Chiari Malformation
Below is a comprehensive, structured report on Chiari Malformation covering its definition, history, clinical features, causes, risk factors, complications, diagnosis, treatment options, prevention strategies, global statistics, recent research, and additional insights. This report is designed to be informative for both the general public and healthcare professionals alike.
1. Overview
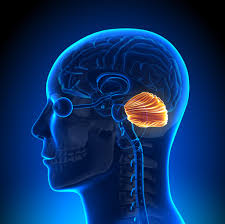
What is Chiari Malformation?
Chiari Malformation is a structural defect in the base of the skull and the cerebellum, the part of the brain that controls balance. In this condition, part of the cerebellum (or sometimes brainstem) protrudes through the foramen magnum—the opening at the base of the skull—into the spinal canal.
Detailed Definition
Chiari Malformation is generally classified into several types based on the severity and the anatomical structures involved. The most common form, Type I, typically presents in adolescents or adults and is characterized by herniation of the cerebellar tonsils. More severe forms (Types II–IV) are usually diagnosed in childhood and involve additional neural abnormalities. The malformation leads to disrupted cerebrospinal fluid (CSF) flow and may cause a range of neurological symptoms.
Affected Body Parts/Organs
- Brain: Primarily affects the cerebellum and, in some types, parts of the brainstem.
- Spinal Cord: The downward displacement of cerebellar tissue can impinge on the upper spinal cord and alter CSF dynamics.
- Cerebrospinal Fluid (CSF) System: Obstruction or altered flow of CSF is a hallmark feature, potentially leading to hydrocephalus.
Prevalence and Significance
Chiari Malformation Type I is estimated to occur in approximately 1 in 1,000 individuals, though many cases remain asymptomatic and undiagnosed. The condition is significant due to its potential to cause chronic pain, neurological deficits, and, in severe cases, life-altering complications. Early recognition and management can help improve quality of life and prevent progression.
2. History & Discoveries
When and How Was Chiari Malformation First Identified?
- Early Descriptions:
The clinical features of Chiari Malformation were first noted in the late 19th century when autopsy findings revealed herniation of the cerebellar tonsils. - Modern Recognition:
The term “Chiari Malformation” was introduced in the early 20th century as neurologists and radiologists began using imaging and autopsy data to define the condition more precisely.
Who Discovered It?
- Key Contributor:
Hans Chiari, an Austrian pathologist, is credited with describing several types of cerebellar herniations in the late 19th century. His work laid the foundation for the classification of Chiari Malformations.
Major Discoveries and Breakthroughs
- Classification System:
Chiari’s original descriptions evolved into a classification system (Types I–IV) based on the severity and extent of cerebellar and brainstem herniation. - Imaging Advances:
The advent of magnetic resonance imaging (MRI) in the 1980s revolutionized the diagnosis of Chiari Malformation, enabling non-invasive visualization of the brain and spinal cord. - CSF Dynamics:
Discoveries related to cerebrospinal fluid flow have provided insights into the symptomatology and complications associated with the malformation.
Evolution of Medical Understanding
Over time, the understanding of Chiari Malformation has evolved from autopsy findings to dynamic, non-invasive imaging techniques and a better grasp of CSF physiology. This progress has informed both conservative and surgical treatment approaches aimed at alleviating symptoms and preventing neurological deterioration.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Occasional headaches, particularly at the back of the head
- Mild dizziness or unsteadiness
- Neck pain or stiffness
- Visual disturbances (e.g., blurred vision) in some cases
- Advanced-Stage Symptoms:
- Severe, chronic headaches often exacerbated by coughing, sneezing, or straining
- Persistent balance problems and vertigo
- Numbness or weakness in the limbs
- Difficulty swallowing (dysphagia) and speech problems
- In severe cases, signs of brainstem dysfunction
Common vs. Rare Symptoms
- Common Symptoms:
Headaches and balance issues are frequently reported in Chiari Malformation Type I. - Rare Symptoms:
Advanced neurological deficits (such as significant motor weakness or respiratory difficulties) are uncommon in Type I but may be observed in more severe forms (Types II–IV).
How Symptoms Progress Over Time
Symptoms of Chiari Malformation often develop gradually. Many individuals with mild forms remain asymptomatic for years, while others may experience a progressive worsening of headaches, balance difficulties, and neurological impairments. The rate of progression can vary significantly among patients.
4. Causes
Biological and Environmental Causes
- Biological Causes:
Chiari Malformation is a congenital anomaly resulting from abnormal development of the skull and cerebellum during fetal growth. Abnormal bone growth can cause a smaller than normal posterior fossa, forcing cerebellar tissue downward. - Environmental Causes:
There is no direct environmental cause, as it is primarily a developmental condition, although factors during pregnancy might play a role.
Genetic and Hereditary Factors
- Genetic Predisposition:
While most cases are sporadic, there is evidence that genetic factors may contribute to the development of Chiari Malformation. Familial occurrences have been documented, suggesting a potential hereditary component.
Known Triggers or Exposure Risks
- Developmental Triggers:
Abnormalities during embryonic development, potentially influenced by genetic and maternal environmental factors. - Associated Conditions:
Chiari Malformation is sometimes associated with other congenital anomalies, such as spina bifida and syringomyelia.
5. Risk Factors
Who Is Most at Risk?
- Age:
Symptoms often become apparent in adolescence or adulthood, although the malformation is congenital. - Gender:
There is no clear gender predominance, although some studies suggest a slight female preponderance. - Lifestyle:
While lifestyle factors do not cause Chiari Malformation, individuals with strenuous physical activities that increase intracranial pressure may notice exacerbation of symptoms. - Pre-existing Conditions:
Patients with associated congenital anomalies or connective tissue disorders may be at higher risk for symptomatic Chiari Malformation.
Environmental, Occupational, and Genetic Factors
- Environmental:
There are no significant environmental risk factors postnatally. - Occupational:
Occupations that involve heavy lifting or straining might exacerbate symptoms. - Genetic:
A family history of Chiari Malformation or other congenital anomalies may increase risk.
Impact of Pre-existing Conditions
- Associated Syndromes:
Conditions such as Ehlers-Danlos syndrome or other connective tissue disorders can exacerbate the severity of Chiari Malformation.
6. Complications
What Complications Can Arise from Chiari Malformation?
- Syringomyelia:
The formation of a fluid-filled cavity (syrinx) within the spinal cord is a common complication. - Neurological Deficits:
Persistent compression of neural structures can lead to motor weakness, sensory loss, and coordination problems. - Brainstem Dysfunction:
In severe cases, compression of the brainstem may result in difficulties with breathing, swallowing, and cardiac regulation. - Chronic Pain:
Ongoing headaches and neck pain can significantly impair quality of life.
Long-term Impact on Organs and Overall Health
Chronic compression of the cerebellum and brainstem can lead to progressive neurological deterioration, while syringomyelia may result in chronic spinal cord dysfunction. These complications can severely impact mobility, sensory function, and overall daily functioning.
Potential Disability or Fatality Rates
While Chiari Malformation itself is not typically fatal, severe complications such as brainstem compression or significant syringomyelia can lead to serious disability and, in rare cases, life-threatening conditions if not properly managed.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
Detailed history and neurological examination focusing on headache, balance issues, and other neurological signs. - Imaging Studies:
Magnetic Resonance Imaging (MRI) is the gold standard for diagnosing Chiari Malformation. It provides detailed images of the brain, cerebellum, and spinal cord. - Electrophysiological Testing:
Nerve conduction studies and evoked potentials may be used to assess associated neurological deficits.
Medical Tests
- MRI:
Essential for visualizing cerebellar tonsillar herniation and associated abnormalities such as syringomyelia. - CT Scan:
May be used when MRI is contraindicated, though it is less sensitive. - CSF Flow Studies:
Phase-contrast MRI can evaluate cerebrospinal fluid dynamics, which is important in assessing the severity of the malformation.
Early Detection Methods and Their Effectiveness
Early detection through MRI, particularly in individuals with a family history or early symptoms, is highly effective. Timely diagnosis allows for appropriate monitoring and intervention, potentially reducing the risk of progressive neurological complications.
8. Treatment Options
Standard Treatment Protocols
- Conservative Management:
- Observation: Asymptomatic or mildly symptomatic patients may be managed with regular follow-up and conservative measures.
- Medications: Pain management with analgesics and anti-inflammatory drugs; physical therapy may help alleviate symptoms.
- Surgical Intervention:
- Posterior Fossa Decompression: The most common surgical treatment for symptomatic Chiari Malformation, aimed at relieving pressure on the cerebellum and brainstem and restoring normal CSF flow.
- Duraplasty: Often performed in conjunction with decompression to expand the dural space.
- Additional Procedures: In cases with associated syringomyelia, shunting procedures may be considered.
Medications, Surgeries, and Therapies
- Medications:
Symptomatic relief with pain relievers (NSAIDs) and muscle relaxants. - Surgical Options:
Posterior fossa decompression is the primary surgical treatment; techniques continue to evolve with improved outcomes and reduced complication rates. - Emerging Treatments:
Research into minimally invasive surgical techniques and the role of adjunctive therapies (e.g., intrathecal medications) is ongoing.
Emerging Treatments and Clinical Trials
- Minimally Invasive Surgery:
Ongoing studies are evaluating endoscopic approaches for decompression. - Targeted Therapies:
Research into pharmacological agents that may improve CSF flow dynamics or reduce inflammation in the region. - Clinical Trials:
Trials assessing long-term outcomes of various surgical techniques and non-surgical interventions are in progress.
9. Prevention & Precautionary Measures
How Can Chiari Malformation Be Prevented?
- Prevention of Congenital Defects:
As a congenital condition, primary prevention is challenging. However, optimal maternal health and avoidance of known teratogens during pregnancy may reduce the overall incidence of congenital anomalies. - Early Monitoring:
In families with a history of Chiari Malformation or related congenital disorders, early screening with fetal or neonatal imaging can facilitate early intervention.
Lifestyle Changes and Environmental Precautions
- Maternal Health:
Maintaining good health during pregnancy through proper nutrition and prenatal care is essential. - Genetic Counseling:
For families with a history of congenital heart or neural tube defects, genetic counseling may provide insight into risks and preventive measures.
Vaccines or Preventive Screenings
- Preventive Screenings:
Routine prenatal ultrasounds and fetal echocardiography/MRI can detect structural abnormalities early. - Vaccines:
There are no vaccines for Chiari Malformation, as it is a developmental condition.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Prevalence:
Chiari Malformation Type I is estimated to occur in approximately 1 in 1,000 individuals, though many remain asymptomatic. - Regional Trends:
The condition is recognized worldwide, with variations in reported prevalence due to differences in diagnostic practices and access to advanced imaging.
Mortality and Survival Rates
- Mortality:
Chiari Malformation itself is rarely fatal; however, complications such as syringomyelia or severe brainstem compression can increase morbidity. - Survival:
With appropriate treatment, especially surgical decompression, long-term survival is excellent, although many patients require lifelong monitoring.
Country-wise Comparison and Trends
- Developed Countries:
Higher detection rates and advanced surgical care contribute to better outcomes. - Developing Countries:
Limited access to MRI and specialized neurosurgical care may result in underdiagnosis and delayed treatment.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- Surgical Innovations:
Advances in posterior fossa decompression techniques, including minimally invasive approaches and intraoperative imaging. - Biomarkers and Genetics:
Ongoing research is investigating genetic markers and molecular pathways that contribute to Chiari Malformation, aiming to improve risk stratification and personalized management. - CSF Flow Studies:
Improved imaging techniques to assess cerebrospinal fluid dynamics are enhancing the understanding of disease severity and guiding treatment decisions.
Ongoing Studies and Future Medical Possibilities
- Clinical Trials:
Trials are ongoing to assess the long-term benefits and safety of various surgical techniques and potential non-surgical therapies. - Precision Medicine:
Future prospects include the integration of genetic and biomarker data to tailor treatment and monitoring protocols for individual patients. - Innovative Therapies:
Research into regenerative therapies and neuroprotective agents may offer new avenues to improve neurological outcomes.
Potential Cures or Innovative Therapies Under Development
While there is currently no cure for Chiari Malformation, emerging therapies focused on advanced surgical techniques and molecular targeting hold promise for reducing symptoms, preventing complications, and enhancing quality of life for affected individuals.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge About Chiari Malformation
- Variable Presentation:
Many individuals with Chiari Malformation Type I are asymptomatic, and the condition is often discovered incidentally during imaging for unrelated issues. - Association with Syringomyelia:
Up to 50% of symptomatic patients may develop syringomyelia, a fluid-filled cyst in the spinal cord, which can further complicate the clinical picture. - Impact on Daily Life:
Even mild cases can significantly affect quality of life due to chronic headaches, balance issues, and fatigue.
Myths and Misconceptions vs. Medical Facts
- Myth: “Chiari Malformation always causes severe symptoms.”
Fact: Many patients remain asymptomatic or have only mild symptoms and may never require surgical intervention. - Myth: “It is solely a congenital disorder with no variability.”
Fact: While it is congenital, the degree of cerebellar herniation and clinical impact vary widely among individuals. - Myth: “Once surgically treated, there is no need for follow-up.”
Fact: Lifelong monitoring is essential due to the risk of residual or progressive complications such as syringomyelia or recurrence of symptoms.
Impact on Specific Populations or Professions
- High-Risk Populations:
Individuals with a family history of Chiari Malformation or related congenital anomalies may be at higher risk. - Occupational Impact:
Professions requiring precise motor coordination or balance (such as athletes or pilots) may be particularly affected by the subtle symptoms of Chiari Malformation. - Economic and Social Impact:
Chronic symptoms can lead to reduced productivity and increased healthcare costs, emphasizing the need for early detection and effective management.
References
- – Provides comprehensive information on the epidemiology, diagnosis, and management of Chiari Malformation.
- – Offers global statistics and public health guidelines on neurological disorders, including Chiari Malformation.
- – Summarizes recent clinical studies and advances in research related to Chiari Malformation.
This report integrates current clinical knowledge and research findings to provide a detailed overview of Chiari Malformation. Understanding its complex pathophysiology, varied clinical presentation, diagnostic strategies, and evolving treatment options is essential for optimizing patient care and guiding future research in this challenging neurological condition.