Hepatitis A
Below is a comprehensive, structured report on Hepatitis A that covers all essential aspects—from an overview and historical context to symptoms, causes, risk factors, complications, diagnosis, treatment, prevention, global statistics, and emerging research. This report is designed to be informative for both the general public and medical professionals.
1. Overview
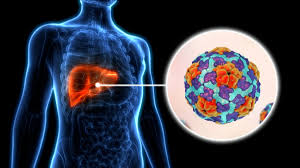
What is Hepatitis A?
Hepatitis A is an infectious liver disease caused by the Hepatitis A virus (HAV). It is primarily transmitted via the fecal-oral route and usually results in acute, self-limited liver inflammation.
Definition:
Hepatitis A is a viral hepatitis that causes inflammation of the liver, leading to symptoms ranging from mild discomfort to severe illness. Unlike other forms of viral hepatitis, it does not typically lead to chronic liver disease.
Affected Body Parts/Organs:
- Liver: The primary organ affected, with inflammation and hepatocellular injury.
- Biliary System: Inflammation may also involve the bile ducts, occasionally causing cholestasis.
Prevalence & Significance:
- Global Impact: Hepatitis A is common in regions with poor sanitation and limited access to clean water. Outbreaks can occur worldwide, particularly among travelers and in developing countries.
- Significance: Although typically self-limiting, hepatitis A can cause significant morbidity, economic burden, and, in rare cases, fulminant hepatitis which may be fatal.
2. History & Discoveries
When and How Was Hepatitis A First Identified?
- Early Recognition: Hepatitis-like illnesses have been described since ancient times, but it was not until the mid-20th century that distinct types of viral hepatitis were recognized.
- Scientific Clarification: In the 1970s, advances in virology led to the identification of Hepatitis A virus as a distinct etiological agent.
Who Discovered It?
- While no single researcher is credited with the discovery of HAV, collaborative efforts by virologists and epidemiologists in the 1970s established its role in acute hepatitis.
Major Discoveries & Breakthroughs:
- Virological Identification: The characterization of HAV and development of serological tests (anti-HAV antibodies) revolutionized diagnosis.
- Vaccine Development: The creation of effective hepatitis A vaccines in the 1990s marked a major breakthrough in prevention.
- Epidemiological Insights: Improved understanding of transmission routes and outbreak patterns has led to enhanced public health measures.
Evolution of Medical Understanding:
From early clinical descriptions to modern molecular diagnostics and vaccination strategies, our understanding of hepatitis A has evolved significantly. Today, emphasis is placed on prevention through improved sanitation, vaccination, and public health education.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
Early Symptoms:
- Fatigue, loss of appetite, and nausea.
- Low-grade fever and malaise.
- Mild abdominal discomfort, particularly in the upper right quadrant.
Advanced-Stage Symptoms:
- Jaundice (yellowing of the skin and eyes) due to significant liver inflammation.
- Dark urine and pale stools.
- Severe fatigue, vomiting, and occasionally joint pain.
Common vs. Rare Symptoms:
- Common:
- Jaundice, fatigue, and gastrointestinal upset (nausea, vomiting).
- Anorexia and malaise.
- Rare:
- In children, the infection is often asymptomatic or produces very mild symptoms.
- Fulminant hepatitis, though rare, can occur, leading to rapid liver failure.
How Symptoms Progress Over Time:
Hepatitis A typically has an incubation period of 15–50 days. Symptoms gradually develop, peak over several weeks, and then resolve over 2–3 months. In most cases, the illness is self-limiting without long-term liver damage.
4. Causes
Biological and Environmental Causes:
- Viral Infection: Hepatitis A is caused by HAV, an RNA virus that primarily spreads via the fecal-oral route.
- Contaminated Food and Water: Poor sanitation and contaminated water are major sources of HAV transmission.
Genetic and Hereditary Factors:
- There is no hereditary predisposition to hepatitis A infection. However, genetic factors might influence the severity of the immune response in an infected individual.
Any Known Triggers or Exposure Risks:
- Travel: International travel to regions with high HAV endemicity increases risk.
- Close Contact: Living in crowded conditions or close contact with an infected person.
- Food Exposure: Consumption of raw or undercooked shellfish from contaminated waters.
5. Risk Factors
Who Is Most at Risk?
- Age: Young children in high-endemic areas often have mild or no symptoms, while older children and adults are more likely to experience severe illness.
- Travelers: Those visiting endemic regions are at increased risk.
- Occupation: Workers in settings with inadequate sanitation may be more susceptible.
- Lifestyle: Poor personal hygiene and lack of access to clean water significantly elevate risk.
Environmental, Occupational, and Genetic Factors:
- Environmental: Poor sanitation and contaminated water supplies.
- Occupational: Certain jobs (e.g., food handlers, sewage workers) may have higher exposure risk.
- Genetic: While not hereditary, variations in immune response genes can affect disease severity.
Impact of Pre-existing Conditions:
- Individuals with chronic liver disease may experience more severe outcomes if infected with HAV.
6. Complications
What Complications Can Arise from Hepatitis A?
- Acute Liver Failure: Though rare, severe cases can progress to fulminant hepatitis.
- Prolonged Recovery: Some individuals may experience extended fatigue and liver dysfunction beyond the acute phase.
- Extrahepatic Manifestations: Rarely, hepatitis A can cause kidney injury, hemolytic anemia, or autoimmune phenomena.
Long-Term Impact on Organs and Overall Health:
- Hepatitis A is typically self-limiting, and most individuals recover completely without chronic liver damage. However, complications can lead to significant short-term morbidity.
Potential Disability or Fatality Rates:
- Fatality rates are generally low (approximately 0.1–0.3%), but they are higher in older adults and individuals with pre-existing liver disease.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation: History and physical examination focusing on symptoms such as jaundice and abdominal pain.
- Serologic Tests: Blood tests to detect anti-HAV IgM (indicative of acute infection) and IgG antibodies (indicative of past infection or immunization).
Medical Tests:
- Liver Function Tests (LFTs): Elevated liver enzymes (ALT, AST) support the diagnosis.
- Viral RNA Detection: In some cases, polymerase chain reaction (PCR) may be used, though serology is the mainstay.
Early Detection Methods and Their Effectiveness:
Routine blood tests for anti-HAV IgM are highly effective in diagnosing acute hepatitis A, allowing for timely intervention and public health measures during outbreaks.
8. Treatment Options
Standard Treatment Protocols:
- Supportive Care: There is no specific antiviral treatment for hepatitis A; management is primarily supportive.
- Hospitalization: In severe cases, especially those with fulminant hepatitis, hospitalization may be required to manage complications.
Medications, Surgeries, and Therapies:
- Rest and Hydration: Ensuring adequate fluid intake and rest.
- Symptom Management: Medications to control nausea, pain, and fever.
- Nutritional Support: A balanced diet to support liver recovery.
Emerging Treatments & Clinical Trials:
- While treatment remains supportive, research is ongoing in areas such as immune modulation and improved supportive therapies for fulminant cases. However, vaccination remains the most effective preventive measure.
9. Prevention & Precautionary Measures
How Can Hepatitis A Be Prevented?
- Vaccination: The hepatitis A vaccine is highly effective and is recommended for travelers, food handlers, and populations in endemic areas.
- Sanitation: Improving water quality, sewage systems, and food hygiene practices.
- Personal Hygiene: Frequent hand washing, particularly after using the bathroom and before eating.
Lifestyle Changes and Environmental Precautions:
- Avoid consuming raw or undercooked shellfish in areas where water quality is questionable.
- Practice safe food and water consumption, especially during travel.
Vaccines or Preventive Screenings:
- A two-dose vaccine series provides long-lasting immunity.
- Routine screening is not typically necessary except in outbreak settings or for high-risk populations.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Hepatitis A is highly endemic in regions with poor sanitation, including parts of Africa, Asia, and Latin America.
- In developed countries, incidence rates are lower due to widespread vaccination and improved sanitation, although outbreaks can still occur.
Mortality and Survival Rates:
- Mortality rates are low in healthy individuals but increase in older adults and those with underlying liver conditions.
- The overall prognosis is good with appropriate preventive measures and supportive care.
Country-Wise Comparison & Trends:
- Developed countries report declining incidence due to effective vaccination programs.
- In contrast, many developing nations continue to face high rates of hepatitis A, highlighting the need for improved public health infrastructure.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Vaccine Development: Ongoing research aims to optimize vaccine schedules and formulations for broader and longer-lasting protection.
- Epidemiological Studies: New studies are refining our understanding of hepatitis A transmission dynamics and risk factors.
- Supportive Care Innovations: Research into better supportive therapies for severe cases is ongoing.
Ongoing Studies & Future Medical Possibilities:
- Clinical trials continue to evaluate immune responses in different populations and investigate novel adjuvants for vaccines.
- Future public health strategies may integrate hepatitis A vaccination with broader STI and infectious disease prevention programs.
Potential Cures or Innovative Therapies Under Development:
- While there is no cure needed for acute hepatitis A given its self-limiting nature, innovations in treatment are focused on improving outcomes for severe cases and minimizing outbreak impacts.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Hepatitis A:
- Silent Infections: Many children in endemic areas experience asymptomatic or mild infections, which can lead to lifelong immunity.
- Outbreaks: Hepatitis A outbreaks are often linked to contaminated food sources, such as shellfish, highlighting the importance of food safety.
- Vaccine Impact: Since the introduction of the vaccine, many developed countries have seen dramatic declines in hepatitis A incidence.
Myths vs. Medical Facts:
- Myth: Hepatitis A always causes severe illness.
Fact: Most infections are mild or asymptomatic, especially in young children. - Myth: Only travelers are at risk.
Fact: While travel to endemic regions increases risk, outbreaks can occur anywhere if sanitation is compromised. - Myth: Once you have hepatitis A, you are immune forever.
Fact: Generally, infection confers lifelong immunity; however, vaccination is still recommended for high-risk individuals to prevent outbreaks.
Impact on Specific Populations or Professions:
- Travelers and Food Handlers: High-risk groups who benefit most from vaccination.
- Public Health Focus: Hepatitis A remains a priority in regions with inadequate sanitation, and effective vaccination programs have significantly reduced disease burden in many parts of the world.
References
- Epidemiological and clinical data are supported by resources from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
- Peer-reviewed studies and clinical reviews in journals on infectious diseases and hepatology provide further insights into diagnostic methods, vaccination impact, and treatment strategies.
This detailed report on Hepatitis A provides an in-depth overview of its clinical features, causes, risk factors, diagnostic approaches, treatment modalities, and prevention strategies. It is intended as a comprehensive resource for understanding this important infectious disease and guiding both public health interventions and clinical practice.