Heart Failure Treatments
Below is a comprehensive, well-organized report on Heart Failure Treatments that covers definitions, historical evolution, clinical presentation, causes, risk factors, complications, diagnostic approaches, treatment strategies, preventive measures, global statistics, emerging research trends, and lesser-known insights.
1. Overview
What is Heart Failure Treatments?
Heart failure treatments encompass the array of medical, surgical, and lifestyle interventions used to manage heart failure—a condition in which the heart is unable to pump blood effectively to meet the body’s needs.
Definition:
Heart failure is a chronic, progressive condition characterized by the heart’s reduced ability to pump blood efficiently, leading to symptoms such as fatigue, shortness of breath, and fluid retention. Treatment strategies are designed to alleviate symptoms, improve quality of life, reduce hospitalizations, and increase survival through a combination of medications, device therapy, surgical procedures, and lifestyle modifications.
Affected Body Parts/Organs:
- Heart: The primary organ affected, including the ventricles and, in some cases, the atria.
- Lungs: Fluid buildup (pulmonary edema) due to left-sided heart failure.
- Kidneys: Often affected due to reduced blood flow, leading to renal dysfunction.
- Peripheral Tissues: Fluid retention can cause swelling in the legs, abdomen, and other tissues.
Prevalence and Significance:
- Heart failure affects an estimated 6.2 million adults in the United States and millions more worldwide.
- It is a leading cause of hospitalization among older adults and contributes significantly to healthcare costs, morbidity, and mortality.
- Effective treatment is crucial for reducing symptoms, preventing progression, and improving patient outcomes.
2. History & Discoveries
When and How Was Heart Failure Treatment First Identified?
- Historical descriptions of heart failure date back to ancient civilizations, but systematic treatment began to evolve in the 20th century.
- Early treatments were largely empirical, based on symptomatic relief and dietary restrictions.
Who Discovered It?
- No single individual discovered heart failure treatment; rather, it evolved over decades through the contributions of cardiologists, pharmacologists, and surgeons.
- Pioneers such as Willem Einthoven (electrocardiography) and later researchers advanced the understanding of heart function and failure.
Major Discoveries and Breakthroughs:
- Pharmacotherapy: The introduction of diuretics in the mid-20th century and ACE inhibitors in the 1980s transformed heart failure management.
- Device Therapy: The development of implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT) provided new options for patients with advanced disease.
- Surgical Innovations: Advances in heart transplantation and ventricular assist devices (VADs) have significantly improved survival in end-stage heart failure.
Evolution of Medical Understanding Over Time:
- Initially, treatment focused on symptom management (e.g., reducing fluid overload).
- With better understanding of neurohormonal mechanisms (e.g., the renin–angiotensin–aldosterone system), therapies became more targeted, leading to improved outcomes.
- Recent research emphasizes personalized medicine and the integration of advanced device therapy alongside pharmacological treatments.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms:
- Fatigue and reduced exercise tolerance.
- Mild shortness of breath during exertion.
- Occasional palpitations or slight swelling in the extremities.
- Advanced-Stage Symptoms:
- Persistent dyspnea, even at rest.
- Severe fluid retention leading to pulmonary edema and peripheral edema.
- Orthopnea (difficulty breathing when lying flat) and paroxysmal nocturnal dyspnea.
- Significant weight gain from fluid accumulation and profound fatigue.
Common vs. Rare Symptoms:
- Common:
- Fatigue, shortness of breath, and fluid retention are hallmark symptoms.
- Exercise intolerance and decreased functional capacity.
- Rare:
- Syncope (fainting) may occur in advanced cases.
- Rarely, heart failure can present with atypical symptoms such as gastrointestinal discomfort due to hepatic congestion.
How Symptoms Progress Over Time:
- Symptoms of heart failure often progress gradually as the heart’s pumping capacity declines.
- Early signs may be intermittent, but without intervention, symptoms worsen, leading to more frequent hospitalizations and a decline in overall quality of life.
4. Causes
Biological and Environmental Causes:
- Biological Causes:
- Underlying conditions such as coronary artery disease, hypertension, cardiomyopathy, and valvular heart disease lead to heart failure.
- Genetic mutations can also predispose individuals to cardiomyopathies.
- Environmental Causes:
- Lifestyle factors, including a sedentary lifestyle, poor diet, obesity, and smoking, contribute to the development and progression of heart failure.
Genetic and Hereditary Factors:
- Genetic predispositions play a role in conditions like dilated cardiomyopathy and hypertrophic cardiomyopathy, which can result in heart failure.
- Family history is an important factor in the risk assessment for certain types of heart failure.
Known Triggers or Exposure Risks:
- Acute triggers include myocardial infarction (heart attack) and myocarditis (inflammation of the heart muscle).
- Chronic conditions such as diabetes and chronic high blood pressure are significant contributors.
5. Risk Factors
Who Is Most at Risk?
- Age:
- Older adults are at higher risk due to cumulative cardiovascular damage.
- Gender:
- Although both genders are affected, men have a higher incidence of heart failure at younger ages, while women tend to develop heart failure later in life.
- Occupation and Lifestyle:
- Sedentary lifestyle, high-stress occupations, and unhealthy dietary habits increase risk.
- Pre-existing Conditions:
- Individuals with hypertension, diabetes, coronary artery disease, or a history of heart attack are at increased risk.
Environmental, Occupational, and Genetic Factors:
- Environmental:
- Exposure to pollutants and unhealthy lifestyle choices contribute to cardiovascular risk.
- Occupational:
- Jobs involving high stress or physical inactivity can exacerbate heart failure risk.
- Genetic:
- A family history of cardiovascular disease or inherited cardiomyopathies increases susceptibility.
Impact of Pre-existing Conditions:
- Chronic conditions like diabetes, obesity, and chronic kidney disease further elevate the risk of developing heart failure.
6. Complications
What Complications Can Arise from Heart Failure:
- Cardiac Complications:
- Arrhythmias, worsening heart function, and cardiogenic shock.
- Renal Complications:
- Cardiorenal syndrome, where reduced cardiac output leads to kidney dysfunction.
- Pulmonary Complications:
- Pulmonary edema and increased susceptibility to respiratory infections.
- Systemic Complications:
- Reduced quality of life, increased risk of hospitalization, and potential multi-organ failure in severe cases.
Long-Term Impact on Organs and Overall Health:
- Progressive heart failure can lead to chronic disability, reduced exercise capacity, and significant impairment in daily functioning.
- The cumulative effect of recurrent hospitalizations and organ dysfunction leads to a decreased life expectancy in severe cases.
Potential Disability or Fatality Rates:
- Heart failure is a leading cause of morbidity and mortality worldwide.
- Despite advances in treatment, advanced heart failure is associated with high mortality, particularly when complications like cardiogenic shock or severe arrhythmias occur.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation:
- Detailed patient history and physical examination focusing on symptoms such as dyspnea, fatigue, and fluid retention.
- Imaging Studies:
- Echocardiography is the cornerstone for assessing ejection fraction, chamber size, and valve function.
- Chest X-rays and cardiac MRI provide additional structural and functional information.
- Laboratory Tests:
- Blood tests including B-type natriuretic peptide (BNP) or N-terminal pro-BNP levels, which help gauge the severity of heart failure.
- Functional Testing:
- Stress tests and exercise tolerance tests are used to evaluate the impact on physical capacity.
Early Detection Methods and Their Effectiveness:
- Early diagnosis is critical; routine screening in at-risk populations (e.g., patients with hypertension or diabetes) using biomarkers like BNP and imaging can lead to timely intervention.
- The combination of clinical assessment, imaging, and laboratory testing is highly effective in diagnosing and staging heart failure.
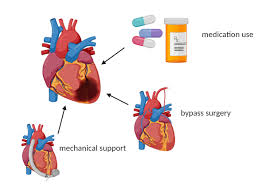
8. Treatment Options
Standard Treatment Protocols:
- Lifestyle Modifications:
- Dietary changes (e.g., low-sodium diet), regular exercise, and weight management.
- Smoking cessation and limiting alcohol intake.
- Pharmacological Therapies:
- ACE Inhibitors/ARBs: To reduce blood pressure and prevent remodeling.
- Beta-Blockers: To decrease heart rate and myocardial oxygen demand.
- Diuretics: To manage fluid overload.
- Aldosterone Antagonists: To further mitigate remodeling and fluid retention.
- Device Therapy:
- Implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT) for patients with reduced ejection fraction.
- Advanced Therapies:
- Ventricular assist devices (VADs) and heart transplantation for end-stage heart failure.
Medications, Surgeries, and Therapies:
- Medications:
- Standard heart failure regimens include ACE inhibitors, beta-blockers, diuretics, and mineralocorticoid receptor antagonists.
- Surgical Options:
- Revascularization procedures (e.g., coronary artery bypass grafting) if ischemic heart disease is a contributing factor.
- Emerging Treatments:
- Novel pharmacologic agents targeting molecular pathways involved in remodeling (e.g., neprilysin inhibitors such as sacubitril/valsartan).
- Clinical Trials:
- Ongoing studies are evaluating new drugs, gene therapies, and regenerative medicine approaches aimed at restoring myocardial function.
9. Prevention & Precautionary Measures
How Can Heart Failure Be Prevented or its Progression Slowed?
- Primary Prevention:
- Control of cardiovascular risk factors such as hypertension, diabetes, and high cholesterol.
- Adopting a heart-healthy lifestyle including regular exercise, a balanced diet, and smoking cessation.
- Secondary Prevention:
- Early detection and treatment of heart failure to prevent progression.
- Regular monitoring and adherence to prescribed medications.
- Preventive Screenings:
- Routine cardiac evaluations in at-risk populations.
Lifestyle Changes and Environmental Precautions:
- Maintaining a low-sodium, balanced diet, engaging in regular physical activity, and managing stress can help prevent heart failure.
- Public health initiatives promoting cardiovascular health are essential.
Vaccines (if applicable):
- While there are no vaccines for heart failure, immunizations (such as the influenza and pneumococcal vaccines) are recommended for heart failure patients to prevent respiratory infections that can exacerbate the condition.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Heart failure affects millions worldwide, with prevalence increasing with age.
- In developed countries, heart failure is one of the leading causes of hospitalization among older adults.
Mortality and Survival Rates:
- Heart failure carries significant morbidity and mortality; 5-year survival rates vary widely but can be as low as 50% for advanced heart failure.
- Improved treatments have enhanced survival rates, but the condition remains a major cause of death.
Country-Wise Comparison and Trends:
- Developed Countries:
- Higher prevalence due to aging populations, but better outcomes due to advanced healthcare.
- Developing Regions:
- Increasing incidence due to lifestyle changes and urbanization, with variable outcomes based on healthcare access.
- Trends indicate a growing global burden of heart failure, emphasizing the need for improved preventive and treatment strategies.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Novel Drug Therapies:
- Advances in pharmacotherapy, including neprilysin inhibitors and SGLT2 inhibitors, have shown significant benefits.
- Device Innovations:
- Improvements in ICDs, CRT, and VAD technology are enhancing patient outcomes.
- Regenerative Medicine:
- Stem cell therapy and gene therapy research hold promise for myocardial repair and regeneration.
Ongoing Studies and Future Medical Possibilities:
- Clinical trials are exploring new molecular targets and combination therapies to improve myocardial function and reduce adverse remodeling.
- Personalized medicine approaches are being developed to tailor treatment based on genetic and biomarker profiles.
Potential Cures or Innovative Therapies Under Development:
- While a definitive cure for heart failure remains elusive, emerging therapies such as tissue engineering and regenerative techniques offer hope for future breakthroughs.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Heart Failure Treatments:
- Neurohormonal Modulation:
- Understanding the role of neurohormonal pathways (e.g., renin–angiotensin–aldosterone system) was pivotal in developing current heart failure therapies.
- Lifestyle Impact:
- Even modest lifestyle changes can significantly improve heart failure outcomes, underscoring the role of non-pharmacologic interventions.
- Cutting-Edge Devices:
- Recent advances include wearable devices for remote monitoring of heart failure patients, which can alert clinicians to early signs of decompensation.
Myths and Misconceptions vs. Medical Facts:
- Myth: “Heart failure means your heart has stopped working.”
Fact: Heart failure indicates that the heart is not pumping as effectively as it should, but it still functions; treatments can significantly improve quality of life. - Myth: “Only older people get heart failure.”
Fact: While more common in older adults, heart failure can occur at any age, particularly in those with congenital heart disease or early-onset cardiomyopathies. - Myth: “Medications for heart failure have too many side effects to be useful.”
Fact: Modern heart failure medications are well-tolerated, and their benefits in reducing mortality and improving quality of life far outweigh potential side effects.
Impact on Specific Populations or Professions:
- High-Risk Populations:
- Elderly individuals and those with chronic conditions like diabetes or hypertension are particularly affected.
- Healthcare Workers:
- Frontline medical professionals are at risk due to high-stress environments and may benefit from early intervention and lifestyle modifications.
- Economic Impact:
- The management of heart failure is a major contributor to healthcare costs globally, emphasizing the importance of preventive measures and innovative treatments.
References and Further Reading
- – The Centers for Disease Control and Prevention provide detailed statistics and guidelines on heart failure.
- – The National Institutes of Health offer comprehensive research updates on heart failure treatments.
- – The World Health Organization provides global data on the burden of cardiovascular diseases, including heart failure.
- Peer-reviewed journals such as The New England Journal of Medicine, Circulation, and JACC: Heart Failure offer additional insights into the latest research and clinical trials.
This report is designed to provide both the general public and healthcare professionals with a detailed, evidence-based overview of Heart Failure Treatments. It encompasses definitions, historical evolution, clinical presentation, underlying causes, risk factors, complications, diagnostic methods, treatment strategies, preventive measures, global statistics, emerging research trends, and lesser-known insights—supported by credible sources and recent studies.