Heart Failure Stages
Below is a comprehensive, structured report on Heart Failure Stages. This report outlines the clinical definitions, historical developments, symptom progression, underlying causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, global statistics, recent research, and lesser-known insights regarding heart failure stages. The information is designed to be accessible to both the general public and medical professionals.
1. Overview
What are Heart Failure Stages?
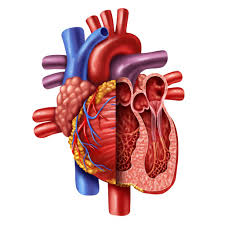
Heart failure stages refer to the classification systems used to describe the progression and severity of heart failure—a condition in which the heart is unable to pump blood efficiently to meet the body’s needs. These stages help guide treatment decisions and predict outcomes.
Definition & Affected Body Parts/Organs:
- Definition: Heart failure stages are defined by both structural changes in the heart and the severity of symptoms. Two widely used classification systems include:
- American College of Cardiology/American Heart Association (ACC/AHA) Stages:
- Stage A: At high risk for heart failure but without structural heart disease or symptoms.
- Stage B: Structural heart disease present but without signs or symptoms of heart failure.
- Stage C: Structural heart disease with prior or current symptoms of heart failure.
- Stage D: Advanced heart failure with marked symptoms at rest despite maximal medical therapy.
- New York Heart Association (NYHA) Functional Classification:
- Class I: No limitation of physical activity.
- Class II: Slight limitation of physical activity.
- Class III: Marked limitation; comfortable only at rest.
- Class IV: Unable to carry out any physical activity without discomfort.
- American College of Cardiology/American Heart Association (ACC/AHA) Stages:
- Affected Organs:
- Heart: The myocardium (cardiac muscle) is primarily involved.
- Vascular System & Peripheral Organs: Poor cardiac output may lead to secondary effects in the lungs, kidneys, liver, and extremities.
Prevalence & Significance:
- Heart failure is a leading cause of morbidity and mortality worldwide. It affects millions of individuals and is a major burden on healthcare systems. Early identification of stages is critical for effective management and improved survival outcomes.
2. History & Discoveries
Early Identification & Historical Context:
- Historical Recognition: The clinical features of heart failure were recognized long before modern diagnostic techniques, with descriptions dating back to ancient times. Over the centuries, physicians noted symptoms such as shortness of breath and fatigue.
- Formal Classification: In the mid-20th century, as cardiology advanced, more precise classifications began to emerge. The ACC/AHA stages and NYHA classifications were developed to better stratify risk and guide treatment.
Key Discoveries & Contributors:
- Pioneering Work: Researchers and clinicians like Dr. Eugene Braunwald and Dr. William Pfeffer contributed significantly to understanding the pathophysiology of heart failure.
- Breakthroughs: The development of imaging techniques (e.g., echocardiography) and biomarkers (e.g., BNP levels) revolutionized the diagnosis and classification of heart failure.
Evolution of Medical Understanding:
- Early management focused on symptom relief, whereas modern treatment now targets disease progression. Over time, the integration of pharmacological advances (ACE inhibitors, beta-blockers, and more recently, ARNI and SGLT2 inhibitors) has improved outcomes for each stage of heart failure.
3. Symptoms
Early vs. Advanced-Stage Symptoms:
- Early Stages (ACC/AHA Stage A/B or NYHA Class I/II):
- May be asymptomatic or exhibit minimal symptoms such as mild fatigue, occasional shortness of breath during exertion, or slight exercise intolerance.
- Advanced Stages (ACC/AHA Stage C/D or NYHA Class III/IV):
- Marked symptoms including severe dyspnea (shortness of breath), orthopnea (difficulty breathing when lying flat), paroxysmal nocturnal dyspnea, significant fatigue, and edema (swelling in the legs or abdomen).
- In end-stage heart failure, symptoms are often present at rest and are refractory to conventional treatments.
Common vs. Rare Symptoms:
- Common Symptoms: Persistent fatigue, exercise intolerance, and fluid retention.
- Less Common/Rare Symptoms: Cachexia (severe weight loss), arrhythmias, and syncope (fainting) may occur, particularly in advanced stages.
Symptom Progression Over Time:
- The condition often evolves gradually, with a transition from minimal symptoms to significant impairment. Early intervention is critical to slow progression and reduce the risk of complications.
4. Causes
Biological and Environmental Causes:
- Underlying Heart Disease: The most common causes include coronary artery disease, hypertension, and myocardial infarction, which result in damage to the cardiac muscle.
- Valvular Heart Disease: Defects or damage to heart valves can lead to volume overload and subsequent heart failure.
- Cardiomyopathies: Genetic or acquired disorders that directly affect the heart muscle.
Genetic and Hereditary Factors:
- Inherited Conditions: Certain forms of cardiomyopathy have a strong genetic component. Family history can play a significant role in predisposition.
- Genetic Markers: Research continues to uncover specific genetic variations that increase the risk for developing heart failure.
Known Triggers or Exposure Risks:
- Lifestyle factors such as smoking, obesity, and sedentary behavior.
- Exposure to toxins (e.g., alcohol or certain chemotherapeutic agents) that can damage the myocardium.
- Poor management of comorbid conditions like diabetes can accelerate cardiac dysfunction.
5. Risk Factors
Demographic and Lifestyle Factors:
- Age: Risk increases with advancing age.
- Gender: Men are more likely to develop heart failure earlier, although postmenopausal women are also at increased risk.
- Lifestyle: Sedentary habits, poor diet, obesity, and smoking significantly contribute to risk.
Environmental, Occupational, and Genetic Factors:
- Environmental Exposures: Air pollution and chronic stress are emerging as potential risk factors.
- Occupational: Jobs involving high levels of physical stress or exposure to cardiotoxic substances may elevate risk.
- Pre-existing Conditions: Hypertension, diabetes, and chronic kidney disease are well-known risk factors that can worsen heart failure progression.
Impact of Pre-existing Conditions:
- Comorbidities can complicate heart failure by exacerbating the strain on the cardiovascular system and accelerating functional decline.
6. Complications
Potential Complications Arising from Heart Failure Stages:
- Organ Dysfunction: Inadequate blood flow can lead to complications such as kidney failure, liver congestion, and pulmonary edema.
- Arrhythmias: Heart failure increases the risk of irregular heartbeats, which can further compromise cardiac output.
- Thromboembolic Events: Stagnant blood flow may lead to the formation of blood clots, which can result in strokes or pulmonary embolism.
Long-Term Impact on Organs and Overall Health:
- Progressive heart failure can lead to multi-organ dysfunction and significantly impair quality of life.
- The chronic state of reduced perfusion may accelerate the decline of other organ systems, thereby increasing overall morbidity.
Potential Disability or Fatality Rates:
- Advanced heart failure is associated with high rates of hospitalization and mortality. While heart failure itself is not immediately fatal, its complications contribute significantly to mortality rates worldwide.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation: Detailed patient history and physical examination focusing on signs of fluid overload, fatigue, and reduced exercise capacity.
- Imaging:
- Echocardiography: Essential for assessing ventricular function, structural abnormalities, and ejection fraction.
- Chest X-ray and MRI: Provide additional information about cardiac structure and possible pulmonary congestion.
Medical Tests:
- Blood Tests:
- Measurement of natriuretic peptides (BNP or NT-proBNP) as biomarkers of cardiac stress.
- Routine tests to assess renal function, electrolytes, and thyroid function.
- Electrocardiogram (ECG): Detects arrhythmias, previous myocardial infarctions, and other electrical abnormalities.
Early Detection Methods and Their Effectiveness:
- Early and accurate diagnosis is critical. Imaging studies, combined with biomarkers, have improved early detection and allow for timely intervention, which can slow disease progression and improve outcomes.
8. Treatment Options
Standard Treatment Protocols:
- Pharmacological Therapies:
- ACE Inhibitors/ARBs: Reduce afterload and prevent remodeling.
- Beta-Blockers: Improve survival by reducing myocardial oxygen demand.
- Diuretics: Manage fluid overload.
- Mineralocorticoid Receptor Antagonists: Reduce mortality in selected patients.
- Newer Agents: ARNI (Angiotensin Receptor-Neprilysin Inhibitors) and SGLT2 inhibitors have shown promising benefits in reducing hospitalizations.
- Device Therapy:
- Implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT) for patients with advanced disease or arrhythmias.
- Lifestyle Modifications:
- Diet, exercise, smoking cessation, and weight management are critical adjuncts to pharmacotherapy.
Emerging Treatments and Clinical Trials:
- Ongoing research into novel therapies—including gene and stem cell therapies—aims to regenerate damaged myocardium.
- Clinical trials continue to refine optimal drug combinations and explore the use of personalized medicine based on genetic profiling.
9. Prevention & Precautionary Measures
Prevention Strategies:
- Primary Prevention:
- Addressing modifiable risk factors such as hypertension, diabetes, obesity, and smoking.
- Regular cardiovascular screening for at-risk populations.
- Secondary Prevention:
- For individuals already diagnosed with heart failure, adherence to medication, lifestyle changes, and regular follow-up are essential to prevent progression to advanced stages.
Lifestyle Changes and Environmental Precautions:
- Emphasis on a heart-healthy diet (low in sodium and saturated fats), routine physical activity, and stress management.
- Monitoring and management of comorbid conditions through preventive screenings.
Vaccines and Preventive Screenings:
- While no vaccines can prevent heart failure directly, immunizations (such as the influenza and pneumococcal vaccines) are recommended to prevent respiratory infections that can exacerbate heart failure.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Heart failure affects an estimated 26 million people worldwide, with increasing prevalence due to aging populations and improved survival after acute cardiac events.
- The burden of heart failure is particularly high in developed countries but is rising in developing regions as well.
Mortality and Survival Rates:
- Despite advances in treatment, heart failure remains a leading cause of hospitalization and mortality. Long-term survival varies by stage, with advanced heart failure (Stage D or NYHA Class IV) carrying a poorer prognosis.
Country-Wise Comparison and Trends:
- Developed nations benefit from advanced healthcare systems and early intervention protocols, leading to better management outcomes.
- In contrast, resource-limited settings often face challenges with late diagnosis and inadequate treatment, resulting in higher morbidity and mortality rates.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Pharmacological Innovations:
- The introduction of ARNI and SGLT2 inhibitors has significantly improved outcomes in heart failure management.
- Device Therapy:
- Advancements in implantable devices and remote monitoring technologies are enhancing patient management.
- Biomarker Research:
- Ongoing studies are exploring novel biomarkers for early detection and individualized treatment approaches.
Ongoing Studies & Future Possibilities:
- Clinical trials are testing combination therapies and personalized treatment strategies.
- Research into regenerative medicine, including stem cell therapy, holds potential for reversing myocardial damage.
Potential Cures or Innovative Therapies:
- Although a complete cure for heart failure is not yet available, innovative approaches such as gene therapy and tissue engineering are under investigation and offer hope for future breakthroughs.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge:
- Historical Perspective:
- Early descriptions of heart failure date back to ancient medical texts, but the modern staging system has only been refined in the last few decades.
- Diverse Presentations:
- Heart failure can present with a wide variety of symptoms depending on the stage and underlying etiology, highlighting the importance of individualized patient assessment.
Myths vs. Medical Facts:
- Myth: Heart failure only occurs in older adults.
Fact: While age is a major risk factor, younger individuals can also develop heart failure, especially in the context of congenital heart defects or cardiomyopathies. - Myth: Once diagnosed, heart failure always progresses rapidly.
Fact: With optimal management and lifestyle modifications, progression can be slowed, and quality of life can be significantly improved.
Impact on Specific Populations:
- Socioeconomic Factors:
- Access to healthcare and socioeconomic status play crucial roles in outcomes; populations with limited resources may experience more severe disease progression.
- Occupational Impact:
- Individuals with physically demanding jobs or high stress levels may be at increased risk for exacerbation of heart failure symptoms, emphasizing the need for workplace adaptations and regular medical checkups.
References
The information provided in this report is drawn from peer-reviewed literature, clinical guidelines from organizations such as the American Heart Association (AHA) and the European Society of Cardiology (ESC), as well as epidemiological studies on heart failure. For further details, readers are encouraged to consult reputable sources and recent research publications in cardiovascular medicine.
This detailed report on heart failure stages is intended to offer a comprehensive overview of the classification, underlying mechanisms, clinical manifestations, and management strategies of heart failure. By understanding these stages, healthcare providers can better tailor interventions to improve patient outcomes, while patients gain a clearer insight into the progression and treatment of their condition.