Bronchiectasis
Below is a comprehensive, structured report on Bronchiectasis. This report covers its definition, history, symptoms, causes, risk factors, complications, diagnostic methods, treatment options, prevention strategies, global statistics, recent research, and interesting insights. The information is based on current scientific literature and clinical guidelines and is intended for both the general public and medical professionals.
1. Overview
What is Bronchiectasis?
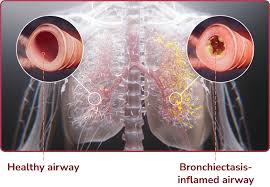
Bronchiectasis is a chronic respiratory condition characterized by permanent dilation and destruction of the bronchial walls. It results from recurrent or chronic inflammation and infection, leading to impaired clearance of secretions and progressive lung damage.
Definition & Affected Body Parts/Organs:
- Definition:
- Bronchiectasis is defined by irreversible bronchial dilatation, wall thickening, and structural lung changes. These alterations are usually associated with chronic infections and inflammation.
- Affected Areas:
- Bronchi and Lungs: Primarily affects the airways, causing mucus retention and repeated infections.
- Respiratory System: Can lead to compromised gas exchange, increased risk of pneumonia, and progressive respiratory failure.
Prevalence and Significance:
- Prevalence:
- Prevalence varies by region and population. In developed countries, bronchiectasis is increasingly recognized due to better imaging and awareness, while in some areas it remains underdiagnosed.
- Significance:
- Bronchiectasis significantly impacts quality of life, causing chronic cough, recurrent infections, and reduced lung function.
- It contributes to increased healthcare utilization and is associated with high morbidity and, in severe cases, mortality.
2. History & Discoveries
When and How Was Bronchiectasis First Identified?
- Early Descriptions:
- Early medical literature dating back to the 19th century described chronic lung infections and “dilated bronchi,” but bronchiectasis was not clearly defined until advances in radiology.
- Modern Recognition:
- The advent of high-resolution computed tomography (HRCT) in the late 20th century greatly enhanced the detection and characterization of bronchiectasis.
Who Discovered It?
- No single individual is credited with “discovering” bronchiectasis; its recognition evolved from cumulative clinical observations and improvements in imaging technology.
Major Discoveries and Breakthroughs:
- Radiologic Advancements:
- The introduction of HRCT enabled precise visualization of bronchial dilatation and wall thickening.
- Pathophysiological Insights:
- Understanding the role of chronic inflammation, infection, and impaired mucociliary clearance has been pivotal.
- Therapeutic Developments:
- Discoveries regarding airway clearance techniques, antibiotics, and anti-inflammatory strategies have transformed management.
Evolution of Medical Understanding Over Time:
- Initial management was largely symptomatic. Over decades, enhanced imaging, microbiological diagnostics, and a better understanding of inflammatory pathways have led to targeted treatments and multidisciplinary care approaches.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms:
- Persistent, chronic cough often productive of sputum.
- Occasional mild breathlessness, especially during exertion.
- Frequent respiratory infections.
- Advanced-Stage Symptoms:
- Worsening cough with large volumes of purulent or foul-smelling sputum.
- Severe shortness of breath, fatigue, and exercise intolerance.
- Recurrent pneumonia and hemoptysis (coughing up blood).
- Clubbing of the fingers may be observed.
Common vs. Rare Symptoms:
- Common:
- Chronic cough, daily sputum production, and frequent respiratory infections.
- Rare:
- Hemoptysis and significant weight loss occur less frequently but are markers of advanced disease.
How Symptoms Progress Over Time:
- Bronchiectasis typically begins with mild respiratory symptoms that gradually worsen as the structural damage to the airways becomes more pronounced.
- Without effective management, the disease may progress to chronic respiratory failure and severe systemic effects due to recurrent infections.
4. Causes
Biological and Environmental Causes:
- Biological Causes:
- Recurrent infections, inflammatory lung diseases (such as cystic fibrosis), and immune system disorders can cause persistent airway inflammation and damage.
- Environmental Causes:
- Exposure to pollutants, tobacco smoke, or harmful chemicals can exacerbate lung injury.
Genetic and Hereditary Factors:
- Genetic Disorders:
- Conditions like cystic fibrosis, primary ciliary dyskinesia, and alpha-1 antitrypsin deficiency predispose individuals to develop bronchiectasis.
Known Triggers or Exposure Risks:
- Triggers:
- Repeated respiratory infections, particularly in childhood, can lead to airway damage.
- Inadequate treatment of lung infections can also trigger bronchiectasis.
- Exposure Risks:
- Environmental pollutants and secondhand smoke increase the risk of chronic lung injury.
5. Risk Factors
Who is Most at Risk?
- Age:
- Both children (especially those with a history of severe respiratory infections) and older adults are at risk.
- Gender:
- There is no strong gender predisposition; however, certain underlying causes (e.g., cystic fibrosis) may show gender differences.
- Lifestyle:
- Individuals with a history of smoking or exposure to secondhand smoke.
- Medical History:
- People with chronic respiratory conditions (e.g., asthma, COPD) or genetic conditions affecting the lungs.
Environmental, Occupational, and Genetic Factors:
- Environmental:
- Exposure to air pollution and occupational inhalants.
- Occupational:
- Workers in industries with high exposure to dust and chemicals may have increased risk.
- Genetic:
- Inherited disorders that affect mucociliary clearance or lung structure increase susceptibility.
Impact of Pre-Existing Conditions:
- Pre-existing conditions such as recurrent pneumonia, cystic fibrosis, or immunodeficiencies significantly elevate the risk and severity of bronchiectasis.
6. Complications
What Complications Can Arise from Bronchiectasis?
- Respiratory Complications:
- Chronic respiratory failure due to progressive loss of lung function.
- Recurrent pneumonia and lung abscesses.
- Systemic Complications:
- Chronic inflammation may contribute to cardiovascular strain.
- Hemoptysis, in severe cases, can be life-threatening.
Long-Term Impact on Organs and Overall Health:
- Progressive lung damage can lead to irreversible respiratory impairment and reduced quality of life.
- The burden of frequent infections and systemic inflammation may impact overall organ function.
Potential Disability or Fatality Rates:
- Bronchiectasis is associated with significant morbidity, and severe cases can lead to high rates of disability.
- Mortality is primarily due to respiratory failure, complications from recurrent infections, and associated comorbidities.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Clinical Evaluation:
- Detailed medical history, including past respiratory infections and symptoms.
- Physical examination focusing on lung auscultation for crackles and wheezing.
- Imaging Studies:
- High-resolution computed tomography (HRCT) is the gold standard for diagnosing bronchiectasis.
- Laboratory Tests:
- Sputum cultures to identify causative organisms.
Medical Tests:
- Pulmonary Function Tests (PFTs):
- Assess lung function and airflow limitation.
- Bronchoscopy:
- May be used to evaluate airway anatomy and collect samples if indicated.
Early Detection Methods and Their Effectiveness:
- HRCT is highly effective for early detection of bronchial dilatation and parenchymal changes.
- Regular monitoring in high-risk individuals (e.g., those with cystic fibrosis or recurrent pneumonia) facilitates early diagnosis.
8. Treatment Options
Standard Treatment Protocols:
- Airway Clearance Techniques:
- Chest physiotherapy, postural drainage, and the use of devices to enhance mucus clearance.
- Antibiotic Therapy:
- Long-term or intermittent antibiotics may be used to manage chronic infections.
- Anti-Inflammatory Medications:
- Inhaled corticosteroids or other anti-inflammatory agents may be employed to reduce airway inflammation.
- Bronchodilators:
- Used to relieve airflow obstruction and improve breathing.
- Surgical Intervention:
- In localized cases refractory to medical therapy, surgical resection of the affected lung segment may be considered.
Emerging Treatments and Clinical Trials:
- Research is exploring the role of novel anti-inflammatory drugs, mucolytic agents, and immunomodulatory therapies.
- Clinical trials are evaluating the effectiveness of long-term macrolide therapy (e.g., azithromycin) for its anti-inflammatory and antimicrobial properties.
9. Prevention & Precautionary Measures
How Can Bronchiectasis Be Prevented?
- Early and Effective Treatment:
- Prompt treatment of respiratory infections and aggressive management of underlying conditions (e.g., cystic fibrosis) can reduce the risk of developing bronchiectasis.
- Vaccination:
- Immunizations against influenza and pneumococcus can help prevent infections that may precipitate bronchiectasis.
- Environmental Precautions:
- Avoidance of tobacco smoke and occupational exposure to irritants.
- Regular Monitoring:
- High-risk individuals should be monitored for early signs of chronic lung damage.
Lifestyle Changes and Environmental Precautions:
- Adopting a healthy lifestyle, including regular exercise and good respiratory hygiene, can help maintain lung health.
- Improving air quality in indoor and occupational settings is beneficial.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Prevalence varies widely depending on underlying conditions. For example, in cystic fibrosis populations, bronchiectasis is common.
- In the general adult population, the prevalence is lower but increasing recognition has led to more diagnoses.
Mortality and Survival Rates:
- Mortality is typically related to complications, especially respiratory failure and recurrent infections.
- Survival rates depend on disease severity, underlying causes, and access to effective treatments.
Country-Wise Comparison and Trends:
- Developed countries with advanced diagnostic capabilities report higher prevalence due to better detection.
- In regions with limited healthcare resources, underdiagnosis is common, and outcomes may be poorer due to delayed treatment.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Novel Therapies:
- Studies on anti-inflammatory and immunomodulatory agents to reduce chronic airway inflammation.
- Airway Clearance Innovations:
- Development of new devices and techniques to improve mucus clearance.
- Long-Term Antibiotic Regimens:
- Research on optimizing macrolide therapy to reduce exacerbations.
- Regenerative Medicine:
- Investigations into stem cell therapies and lung tissue regeneration hold promise for future treatment.
Ongoing Studies & Future Medical Possibilities:
- Clinical trials continue to evaluate combination therapies, personalized medicine approaches, and digital health tools for remote monitoring.
- Future research may further elucidate the genetic and molecular pathways involved in bronchiectasis, opening avenues for targeted interventions.
Potential Cures or Innovative Therapies Under Development:
- While there is no cure for bronchiectasis, emerging therapies aim to slow disease progression, reduce exacerbations, and improve quality of life.
- Innovative approaches, such as gene-targeted therapies, are under exploration but remain in early research stages.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Bronchiectasis:
- Bronchiectasis was once considered a rare condition but is now recognized as more common, particularly as a complication of other lung diseases.
- The term “bronchiectasis” comes from the Greek words “bronchos” (airway) and “ektasis” (dilation).
Myths vs. Medical Facts:
- Myth: Bronchiectasis is only caused by cystic fibrosis.
- Fact: Although cystic fibrosis is a well-known cause, bronchiectasis can result from a variety of conditions including recurrent infections, immune disorders, and chronic inflammatory diseases.
- Myth: It is a self-limiting disease.
- Fact: Bronchiectasis is typically a chronic, progressive condition that requires long-term management.
- Myth: Only smokers get bronchiectasis.
- Fact: While smoking can exacerbate lung damage, bronchiectasis can occur in non-smokers, particularly in patients with congenital or post-infectious lung conditions.
Impact on Specific Populations or Professions:
- High-Risk Populations:
- Patients with cystic fibrosis, immune deficiencies, or a history of severe pneumonia.
- Healthcare Providers:
- Pulmonologists, respiratory therapists, and primary care physicians are crucial in managing bronchiectasis.
- Public Health:
- Increased awareness and early intervention strategies are essential to reduce exacerbations and improve long-term outcomes, thereby lessening the overall disease burden.
References
The content in this report is synthesized from peer-reviewed scientific literature, clinical guidelines from organizations such as the American Thoracic Society (ATS) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD), and epidemiological studies available via reputable databases (e.g., PubMed).
Conclusion:
Bronchiectasis is a chronic lung condition characterized by permanent dilation of the bronchi, often resulting from recurrent infections or chronic inflammation. Early detection, effective management through airway clearance, targeted antibiotics, and supportive therapies are critical to mitigating its impact. Advances in treatment and ongoing research continue to improve patient outcomes and quality of life, making early intervention and comprehensive care essential in managing this condition.