lead to chronic damage.
- Polycystic Kidney Disease: A genetic disorder that can lead to progressive kidney impairment.
Environmental Causes and Exposure Risks:
- Nephrotoxic Medications: Prolonged use of certain drugs (e.g., NSAIDs, some antibiotics) can damage kidney tissue.
- Toxins: Exposure to environmental toxins or heavy metals can contribute to kidney damage.
Genetic and Hereditary Factors:
- Family History: A genetic predisposition to kidney disease increases the risk of developing Stage 3 CKD.
- Inherited Disorders: Conditions like Alport syndrome or autosomal dominant polycystic kidney disease (ADPKD) can lead to early kidney damage.
Known Triggers:
- Uncontrolled Chronic Conditions: Poorly managed diabetes or high blood pressure accelerates kidney damage.
- Lifestyle Factors: Obesity, smoking, and a high-salt diet can also trigger or worsen kidney dysfunction.
5. Risk Factors
Who Is Most at Risk?
- Age: Older adults are at higher risk as kidney function naturally declines with age.
- Gender: Some studies suggest men may develop CKD earlier, though both genders are affected.
- Chronic Conditions: Individuals with diabetes, hypertension, or cardiovascular disease are at heightened risk.
Environmental, Occupational, and Genetic Factors:
- Lifestyle: Sedentary behavior, obesity, and high dietary salt intake contribute to the risk.
- Occupational Exposure: Jobs with exposure to nephrotoxic substances can increase the risk.
- Genetics: A family history of CKD or related conditions increases susceptibility.
Impact of Pre-existing Conditions:
- Cardiovascular Disease: Often coexists with CKD and can accelerate its progression.
- Metabolic Syndrome: Conditions such as obesity, insulin resistance, and dyslipidemia are linked to kidney disease.
6. Complications
Potential Complications:
- Progression to End-Stage Renal Disease (ESRD): If untreated, Stage 3 can progress to Stage 4 and eventually ESRD, where dialysis or transplant becomes necessary.
- Cardiovascular Events: Patients with CKD are at increased risk of heart attack, stroke, and other cardiovascular complications.
- Anemia: Reduced kidney function can lead to decreased production of erythropoietin, causing anemia.
- Bone Disease: Imbalances in calcium and phosphate metabolism can lead to renal osteodystrophy.
Long-Term Impact on Health:
- The decline in kidney function can affect nearly every body system, leading to a significant reduction in quality of life.
- Persistent complications may lead to increased hospitalizations and a higher overall healthcare burden.
Potential Disability or Fatality Rates:
- While Stage 3 CKD itself is not immediately life-threatening, its complications, particularly cardiovascular disease, contribute to increased morbidity and mortality in this patient population.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Blood Tests: Measurement of serum creatinine and calculation of eGFR are fundamental.
- Urine Tests: Analysis for proteinuria (excess protein in urine) is a key indicator of kidney damage.
- Imaging Studies: Ultrasound or CT scans can assess kidney size, structure, and any possible obstructions.
- Kidney Biopsy: In some cases, a biopsy may be performed to determine the underlying cause of kidney dysfunction.
Early Detection Methods and Their Effectiveness:
- Routine screening in high-risk populations (e.g., patients with diabetes or hypertension) is critical for early detection.
- Regular monitoring allows for timely intervention to slow progression and manage complications.
8. Treatment Options
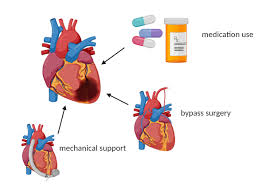
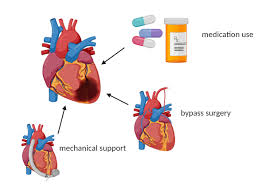
Standard Treatment Protocols:
- Lifestyle Modifications: Dietary changes (e.g., reduced salt intake, balanced protein consumption), regular exercise, and weight management.
- Medication Management:
- Antihypertensives: ACE inhibitors or ARBs to control blood pressure and reduce proteinuria.
- Diabetes Management: Strict glycemic control is essential in diabetic patients.
- Lipid-Lowering Agents: Statins may be prescribed to manage dyslipidemia.
Medications, Surgeries, and Therapies:
- Medical Therapies: Focus on slowing disease progression and managing associated complications.
- Dialysis: Not indicated at Stage 3 but may be discussed as a future option if the disease progresses.
- Emerging Therapies: Research is ongoing into antifibrotic agents and novel treatments aimed at preserving kidney function.
Clinical Trials and Future Directions:
- Several studies are exploring new drugs that target inflammation and fibrosis in CKD.
- Advances in personalized medicine are aiming to tailor treatments based on genetic and molecular profiling.
9. Prevention & Precautionary Measures
Prevention Strategies:
- Early Detection and Management: Regular screening for high-risk individuals to identify kidney impairment early.
- Lifestyle Changes: Adopting a kidney-friendly diet, engaging in regular physical activity, and avoiding nephrotoxic substances.
- Blood Pressure and Diabetes Control: Tight management of these conditions is critical to prevent further kidney damage.
Environmental and Lifestyle Precautions:
- Avoiding Harmful Substances: Minimizing exposure to medications and toxins that can impair kidney function.
- Education and Counseling: Patient education on CKD risk factors and preventive strategies can lead to better long-term outcomes.
Vaccines and Preventive Screenings:
- Although no vaccine exists for CKD, routine health screenings and early interventions play a vital role in prevention.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- CKD affects approximately 10–15% of the adult population in many countries, with Stage 3 being one of the most common stages.
- Rates vary significantly by region, often reflecting differences in the prevalence of diabetes, hypertension, and access to healthcare services.
Mortality and Survival Rates:
- CKD is associated with increased mortality, largely due to cardiovascular complications.
- Early intervention and proper management of Stage 3 can improve survival rates and quality of life.
Country-Wise Comparisons and Trends:
- Developed Countries: More comprehensive screening programs have led to earlier detection and better management.
- Developing Regions: Limited healthcare access may result in underdiagnosis and later presentation, increasing the risk of complications.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- New Therapeutics: Ongoing research into drugs that can reduce kidney fibrosis and inflammation shows promise.
- Biomarker Discovery: Studies are identifying biomarkers that can predict progression from Stage 3 to more severe kidney disease.
- Personalized Medicine: Advances in genetic profiling are paving the way for individualized treatment plans based on a patient’s unique risk factors.
Ongoing Studies and Future Medical Possibilities:
- Clinical trials are underway to assess novel agents that may slow or even reverse kidney damage.
- Research into regenerative medicine and stem cell therapies offers potential future breakthroughs for kidney repair.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Stage 3 Kidney Disease:
- Silent Progression: Many patients are asymptomatic until significant kidney damage has occurred, emphasizing the need for routine screenings.
- Interconnection with Cardiovascular Health: The close link between kidney function and heart health is a major focus of current research.
- Dietary Impact: Emerging evidence suggests that certain dietary patterns—not just salt restriction but also the type and amount of protein—can influence the progression of CKD.
Myths and Misconceptions vs. Medical Facts:
- Myth: “Kidney disease only affects older people.”
Fact: While more common with advancing age, kidney disease can affect younger individuals, especially those with diabetes or hypertension. - Myth: “Once diagnosed with CKD, nothing can be done to slow progression.”
Fact: Early detection and appropriate management—including lifestyle modifications and medications—can significantly slow disease progression.
Impact on Specific Populations or Professions:
- High-Risk Groups: Individuals with diabetes, hypertension, and those with a family history of CKD are at particularly high risk.
- Occupational Hazards: Certain industries with exposure to nephrotoxic chemicals or heavy metals may have higher incidences of kidney disease.
References and Further Reading
- National Kidney Foundation (NKF): Detailed guidelines on CKD stages, management, and lifestyle recommendations.
- Kidney Disease: Improving Global Outcomes (KDIGO): International clinical practice guidelines for CKD evaluation and management.
- Centers for Disease Control and Prevention (CDC): Information on kidney disease prevalence and risk factors.
- Recent Medical Journals: Articles in Clinical Journal of the American Society of Nephrology and American Journal of Kidney Diseases provide ongoing research updates.
This report is intended to provide both the general public and healthcare professionals with a detailed, evidence-based overview of Stage 3 Kidney Disease. It covers clinical definitions, historical evolution, symptomatology, causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, global statistics, and emerging research trends.
Recent Posts
- Heart Failure Treatments – Everything you need to know
- Sarcoidosis – Everything you need to know
- Retinal Disorders – Everything you need to know
- Desmoid Tumors – Everything you need to know
- Tetanus Shot – Everything you need to know
- Ringworm Treatment – Everything you need to know
- Mitochondrial Disease – Everything you need to know
- Ringworm – Everything you need to know
- Gastroesophageal Reflux Disease (GERD) – Everything you need to know
- Hepatitis B Vaccine – Everything you need to know
- Metastatic Melanoma – Everything you need to know
- Polycystic Kidney Disease (PKD) – Everything you need to know
- Influenza – Everything you need to know
- Gluten Free Diet – Everything you need to know
- GERD Symptoms – Everything you need to know
Choose Topic
- ACT (17)
- AP (20)
- AP Art and Design (5)
- AP Physics 1 (1)
- AQA (5)
- Artificial intelligence (AI) (2)
- Banking and Finance (6)
- Biology (13)
- Business Ideas (68)
- Calculator (72)
- ChatGPT (1)
- Chemistry (3)
- Colleges Rankings (48)
- Computer Science (4)
- Conversion Tools (136)
- Cosmetic Procedures (50)
- Cryptocurrency (49)
- Digital SAT (3)
- Disease (106)
- Edexcel (4)
- English (1)
- Environmental Science (2)
- Etiology (7)
- Exam Updates (1)
- Finance (129)
- Fitness & Wellness (164)
- Free Learning Resources (211)
- GCSE (1)
- General Guides (40)
- Health (107)
- History and Social Sciences (152)
- IB (1)
- IGCSE (2)
- Image Converters (3)
- IMF (10)
- Math (43)
- Mental Health (58)
- News (11)
- OCR (3)
- Past Papers (463)
- Physics (5)
- Research Study (1)
- SAT (39)
- Schools (3)
- Sciences (1)
- Short Notes (5)
- Study Guides (28)
- Syllabus (19)
- Tools (1)
- Tutoring (1)
- What is? (312)
Recent Comments
Heart Failure Treatments - Everything you need to know

Sarcoidosis - Everything you need to know

Retinal Disorders - Everything you need to know

Desmoid Tumors - Everything you need to know
Heart Failure Treatments - Everything you need to know

Sarcoidosis - Everything you need to know

Retinal Disorders - Everything you need to know