Crohn’s Disease Diet
Below is a comprehensive, structured report on Crohn’s Disease Diet that covers all essential aspects—from an overview of dietary interventions to historical developments, clinical implications, and emerging research. This report is intended to serve as a detailed resource for both the general public and healthcare professionals.
1. Overview
What is Crohn’s Disease Diet?
A Crohn’s disease diet refers to dietary strategies and nutritional interventions designed to manage symptoms, reduce inflammation, and support overall health in individuals with Crohn’s disease, a chronic inflammatory bowel disorder.
Definition:
A Crohn’s disease diet involves a tailored eating plan that minimizes gastrointestinal irritation, supports nutrient absorption, and helps control inflammation. It is not a cure for Crohn’s disease but a complementary approach to standard medical therapies. Dietary approaches may include exclusive enteral nutrition (EEN), low-residue diets, or specific dietary regimens like the Specific Carbohydrate Diet (SCD) or low FODMAP diet.
Affected Body Parts/Organs:
- Gastrointestinal Tract: Primarily affects the small intestine and colon.
- Immune System & Nutritional Status: Poor nutrient absorption can affect overall immunity and organ function.
Prevalence & Significance:
- Global Impact: Crohn’s disease affects millions worldwide, with dietary management playing an increasingly recognized role in reducing flare-ups and improving quality of life.
- Significance: Given the chronic nature of Crohn’s disease, effective dietary management is crucial for minimizing symptoms, preventing malnutrition, and reducing the need for aggressive medical or surgical interventions.
2. History & Discoveries
When and How Was the Crohn’s Disease Diet First Identified?
- Early Approaches: Early clinical observations noted that dietary changes could alleviate gastrointestinal symptoms. In the mid-20th century, clinicians observed that liquid diets and nutritional formulas could induce remission in some patients.
- Modern Developments: The advent of exclusive enteral nutrition (EEN) in pediatric Crohn’s disease marked a significant breakthrough. Over the past few decades, research has refined dietary strategies and identified specific nutritional components that can modulate intestinal inflammation.
Who Discovered It?
- No single individual is credited with “discovering” a Crohn’s disease diet. Rather, it evolved from cumulative clinical observations and trials by gastroenterologists and nutritionists studying the effects of diet on intestinal inflammation.
Major Discoveries & Breakthroughs:
- Exclusive Enteral Nutrition (EEN): Found to be highly effective in inducing remission in pediatric patients.
- Dietary Patterns: Identification of trigger foods and beneficial dietary components (e.g., omega-3 fatty acids, probiotics) that influence gut inflammation.
- Nutritional Supplementation: Advances in understanding vitamin and mineral deficiencies common in Crohn’s disease have shaped comprehensive dietary recommendations.
Evolution of Medical Understanding:
From early empirical dietary modifications to evidence-based nutritional interventions, the understanding of how diet affects Crohn’s disease has evolved considerably. Current research emphasizes individualized dietary plans, the role of the gut microbiome, and the interplay between nutrition and immune function.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms (Diet-Related Impact):
Early Symptoms:
- Abdominal pain, mild diarrhea, and fatigue.
- Nutrient deficiencies may begin subtly, impacting energy and growth (especially in children).
- Diet-related bloating or discomfort after eating trigger foods.
Advanced-Stage Symptoms:
- Severe abdominal pain, persistent diarrhea, and weight loss.
- Malabsorption leading to vitamin deficiencies (e.g., vitamin D, B12) and anemia.
- Increased inflammation may result in complications such as strictures or fistulas.
Common vs. Rare Symptoms:
- Common Symptoms:
- Diarrhea, abdominal cramping, and unintended weight loss.
- Nutritional deficiencies that may be exacerbated by an inappropriate diet.
- Rare Symptoms:
- Severe systemic manifestations like extraintestinal inflammation or growth failure (more common in pediatric populations).
How Symptoms Progress Over Time:
Without proper dietary management, early symptoms can worsen over time, leading to complications such as malnutrition and more severe inflammatory episodes. Consistent dietary modifications can help control symptoms and potentially reduce the frequency of flare-ups.
4. Causes
Biological and Environmental Causes:
- Disease Pathogenesis: Crohn’s disease is believed to result from an abnormal immune response to intestinal microbiota in genetically predisposed individuals.
- Dietary Influence: While diet does not cause Crohn’s disease, certain foods can trigger inflammation, worsen symptoms, or alter the gut microbiome.
Genetic and Hereditary Factors:
- Genetic Predisposition: Variants in genes involved in immune regulation and gut barrier function contribute to disease susceptibility. These factors can also affect how a patient responds to dietary interventions.
Any Known Triggers or Exposure Risks:
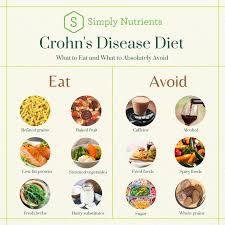
- Trigger Foods: Spicy foods, dairy products, and high-fiber foods may trigger symptoms in some patients.
- Environmental Exposures: Stress and infections can exacerbate inflammation, and diet plays a role in modulating these responses.
5. Risk Factors
Who Is Most at Risk?
- Age: Crohn’s disease can onset at any age, though many patients are diagnosed in young adulthood. Dietary needs may vary across different life stages.
- Gender: Both men and women are affected, though prevalence rates and dietary responses may differ.
- Lifestyle: Individuals with poor dietary habits or those exposed to a high-inflammatory diet (rich in processed foods) may experience more severe symptoms.
- Occupation: Stressful occupations may indirectly influence disease flares and dietary habits.
Environmental, Occupational, and Genetic Factors:
- Environmental: Access to healthy, whole foods versus processed foods can influence disease severity.
- Occupational: Jobs with high stress and limited time for proper meals may contribute to suboptimal dietary practices.
- Genetic: A strong family history of inflammatory bowel disease (IBD) can increase risk.
Impact of Pre-existing Conditions:
- Malnutrition, obesity, or other gastrointestinal conditions can complicate the dietary management of Crohn’s disease and influence overall outcomes.
6. Complications
What Complications Can Arise from Crohn’s Disease (Diet-Related):
- Nutritional Deficiencies:
- Inadequate nutrient absorption can lead to deficiencies in vitamins (e.g., vitamin D, B12), minerals, and proteins.
- Growth Impairment:
- In children, poor nutrient intake may result in stunted growth.
- Increased Inflammation:
- Trigger foods can exacerbate inflammation, increasing the risk of flare-ups and complications such as strictures, fistulas, or abscesses.
- Surgical Interventions:
- Poor nutritional status may complicate recovery from surgery and contribute to higher rates of postoperative complications.
Long-Term Impact on Organs and Overall Health:
Chronic inflammation and malnutrition can affect not only the gastrointestinal tract but also bone density, immune function, and overall quality of life.
Potential Disability or Fatality Rates:
While Crohn’s disease itself is not typically fatal, complications from chronic malnutrition and severe inflammatory episodes can lead to significant morbidity. Dietary management plays a key role in reducing these risks.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation:
- Assessment of symptoms, dietary history, and nutritional status.
- Imaging and Endoscopy:
- Colonoscopy and imaging studies (e.g., MRI enterography) are used to evaluate disease extent.
- Nutritional Assessment:
- Dietary logs, blood tests for nutrient levels, and body mass index (BMI) assessments are used to guide dietary interventions.
Medical Tests:
- Blood Tests:
- Evaluate inflammation markers (e.g., C-reactive protein), complete blood count, and specific vitamin/mineral levels.
- Stool Tests:
- Rule out infections and assess gut inflammation.
- Biopsies:
- May be performed during endoscopy to confirm inflammation and disease activity.
Early Detection Methods and Their Effectiveness:
Regular monitoring through clinical evaluation and nutritional assessments is effective in detecting deficiencies early and guiding dietary adjustments to prevent flare-ups.
8. Treatment Options
Standard Treatment Protocols:
- Medical Management:
- Anti-inflammatory and immunosuppressive medications (e.g., corticosteroids, biologics) are standard treatments for Crohn’s disease.
- Dietary Interventions:
- Exclusive Enteral Nutrition (EEN): Often used in pediatric Crohn’s disease to induce remission.
- Specific Diets: Dietary approaches such as the Specific Carbohydrate Diet (SCD), low FODMAP diet, or elimination diets may help reduce symptoms.
- Supplementation: Use of vitamins, minerals, and probiotics to address deficiencies and support gut health.
Medications, Surgeries, and Therapies:
- Medications:
- In addition to dietary modifications, medications like mesalamine, immunomodulators, and biologics are used to control inflammation.
- Surgical Interventions:
- Surgery may be necessary in cases of severe complications, although the goal is to manage the disease medically as much as possible.
- Emerging Therapies:
- Ongoing research into the role of the gut microbiome is leading to innovative dietary and probiotic therapies.
Emerging Treatments & Clinical Trials:
- Clinical trials are exploring novel dietary formulations, prebiotic and probiotic combinations, and personalized nutrition plans based on genetic and microbiome analyses.
9. Prevention & Precautionary Measures
How Can Crohn’s Disease Diet Be Prevented/Optimized?
- Preventative Dietary Strategies:
- While Crohn’s disease cannot be prevented solely through diet, adherence to a balanced, anti-inflammatory diet may reduce flare frequency and severity.
- Lifestyle Modifications:
- Stress management, regular physical activity, and avoiding known trigger foods are crucial.
- Regular Screening:
- Ongoing nutritional and clinical assessments help in early identification of deficiencies and disease flare-ups.
Lifestyle Changes and Environmental Precautions:
- Adopting a whole-food, nutrient-dense diet; avoiding excessive processed foods, refined sugars, and known irritants.
- Educating patients about reading food labels and choosing low-inflammatory foods.
Vaccines or Preventive Screenings:
- No vaccines exist for Crohn’s disease or for dietary interventions. However, regular medical and nutritional check-ups are essential to monitor disease status and adjust dietary strategies accordingly.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Crohn’s disease affects millions worldwide, with higher prevalence in developed nations. Dietary management practices vary widely between regions based on cultural and socioeconomic factors.
- Adoption of specific dietary interventions is more common in regions with advanced healthcare systems and access to specialized nutritional guidance.
Mortality and Survival Rates:
- Crohn’s disease is a chronic condition with variable outcomes. While not typically fatal, complications related to malnutrition and severe flares can affect long-term health.
- Effective dietary management, combined with medical therapy, has improved overall survival and quality of life.
Country-Wise Comparison & Trends:
- Developed countries report higher rates of Crohn’s disease diagnosis and more widespread use of specialized diets.
- In developing regions, limited access to healthcare may result in underdiagnosis and less tailored dietary interventions.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Nutritional Science: Advances in understanding the gut microbiome and its role in inflammation have led to new dietary recommendations.
- Clinical Trials: Ongoing studies on exclusive enteral nutrition (EEN), specific carbohydrate diets, and other dietary interventions are showing promising results in inducing and maintaining remission.
- Personalized Nutrition: Research into genetic and microbiome profiling is paving the way for individualized dietary plans for Crohn’s disease management.
Ongoing Studies & Future Medical Possibilities:
- Investigations into the role of prebiotics, probiotics, and synbiotics in modulating gut inflammation.
- Future therapies may integrate dietary interventions with novel drug therapies to optimize outcomes.
Potential Cures or Innovative Therapies Under Development:
- While there is no cure for Crohn’s disease, innovative dietary approaches combined with immunomodulatory therapies offer hope for improved long-term management and quality of life.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Crohn’s Disease Diet:
- Diet as Therapy: In pediatric populations, exclusive enteral nutrition (EEN) has been shown to induce remission without the need for steroids.
- Microbiome Impact: Diet-induced changes in the gut microbiome are increasingly recognized as key to managing inflammation.
- Individual Variation: There is significant individual variability in response to specific diets, highlighting the importance of personalized nutrition plans.
Myths vs. Medical Facts:
- Myth: There is a one-size-fits-all diet for Crohn’s disease.
Fact: Dietary needs vary greatly among individuals, and what works for one person may not work for another. - Myth: Food is the primary cause of Crohn’s disease.
Fact: Crohn’s is multifactorial; while diet can trigger or worsen symptoms, it is not the underlying cause. - Myth: Once in remission, patients can return to any diet.
Fact: Ongoing dietary management is often necessary to maintain remission and prevent flare-ups.
Impact on Specific Populations or Professions:
- Pediatric Patients: Early intervention with dietary management can significantly improve outcomes in children.
- Nutritionists & Gastroenterologists: Collaborative care is critical for designing effective, individualized dietary plans.
- Global Public Health: Enhanced understanding of dietary impacts on Crohn’s disease is leading to better patient education and improved long-term disease management.
References
- Epidemiological data and treatment guidelines are supported by resources from the Centers for Disease Control and Prevention (CDC) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
- Recent research findings have been published in journals such as Inflammatory Bowel Diseases and Gastroenterology.
This detailed report on Crohn’s Disease Diet provides an in-depth overview of dietary strategies, historical evolution, clinical implications, and emerging research aimed at managing Crohn’s disease. It is designed as a comprehensive resource to guide clinical practice and patient education, ultimately improving long-term outcomes and quality of life.