Gastroparesis
Below is a comprehensive, structured report on Gastroparesis that covers its clinical definition, historical evolution, symptomatology, causes, risk factors, complications, diagnostic and treatment options, prevention measures, global statistics, recent research, and interesting insights. This report is intended to serve as an in‐depth resource for both the general public and medical professionals.
1. Overview
What is Gastroparesis?
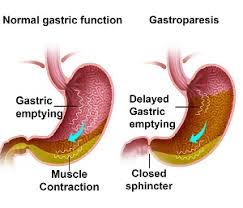
Gastroparesis is a chronic disorder of gastric motility characterized by delayed emptying of stomach contents in the absence of any mechanical obstruction. This impaired motility results from abnormalities in the nerves, muscles, or the interstitial cells of Cajal (the pacemaker cells of the gastrointestinal tract).
Definition & Affected Body Parts/Organs:
- Definition: Gastroparesis is defined as delayed gastric emptying with symptoms such as nausea, vomiting, early satiety, bloating, and upper abdominal pain.
- Affected Organs:
- Stomach: The primary organ affected, with its muscular contractions (peristalsis) compromised.
- Upper Gastrointestinal Tract: Indirectly impacts the esophagus and small intestine due to altered digestion.
Prevalence & Significance:
- Prevalence: Although considered relatively uncommon, gastroparesis is most frequently observed in individuals with long-standing diabetes, but it also occurs idiopathically and post-surgically. Estimates vary, with studies suggesting a prevalence of 0.2–5% in the general population.
- Significance: Gastroparesis can lead to significant morbidity, including nutritional deficiencies, poor glycemic control in diabetics, and a marked reduction in quality of life. It also poses a burden on healthcare systems due to recurrent hospitalizations and chronic management needs.
2. History & Discoveries
When and How Was Gastroparesis First Identified?
- Early clinical descriptions of symptoms consistent with gastroparesis date back many decades, with initial recognition largely among diabetic patients experiencing unexplained nausea and vomiting.
- The term “gastroparesis” (meaning “stomach paralysis”) emerged as clinicians observed delayed gastric emptying without physical blockage.
Who Discovered It?
- Rather than being attributed to a single discoverer, the understanding of gastroparesis evolved gradually through the collective clinical observations of physicians managing diabetic complications and post-surgical patients.
Major Discoveries & Breakthroughs:
- Diagnostic Imaging: The development of gastric emptying scintigraphy in the 1980s revolutionized diagnosis by objectively measuring the rate of gastric emptying.
- Understanding Neuromuscular Dysfunction: Research into the roles of the vagus nerve and interstitial cells of Cajal has deepened insight into the pathophysiology of gastroparesis.
- Advances in Treatment: The identification of effective prokinetic agents (e.g., metoclopramide) and antiemetics has helped shape modern therapeutic approaches.
Evolution of Medical Understanding:
- Over time, medical understanding has shifted from viewing gastroparesis solely as a complication of diabetes to recognizing its multifactorial etiology—including idiopathic forms, post-surgical changes, and drug-induced cases—which has influenced diagnostic and treatment strategies.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms:
- Early Symptoms:
- Mild nausea and occasional vomiting
- Early satiety (feeling full quickly)
- Bloating and discomfort after eating
- Advanced-Stage Symptoms:
- Frequent, severe nausea and vomiting (which may lead to dehydration)
- Significant weight loss and malnutrition
- Persistent upper abdominal pain and bloating
- Fluctuating blood sugar levels, particularly in diabetic patients
Common vs. Rare Symptoms:
- Common Symptoms:
- Nausea, vomiting, early satiety, bloating, and abdominal pain are frequently reported.
- Rare Symptoms:
- In some cases, patients may experience erratic glycemic control, anemia, or even bezoar formation (hardened food masses) due to prolonged retention of food.
Progression Over Time:
- Gastroparesis symptoms often worsen gradually. Early manifestations may be intermittent, but without effective management, they can progress to chronic, debilitating symptoms that significantly impact nutritional status and overall quality of life.
4. Causes
Biological and Environmental Causes:
- Diabetic Neuropathy: Long-standing diabetes is the most common cause; chronic high blood sugar damages the vagus nerve, which controls stomach muscles.
- Post-Surgical Changes: Surgeries involving the stomach or vagus nerve (e.g., fundoplication or bariatric procedures) may lead to gastroparesis.
- Medication-Induced: Certain medications, such as opioids, anticholinergics, and some antidepressants, can slow gastric motility.
- Idiopathic Causes: In many cases, no specific cause is identified despite thorough evaluation.
Genetic and Hereditary Factors:
- While a direct genetic cause is not well established, genetic predispositions may influence susceptibility to nerve and muscle dysfunction, thereby contributing to the risk.
Known Triggers or Exposure Risks:
- Metabolic Triggers: Poor glycemic control in diabetes can exacerbate or trigger gastroparesis.
- Infections: Rarely, viral infections have been implicated in the development of idiopathic gastroparesis.
- Lifestyle Factors: Dietary habits, stress, and certain medications can serve as triggers or aggravate existing conditions.
5. Risk Factors
Who is Most at Risk?
- Diabetics: Particularly those with type 1 or long-standing type 2 diabetes.
- Post-Surgical Patients: Individuals who have undergone gastric or vagal nerve surgeries.
- Gender & Age: Although gastroparesis can occur in any demographic, studies have noted a higher prevalence among women.
- Other Conditions: Patients with connective tissue disorders (e.g., scleroderma) or neurological diseases are also at increased risk.
Environmental, Occupational, and Genetic Factors:
- Environmental: Lifestyle factors like diet, stress, and exposure to certain medications can contribute.
- Occupational: Although not a direct risk factor, occupations that involve high stress or irregular eating patterns may indirectly impact disease development.
- Genetic: A family history of diabetes or gastrointestinal motility disorders might elevate risk.
Impact of Pre-Existing Conditions:
- Chronic conditions such as diabetes, hypothyroidism, and autoimmune diseases can predispose individuals to gastroparesis by affecting nerve function and gastric muscle activity.
6. Complications
Potential Complications Arising from Gastroparesis:
- Nutritional Deficiencies: Prolonged delayed emptying can lead to malnutrition, vitamin deficiencies, and unintended weight loss.
- Dehydration and Electrolyte Imbalances: Frequent vomiting increases the risk of dehydration and disturbances in electrolyte balance.
- Poor Glycemic Control: In diabetic patients, erratic gastric emptying can lead to significant fluctuations in blood sugar levels.
- Bezoar Formation: The stagnation of food can sometimes lead to the formation of bezoars, which may require endoscopic or surgical removal.
Long-Term Impact on Organs and Overall Health:
- Over time, chronic gastroparesis can result in impaired absorption of nutrients, worsening of diabetes control, and a decline in overall quality of life.
Potential Disability or Fatality Rates:
- While gastroparesis itself is rarely directly fatal, its complications can contribute to significant morbidity and, in severe cases, may necessitate repeated hospitalizations and intensive management.
7. Diagnosis & Testing
Common Diagnostic Procedures:
- Gastric Emptying Scintigraphy: The gold standard diagnostic test that measures the rate of gastric emptying using a radiolabeled meal.
- Breath Tests: The 13C-octanoic acid breath test is an alternative non-invasive method for assessing gastric emptying.
- Upper Endoscopy: Used primarily to exclude mechanical obstruction and assess mucosal health.
Medical Tests:
- Blood Tests: To evaluate electrolyte levels, nutritional status, and glycemic control.
- Ultrasound or CT Scan: Occasionally employed to rule out other abdominal pathologies.
Early Detection Methods and Their Effectiveness:
- Early detection is achieved through a combination of patient history, symptom assessment, and objective testing (such as scintigraphy). Prompt diagnosis allows for earlier intervention, which can help mitigate nutritional and metabolic complications.
8. Treatment Options
Standard Treatment Protocols:
- Dietary Modifications:
- Small, frequent meals that are low in fat and fiber to facilitate easier digestion.
- Liquid or pureed diets may be recommended during severe flare-ups.
- Medications:
- Prokinetic Agents: Such as metoclopramide and erythromycin to enhance gastric motility.
- Antiemetics: To control nausea and vomiting.
- Ghrelin Agonists: Emerging treatments that have shown promise in accelerating gastric emptying.
- Nutritional Support:
- Supplements or enteral feeding may be necessary for patients with significant malnutrition.
Surgical and Interventional Therapies:
- Gastric Electrical Stimulation (GES): A device implanted to help regulate stomach contractions in refractory cases.
- Endoscopic and Surgical Interventions: Procedures like pyloroplasty or endoscopic pyloromyotomy are considered for severe, medically refractory gastroparesis.
Emerging Treatments & Clinical Trials:
- Novel agents including new prokinetic drugs and ghrelin analogs are under investigation.
- Research into regenerative therapies and minimally invasive interventions (e.g., endoscopic techniques) is ongoing to improve long-term outcomes.
9. Prevention & Precautionary Measures
Prevention Strategies:
- Management of Underlying Conditions:
- Strict glycemic control in diabetic patients and careful management of other chronic diseases can reduce the risk of developing gastroparesis.
- Medication Review:
- Avoiding or carefully monitoring medications known to slow gastric motility may help prevent symptom onset.
- Lifestyle Modifications:
- A balanced diet, regular physical activity, and stress reduction are recommended to support overall gastrointestinal health.
Preventive Screenings:
- There are no vaccines for gastroparesis; however, routine screening for gastrointestinal symptoms in high-risk populations (e.g., diabetics) allows for earlier detection and management.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Gastroparesis is estimated to affect a small but significant proportion of the population, with higher prevalence observed in diabetic patients.
- Prevalence figures vary by region, with some studies suggesting up to 5% in high-risk groups, though overall population prevalence remains low.
Mortality and Survival Rates:
- Gastroparesis is not typically directly fatal; however, its complications—particularly malnutrition and poor glycemic control in diabetics—can contribute to increased morbidity.
- The long-term impact on quality of life and healthcare utilization is considerable.
Country-Wise Comparison and Trends:
- Developed countries with higher rates of diabetes tend to report more cases of gastroparesis.
- In resource-limited settings, underdiagnosis remains a challenge, potentially skewing true prevalence data.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Pharmacological Innovations:
- The development of new prokinetic agents and ghrelin agonists is underway to offer improved symptom control.
- Device-Based Therapies:
- Advances in gastric electrical stimulation have provided a novel treatment option for refractory cases.
- Diagnostic Improvements:
- Enhanced imaging and non-invasive testing methods (e.g., advanced breath tests) are being refined for earlier and more accurate diagnosis.
Ongoing Studies & Future Possibilities:
- Current clinical trials are evaluating the efficacy and safety of emerging therapies, including minimally invasive endoscopic interventions.
- Future research is focusing on personalized treatment approaches based on patient-specific factors, including genetic and metabolic profiles.
Potential Cures or Innovative Therapies:
- While a definitive cure for gastroparesis is not yet available, regenerative medicine, stem cell therapies, and novel neuromodulation techniques hold promise for reversing gastric dysmotility.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge about Gastroparesis:
- The term “gastroparesis” literally means “stomach paralysis,” though most patients experience partial rather than complete loss of motility.
- Gastroparesis was historically underdiagnosed because its symptoms overlap with other gastrointestinal disorders, leading to delayed treatment.
Myths and Misconceptions vs. Medical Facts:
- Myth: Gastroparesis only affects diabetics.
Fact: Although diabetes is a major risk factor, idiopathic and post-surgical gastroparesis also account for a significant number of cases. - Myth: All patients with gastroparesis experience severe vomiting.
Fact: Symptoms vary widely; some patients may primarily experience early satiety and bloating with minimal vomiting.
Impact on Specific Populations or Professions:
- Gender Differences: Studies indicate that women are more frequently diagnosed with gastroparesis, though the reasons for this disparity are not fully understood.
- Quality of Life: Gastroparesis can have a profound impact on daily activities, employment, and overall mental health, particularly in individuals with chronic conditions like diabetes.
References
The information in this report is synthesized from peer-reviewed medical literature, clinical guidelines from organizations such as the American Gastroenterological Association (AGA), and recent epidemiological studies. For further details, readers are encouraged to consult reputable sources including PubMed, clinical trials databases, and specialty society publications.
This detailed report on gastroparesis provides a thorough overview—from its definition and pathophysiology to historical insights, symptom progression, diagnostic strategies, treatment options, and ongoing research. By understanding these aspects, healthcare providers can better tailor interventions, and patients can gain clearer insights into managing this challenging condition.