Pulmonary Hypertension
Below is a comprehensive, structured report on Pulmonary Hypertension. This report covers all essential aspects—from an overview and historical context to symptoms, causes, risk factors, complications, diagnosis, treatment, prevention, global statistics, recent research, and interesting insights. The information is based on current clinical guidelines and recent research to serve as an informative resource for both the general public and medical professionals.
1. Overview
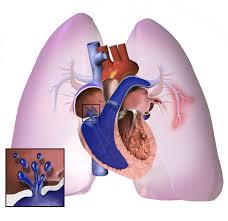
What is Pulmonary Hypertension?
Pulmonary hypertension (PH) is a condition characterized by abnormally high blood pressure in the pulmonary arteries—the vessels that transport blood from the heart to the lungs. This increased pressure places an extra burden on the right side of the heart.
Definition & Affected Body Parts/Organs
- Definition: PH is defined by a mean pulmonary arterial pressure (mPAP) of ≥25 mmHg at rest, measured via right heart catheterization. It is classified into several groups based on its underlying cause (e.g., pulmonary arterial hypertension, PH due to left heart disease, PH due to lung diseases, and chronic thromboembolic pulmonary hypertension).
- Affected Organs: The primary affected organs are the pulmonary arteries and the right ventricle of the heart. Over time, increased pulmonary pressures can lead to right ventricular hypertrophy and eventual right heart failure.
Prevalence and Significance of the Disease
- Prevalence: PH is relatively rare, with pulmonary arterial hypertension (Group 1) affecting about 15–50 cases per million people, though overall PH prevalence is higher when including other groups.
- Significance: PH is a serious and progressive condition associated with high morbidity and mortality. Early recognition and targeted treatment are crucial to improving survival and quality of life.
2. History & Discoveries
When and How Was Pulmonary Hypertension First Identified?
- Early Identification: Early descriptions of elevated pulmonary pressures emerged in the mid-20th century, although the clinical syndrome was recognized later as diagnostic techniques evolved.
Who Discovered It?
- Historical Contributions: While no single individual is solely credited with “discovering” PH, early pioneers in cardiology and pulmonology, such as Dr. Paul Wood and others in the 1950s and 1960s, helped characterize the hemodynamic abnormalities of PH.
Major Discoveries and Breakthroughs
- Hemodynamic Measurements: The development of right heart catheterization provided the means to measure pulmonary pressures accurately.
- Classification Systems: Over the decades, evolving classification systems (such as the World Health Organization’s classification) have improved our understanding of the different types of PH.
- Therapeutic Advances: The introduction of targeted therapies—such as prostacyclin analogues, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors—in the late 20th and early 21st centuries marked major breakthroughs.
Evolution of Medical Understanding Over Time
- The understanding of PH has evolved from viewing it as a uniform condition to recognizing its diverse etiologies. Improved diagnostic modalities and molecular insights have led to personalized treatment strategies for different PH subtypes.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Shortness of breath during exertion (dyspnea on exertion)
- Fatigue and reduced exercise tolerance
- Mild chest discomfort
- Occasionally, light-headedness or syncope (fainting)
- Advanced-Stage Symptoms:
- Severe dyspnea even at rest
- Increased fatigue and weakness
- Swelling in the ankles and legs (peripheral edema)
- Chest pain and palpitations
- Signs of right heart failure, such as ascites and liver congestion
Common vs. Rare Symptoms
- Common:
- Exertional dyspnea, fatigue, and peripheral edema are frequently reported.
- Rare:
- Some patients may experience cyanosis (bluish skin) or severe syncope, particularly if arrhythmias occur.
How Symptoms Progress Over Time
- PH often starts with subtle symptoms that are easily attributed to aging or deconditioning. As pulmonary pressures increase, symptoms become more pronounced, eventually leading to significant functional limitations and signs of right heart failure.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- In Group 1 (pulmonary arterial hypertension), the underlying cause often involves endothelial dysfunction, smooth muscle proliferation, and vascular remodeling.
- In other groups, PH may result from left heart disease, chronic lung diseases, or chronic thromboembolic events.
- Environmental Causes:
- Exposure to toxins (e.g., certain drugs, appetite suppressants) has been linked to PH.
- Chronic hypoxia from lung diseases also contributes.
Genetic and Hereditary Factors
- Genetic Predisposition:
- Mutations in genes such as BMPR2 (bone morphogenetic protein receptor type II) are found in many cases of familial pulmonary arterial hypertension.
- Hereditary Influences:
- A family history of PH increases the likelihood of developing the condition.
Any Known Triggers or Exposure Risks
- Triggers:
- Certain medications, high-altitude exposure, and chronic lung infections can trigger or worsen PH in susceptible individuals.
5. Risk Factors
Who Is Most at Risk?
- Age:
- PH can occur at any age but is more common in middle-aged adults.
- Gender:
- There is a slight female predominance in certain types of PH, particularly pulmonary arterial hypertension.
- Occupation and Lifestyle:
- Occupations involving high-altitude work or exposure to environmental toxins may have a higher risk.
- Pre-existing Conditions:
- Individuals with chronic lung diseases, left heart disease, or a history of thromboembolic events are at increased risk.
Environmental, Occupational, and Genetic Factors
- Environmental/Occupational:
- Exposure to drugs or toxins that damage the pulmonary vasculature.
- Genetic:
- Family history and genetic mutations (e.g., BMPR2) are significant risk factors.
Impact of Pre-Existing Conditions
- Pre-existing conditions such as chronic obstructive pulmonary disease (COPD), heart failure, and connective tissue diseases significantly elevate the risk of developing PH.
6. Complications
What Complications Can Arise from Pulmonary Hypertension?
- Cardiac Complications:
- Right ventricular hypertrophy and eventual right heart failure.
- Arrhythmias, which can further compromise cardiac output.
- Systemic Complications:
- Reduced oxygenation can lead to multi-organ dysfunction.
- Severe cases can result in syncope, shock, and sudden cardiac death.
Long-Term Impact on Organs and Overall Health
- Progressive PH leads to chronic strain on the heart and other organs, causing diminished quality of life and increased morbidity.
Potential Disability or Fatality Rates
- PH, particularly when advanced, is associated with high mortality. Survival rates vary by PH subtype, but overall, PH significantly increases the risk of fatal cardiac events.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
- Detailed medical history and physical examination, noting symptoms like dyspnea, fatigue, and signs of right heart failure.
- Medical Tests:
- Echocardiography: The primary non-invasive test to estimate pulmonary artery pressures and assess right ventricular function.
- Right Heart Catheterization: The gold standard for diagnosing PH by directly measuring pulmonary arterial pressure.
- Electrocardiogram (ECG): May show signs of right ventricular strain.
- Imaging:
- Chest X-ray, CT, or MRI can assess lung parenchyma and rule out other causes.
- Laboratory Tests:
- Blood tests including BNP or NT-proBNP to evaluate cardiac stress.
Early Detection Methods and Their Effectiveness
- Early detection is critical. Screening high-risk populations (e.g., patients with COPD or left heart disease) with echocardiography can lead to earlier diagnosis and intervention.
8. Treatment Options
Standard Treatment Protocols
- Medications:
- Vasodilators: Such as prostacyclin analogues, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors help reduce pulmonary artery pressure.
- Diuretics: To manage fluid overload and reduce symptoms of right heart failure.
- Anticoagulants: May be used in cases associated with thromboembolic PH.
- Supportive Therapies:
- Oxygen therapy to improve tissue oxygenation.
- Lifestyle modifications, including exercise programs and dietary adjustments.
- Advanced Therapies:
- In severe cases, lung transplantation may be considered.
Emerging Treatments and Clinical Trials
- Ongoing research is evaluating new pharmacologic agents targeting different pathways (e.g., soluble guanylate cyclase stimulators) and novel combination therapies.
- Clinical trials are exploring gene-based and regenerative therapies aimed at improving pulmonary vascular remodeling.
9. Prevention & Precautionary Measures
How Can Pulmonary Hypertension Be Prevented?
- Primary Prevention:
- Preventing or effectively managing conditions that lead to PH, such as COPD, left heart disease, and chronic thromboembolism.
- Lifestyle Changes and Environmental Precautions:
- Smoking cessation, regular exercise, and a healthy diet are critical.
- Avoiding exposure to known environmental toxins and managing high-altitude exposures in susceptible individuals.
- Preventive Screenings:
- Routine cardiac evaluations for individuals with known risk factors.
- Vaccines (if applicable):
- While no vaccines directly prevent PH, immunizations (e.g., influenza, pneumococcal) can prevent respiratory infections that may exacerbate underlying conditions.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally:
- Global Trends:
- The prevalence of PH varies by etiology. For instance, pulmonary arterial hypertension (Group 1) is estimated at 15–50 cases per million, while PH secondary to left heart or lung diseases is more common.
- Regional Variations:
- Developed countries with comprehensive diagnostic facilities report higher prevalence due to better detection. In contrast, developing regions may have underdiagnosis.
Mortality and Survival Rates:
- Outcomes:
- Mortality remains high in advanced PH, with survival rates significantly dependent on the underlying cause and timely treatment.
- Country-Wise Comparisons and Trends:
- Countries with advanced healthcare systems and specialized PH centers generally report better outcomes compared to regions with limited resources.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research:
- Targeted Therapies:
- Recent advances in prostacyclin analogues, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors have improved outcomes.
- Molecular Research:
- Studies focusing on the molecular pathways of vascular remodeling and inflammation are paving the way for novel therapies.
- Clinical Trials:
- Numerous clinical trials are ongoing to test new agents and combination therapies aimed at further reducing pulmonary pressures and improving right ventricular function.
- Personalized Medicine:
- Integration of genetic and biomarker data is expected to enhance risk stratification and treatment personalization in PH.
Ongoing Studies and Future Medical Possibilities:
- Research into regenerative therapies, including stem cell applications and gene therapy, may offer future breakthroughs.
- Advances in imaging and remote monitoring are enhancing early detection and long-term management.
Potential Cures or Innovative Therapies Under Development:
- While a definitive cure for PH remains elusive, innovative therapies targeting the underlying pathophysiological mechanisms hold promise for the future.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge and Myths:
- Myths vs. Medical Facts:
- Myth: Pulmonary hypertension is solely a disease of older adults.
- Fact: Although PH is more common in older individuals, certain forms (e.g., idiopathic pulmonary arterial hypertension) can affect younger patients, particularly women.
- Lesser-Known Insights:
- PH often goes undiagnosed in its early stages due to nonspecific symptoms, emphasizing the importance of screening high-risk populations.
- The development of advanced imaging techniques (e.g., cardiac MRI and CT angiography) has significantly improved the diagnosis and management of PH.
- Multidisciplinary care, involving cardiologists, pulmonologists, and specialized PH centers, is critical for optimal patient outcomes.
- Ongoing research into the genetic basis of PH is helping to identify individuals at risk before significant symptoms develop.
- Public awareness initiatives and support groups play a vital role in improving the quality of life for patients with PH.
References
- – Global health data and guidelines on pulmonary hypertension.
- – Provides detailed information on the diagnosis, management, and treatment of PH.
- – Resources on pulmonary vascular diseases, including PH.
- – Recent studies on emerging therapies and the molecular basis of pulmonary hypertension.
This detailed report on pulmonary hypertension integrates historical context, clinical features, and emerging research to provide a comprehensive resource. Emphasis on early detection, targeted treatment strategies, and ongoing innovations in therapy highlights the multifaceted approach required to manage PH and improve outcomes for affected individuals.