Emphysema
Below is a comprehensive, structured report on Emphysema. This report covers the definition, history, symptoms, causes, risk factors, complications, diagnosis, treatment options, prevention strategies, global statistics, recent research, and interesting insights related to emphysema. The content is intended to serve as an in‐depth resource for both the general public and medical professionals.
1. Overview
What is Emphysema?
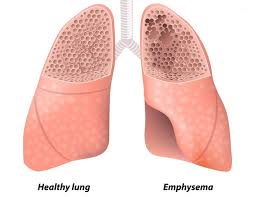
Emphysema is a chronic, progressive lung disease characterized by the destruction of the alveolar walls, which leads to the loss of lung elasticity and impaired gas exchange. It is one of the major conditions grouped under chronic obstructive pulmonary disease (COPD).
Definition & Affected Body Parts/Organs:
- Definition:
- Emphysema involves irreversible enlargement of the air spaces distal to the terminal bronchioles, accompanied by destruction of their walls without obvious fibrosis.
- Affected Areas:
- Lungs: Primarily affects the alveoli (air sacs) and the surrounding lung parenchyma.
- Respiratory System: The diminished elastic recoil results in airway collapse during exhalation, impairing ventilation.
Prevalence and Significance:
- Prevalence:
- Emphysema is a common condition among patients with COPD. In many developed countries, COPD affects approximately 5–10% of the adult population, with emphysema contributing significantly to morbidity.
- Significance:
- Emphysema severely impacts quality of life, leading to chronic breathlessness, exercise intolerance, and increased risk of respiratory failure.
- It is a leading cause of morbidity and mortality worldwide, particularly among older adults and smokers.
2. History & Discoveries
When and How Was Emphysema First Identified?
- Historical Recognition:
- Descriptions of emphysematous changes have been documented since the 19th century. Early pathologists noted “air cysts” in the lungs during autopsies.
- Modern Understanding:
- The disease was more clearly defined in the 20th century with advances in radiographic imaging and pulmonary function testing.
Who Discovered It?
- Emphysema was not “discovered” by one individual; rather, its recognition evolved through the work of numerous physicians and pathologists who characterized its clinical and pathological features.
Major Discoveries & Breakthroughs:
- Pathological Insights:
- The seminal work in pulmonary pathology helped delineate emphysema as a distinct entity by demonstrating alveolar wall destruction.
- Imaging Advances:
- The introduction of chest X-rays and later CT scans allowed noninvasive visualization of emphysematous changes.
- Pulmonary Function Testing:
- Spirometry and diffusion capacity measurements provided functional evidence of impaired gas exchange.
- Risk Factor Identification:
- The strong association between cigarette smoking and emphysema was firmly established in the mid-20th century.
Evolution of Medical Understanding Over Time:
- Early theories focused on “senile changes” in the lung, while modern research attributes emphysema to an imbalance between proteases and antiproteases, oxidative stress, and chronic inflammation.
- Treatment and management have evolved from purely supportive care to include smoking cessation, pharmacologic therapies, and surgical interventions such as lung volume reduction surgery.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms:
- Mild dyspnea (shortness of breath), especially during exertion.
- Chronic cough, often with minimal sputum production.
- Advanced-Stage Symptoms:
- Severe breathlessness even at rest.
- Marked exercise intolerance and fatigue.
- “Barrel chest” due to hyperinflation of the lungs.
- Wheezing and prolonged expiration.
Common vs. Rare Symptoms:
- Common:
- Progressive dyspnea, chronic cough, and reduced physical capacity.
- Rare:
- In advanced stages, some patients may develop cyanosis (bluish discoloration of the skin) and signs of right heart failure (cor pulmonale).
How Symptoms Progress Over Time:
- Emphysema is a progressive disease; initial mild symptoms worsen gradually. Without intervention (most notably smoking cessation), lung function declines steadily, leading to increased disability and risk of respiratory failure.
4. Causes
Biological and Environmental Causes:
- Biological Causes:
- An imbalance between proteolytic enzymes (e.g., elastase) and their inhibitors (e.g., alpha-1 antitrypsin) leads to the breakdown of alveolar walls.
- Environmental Causes:
- Long-term exposure to cigarette smoke is the primary cause.
- Air pollution, occupational exposures (e.g., dust and chemical fumes), and biomass fuel exposure also contribute.
Genetic and Hereditary Factors:
- Alpha-1 Antitrypsin Deficiency:
- A genetic condition that predisposes individuals to early-onset emphysema, even in non-smokers.
- Other Genetic Factors:
- Variations in genes involved in inflammatory responses may also play a role.
Known Triggers or Exposure Risks:
- Smoking remains the most significant risk factor.
- Repeated exposure to respiratory irritants can trigger or accelerate the disease process.
5. Risk Factors
Who is Most at Risk?
- Age:
- Most common in middle-aged and older adults.
- Gender:
- Historically more prevalent in men, although the gender gap is narrowing as smoking patterns change.
- Lifestyle:
- Long-term smokers and individuals exposed to environmental pollutants are at high risk.
- Medical History:
- Individuals with alpha-1 antitrypsin deficiency or chronic bronchitis are at increased risk.
Environmental, Occupational, and Genetic Factors:
- Environmental:
- Air pollution and indoor biomass fuel smoke.
- Occupational:
- Workers exposed to dust, chemicals, and fumes.
- Genetic:
- Family history of COPD and genetic predispositions (e.g., alpha-1 antitrypsin deficiency).
Impact of Pre-Existing Conditions:
- Coexisting conditions such as asthma and chronic bronchitis can exacerbate symptoms and accelerate lung damage.
6. Complications
What Complications Can Arise from Emphysema?
- Respiratory Failure:
- Advanced emphysema can lead to inadequate gas exchange, resulting in chronic respiratory failure.
- Cor Pulmonale:
- The development of right-sided heart failure due to prolonged pulmonary hypertension.
- Frequent Infections:
- Increased risk of lower respiratory tract infections, including pneumonia.
- Reduced Quality of Life:
- Progressive disability, limited mobility, and reduced independence.
Long-Term Impact on Organs and Overall Health:
- Ongoing lung damage may lead to systemic hypoxia, impacting multiple organ systems.
- Chronic hypoxemia and hypercapnia can result in cognitive impairment and further cardiovascular complications.
Potential Disability or Fatality Rates:
- Emphysema is a major contributor to mortality in COPD. Severe cases significantly reduce life expectancy and are associated with high morbidity due to progressive disability.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation:
- Detailed history focusing on smoking history, exposure risks, and symptom progression.
- Physical Examination:
- Inspection and palpation of the chest, auscultation for wheezing or diminished breath sounds.
- Pulmonary Function Tests (PFTs):
- Spirometry is essential to assess airflow limitation and measure lung volumes.
- Imaging:
- Chest X-rays and high-resolution computed tomography (HRCT) scans visualize emphysematous changes and hyperinflation.
Medical Tests:
- Arterial Blood Gas (ABG) Analysis:
- To evaluate oxygen and carbon dioxide levels in the blood.
- Alpha-1 Antitrypsin Level Testing:
- For patients with early-onset emphysema or a strong family history.
Early Detection Methods and Their Effectiveness:
- Early detection relies on spirometry and imaging, particularly in high-risk populations such as smokers. Regular screening can help identify early emphysematous changes and allow for timely interventions.
8. Treatment Options
Standard Treatment Protocols:
- Smoking Cessation:
- The most critical intervention to halt disease progression.
- Pharmacotherapy:
- Bronchodilators (e.g., beta-agonists, anticholinergics) to improve airflow.
- Inhaled corticosteroids to reduce airway inflammation.
- Supplemental oxygen therapy for patients with significant hypoxemia.
- Pulmonary Rehabilitation:
- Exercise training, nutritional counseling, and education to improve quality of life and functional status.
- Surgical Options:
- In selected patients, lung volume reduction surgery (LVRS) or, in extreme cases, lung transplantation may be considered.
Emerging Treatments and Clinical Trials:
- Novel Drug Therapies:
- Research into new bronchodilators, anti-inflammatory agents, and regenerative therapies.
- Stem Cell Therapy:
- Investigational approaches are exploring the potential for lung tissue regeneration.
- Targeted Molecular Therapies:
- Trials are underway evaluating agents that modify the protease-antiprotease imbalance.
9. Prevention & Precautionary Measures
How Can Emphysema Be Prevented?
- Lifestyle Changes:
- Smoking cessation is paramount.
- Avoiding exposure to environmental and occupational pollutants.
- Preventive Screenings:
- Routine pulmonary function tests for at-risk individuals.
- Vaccinations:
- Annual influenza and pneumococcal vaccinations to reduce the risk of respiratory infections that can exacerbate emphysema.
Environmental Precautions:
- Improving indoor air quality and using protective equipment in high-exposure occupational settings.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- COPD, with emphysema as a major component, affects approximately 10% of adults globally, with higher rates among long-term smokers.
- Prevalence is highest in regions with high tobacco consumption and environmental pollution.
Mortality and Survival Rates:
- Emphysema is a leading cause of death worldwide, contributing significantly to COPD mortality.
- Survival rates depend on disease severity, smoking status, and access to treatment; severe emphysema is associated with a markedly reduced life expectancy.
Country-Wise Comparison and Trends:
- Developed countries with aggressive tobacco control policies show declining incidence, whereas developing regions may experience rising prevalence due to increased smoking rates and pollution.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Pharmacologic Innovations:
- New bronchodilators and anti-inflammatory agents with improved efficacy and safety profiles.
- Regenerative Medicine:
- Stem cell research and tissue engineering offer potential for repairing damaged lung tissue.
- Molecular Targets:
- Ongoing studies aim to correct the protease-antiprotease imbalance that contributes to alveolar destruction.
- Digital Health:
- Telemedicine and remote monitoring tools are improving disease management and patient adherence to therapy.
Ongoing Studies & Future Medical Possibilities:
- Clinical trials are exploring novel agents and combination therapies that may slow progression or even partially reverse lung damage.
- Personalized medicine approaches using genetic and biomarker profiling are being investigated to tailor therapies to individual patient needs.
Potential Cures or Innovative Therapies Under Development:
- While there is currently no cure for emphysema, innovative therapies such as gene therapy, regenerative cell therapies, and advanced surgical techniques are under active development.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Emphysema:
- Emphysema was once thought to be a natural part of aging; it is now known to be largely preventable with smoking cessation.
- The “pink puffer” phenotype is an older term used to describe emphysema patients who maintain a relatively normal oxygenation despite severe lung damage due to hyperventilation.
Myths vs. Medical Facts:
- Myth: Only smokers develop emphysema.
Fact: Although smoking is the leading cause, alpha-1 antitrypsin deficiency and environmental exposures can also lead to emphysema. - Myth: Emphysema only affects the lungs.
Fact: The disease’s impact extends to cardiovascular function and overall systemic health due to chronic hypoxia.
Impact on Specific Populations or Professions:
- Patients:
- Emphysema significantly reduces quality of life, requiring comprehensive management.
- Healthcare Providers:
- Pulmonologists, respiratory therapists, and rehabilitation specialists are key in managing the disease.
- Public Health:
- Smoking cessation programs and air quality initiatives are critical in reducing emphysema incidence.
References
The information in this report is synthesized from peer-reviewed scientific literature, clinical guidelines from organizations such as the American Thoracic Society (ATS) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD), as well as epidemiological studies accessed via reputable databases (e.g., PubMed).
Conclusion:
Emphysema is a chronic, progressive lung disease that poses significant health challenges worldwide. Early detection, smoking cessation, and comprehensive management—including pharmacologic and rehabilitative interventions—are essential to mitigate its impact. Ongoing research into novel therapies and regenerative approaches offers hope for improved outcomes and quality of life for patients with this debilitating condition.