Heart Failure Symptoms
Below is a comprehensive, structured report on Heart Failure Symptoms. This document covers every essential aspect—from an overview of what heart failure symptoms are and their historical context to detailed discussions on clinical manifestations, causes, risk factors, complications, diagnosis, treatment, prevention, global statistics, recent research, and interesting facts. The information is based on current clinical guidelines, research studies, and authoritative sources to serve as a resource for both the general public and healthcare professionals.
1. Overview
What Are Heart Failure Symptoms?
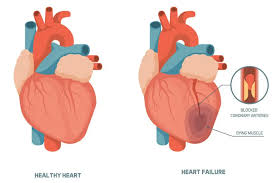
Heart failure symptoms refer to the clinical signs and manifestations that occur when the heart is unable to pump blood effectively, leading to inadequate perfusion of tissues and fluid buildup in various organs.
Definition & Affected Body Parts/Organs
- Definition: Heart failure is a chronic condition in which the heart’s pumping function is impaired, causing a cascade of symptoms such as shortness of breath, fatigue, and fluid retention. These symptoms reflect the inability of the heart to meet the body’s circulatory demands.
- Affected Organs: While the primary defect lies within the heart, heart failure affects multiple organ systems. The lungs (due to pulmonary congestion), kidneys (from decreased perfusion), liver (congestion), and peripheral tissues (leading to edema) are frequently impacted.
Prevalence and Significance of the Disease
- Prevalence: Heart failure is a leading cause of morbidity and mortality worldwide, particularly among older adults. It affects millions globally, with increasing prevalence due to an aging population and improved survival rates following acute cardiac events.
- Significance: The high hospitalization rates, reduced quality of life, and significant economic burden associated with heart failure make it a critical public health challenge. Early detection and management of symptoms are essential to improve outcomes.
2. History & Discoveries
When and How Were Heart Failure Symptoms First Identified?
- Early Recognition: Descriptions of heart failure symptoms date back centuries, though early clinicians did not have the diagnostic tools available today. Historical medical texts described symptoms such as breathlessness, fatigue, and edema.
- Modern Era: In the 19th century, improved clinical observations and autopsy studies helped clarify the concept of heart failure as a distinct clinical syndrome.
Who Discovered It?
- Collective Contributions: No single individual is credited with the discovery of heart failure symptoms. Instead, a series of contributions by pioneering physicians—such as William Harvey, who described the circulatory system, and later clinicians who detailed signs of congestion—laid the foundation for our current understanding.
Major Discoveries and Breakthroughs
- Diagnostic Advances: The invention of the stethoscope and later developments in imaging (e.g., chest X-ray, echocardiography) significantly improved the diagnosis of heart failure.
- Therapeutic Milestones: Discoveries such as the beneficial effects of diuretics, ACE inhibitors, beta-blockers, and device therapies (ICDs and CRT) have transformed the management of heart failure.
Evolution of Medical Understanding Over Time
- The understanding of heart failure has evolved from a terminal diagnosis to a manageable chronic condition. This evolution is marked by improved pathophysiological insights, the development of evidence-based therapies, and the emergence of personalized treatment strategies.
3. Symptoms
Early Symptoms vs. Advanced-Stage Symptoms
- Early Symptoms:
- Dyspnea on Exertion: Shortness of breath during physical activity.
- Fatigue: Reduced exercise tolerance and chronic tiredness.
- Mild Peripheral Edema: Subtle swelling in the lower extremities.
- Advanced-Stage Symptoms:
- Orthopnea and Paroxysmal Nocturnal Dyspnea: Severe breathlessness when lying flat and waking up at night gasping for air.
- Pulmonary Congestion: Rales (crackles) on lung auscultation due to fluid in the lungs.
- Severe Edema and Weight Gain: Marked fluid retention leading to significant swelling in the legs, abdomen, and other tissues.
- Persistent Cough: Sometimes with frothy or blood-tinged sputum.
Common vs. Rare Symptoms
- Common Symptoms:
- Shortness of breath, fatigue, and peripheral edema are among the most frequently reported.
- Rare Symptoms:
- Symptoms such as sudden syncope (fainting) or severe palpitations may occur in some patients and indicate an associated arrhythmia or acute decompensation.
How Symptoms Progress Over Time
- Heart failure typically follows a gradual progression. Early symptoms may be intermittent and easily overlooked but tend to worsen as the condition advances. Without effective management, the patient may experience frequent hospitalizations and a substantial decline in quality of life.
4. Causes
Biological and Environmental Causes
- Biological Causes:
- Ischemic Heart Disease: Reduced blood flow from coronary artery disease is the leading cause.
- Hypertension: Chronic high blood pressure increases the heart’s workload, eventually leading to failure.
- Cardiomyopathies: Diseases of the heart muscle (dilated, hypertrophic, or restrictive) impair contractility.
- Environmental Causes:
- Lifestyle factors such as a sedentary lifestyle, poor diet, and excessive alcohol consumption contribute to the development of heart failure.
Genetic and Hereditary Factors
- Genetic Predisposition: Inherited conditions such as familial dilated cardiomyopathy can predispose individuals to heart failure.
- Hereditary Influences: A family history of heart disease is a significant risk factor, often interacting with lifestyle and environmental factors.
Any Known Triggers or Exposure Risks
- Triggers:
- Acute events such as myocardial infarction or severe arrhythmias can precipitate heart failure.
- Exposure to cardiotoxic substances (e.g., certain chemotherapy agents) can also trigger the development of heart failure symptoms.
5. Risk Factors
Who Is Most at Risk?
- Age: Incidence increases significantly with age, especially in individuals over 65.
- Gender: Both men and women are affected, though the underlying causes and presentation may vary.
- Occupation and Lifestyle: Sedentary lifestyle, obesity, and chronic stress are key risk factors.
Environmental, Occupational, and Genetic Factors
- Environmental/Occupational:
- Exposure to environmental toxins and chronic stress may contribute to heart failure development.
- Genetic Factors:
- Family history of heart disease, genetic mutations, and inherited cardiomyopathies increase risk.
Impact of Pre-Existing Conditions
- Comorbidities:
- Conditions such as diabetes, chronic kidney disease, and hypertension significantly increase the risk of heart failure and worsen the prognosis.
6. Complications
What Complications Can Arise from Heart Failure Symptoms?
- Organ Dysfunction:
- Pulmonary Edema: Fluid accumulation in the lungs impairs gas exchange.
- Renal Dysfunction: Reduced cardiac output can lead to kidney failure.
- Hepatic Congestion: Chronic right-sided heart failure can cause liver dysfunction.
- Arrhythmias:
- Heart failure predisposes patients to dangerous arrhythmias, including atrial fibrillation and ventricular tachycardia.
- Thromboembolism:
- Reduced mobility and altered blood flow increase the risk of blood clots, potentially leading to stroke.
Long-Term Impact on Organs and Overall Health
- Persistent heart failure can lead to progressive deterioration in organ function, significantly impairing quality of life and increasing the risk of multi-organ failure.
Potential Disability or Fatality Rates
- Heart failure is a major cause of hospitalization and is associated with high mortality rates. Advanced heart failure often results in significant disability and a reduced life expectancy, particularly if not managed optimally.
7. Diagnosis & Testing
Common Diagnostic Procedures
- Clinical Evaluation:
- Detailed patient history and physical examination, focusing on signs of fluid overload and reduced cardiac output.
- Medical Tests:
- Blood Tests: Measurement of biomarkers such as B-type natriuretic peptide (BNP) or NT-proBNP to assess the severity of heart failure.
- Imaging:
- Echocardiography: Essential for assessing cardiac structure, function, and ejection fraction.
- Chest X-ray: Useful for identifying pulmonary congestion and cardiomegaly.
- Cardiac MRI: Provides detailed imaging of myocardial structure and function.
- Electrocardiogram (ECG): Detects arrhythmias, prior myocardial infarctions, and other cardiac abnormalities.
Early Detection Methods and Their Effectiveness
- Early detection using biomarker screening and imaging modalities is crucial. Screening in high-risk populations (e.g., patients with hypertension or diabetes) can lead to timely intervention and improved outcomes.
8. Treatment Options
Standard Treatment Protocols
- Medications:
- Diuretics: Reduce fluid overload and relieve symptoms of congestion.
- ACE Inhibitors/ARBs: Lower blood pressure and reduce cardiac remodeling.
- Beta-Blockers: Improve cardiac function and reduce the risk of arrhythmias.
- Aldosterone Antagonists: Help manage fluid retention and improve survival.
- Device Therapies:
- Implantable Cardioverter-Defibrillators (ICDs): Prevent sudden cardiac death by treating life-threatening arrhythmias.
- Cardiac Resynchronization Therapy (CRT): Improves cardiac efficiency in patients with ventricular dyssynchrony.
- Surgical Interventions:
- In selected patients, surgical options such as coronary artery bypass grafting (CABG) or valve repair/replacement may be indicated.
Emerging Treatments and Clinical Trials
- Innovative Therapies:
- Research is ongoing into stem cell therapy, gene therapy, and novel pharmacologic agents targeting the neurohormonal pathways involved in heart failure.
- Personalized Medicine:
- Advances in genetic and biomarker profiling are paving the way for individualized treatment plans aimed at optimizing therapeutic outcomes.
9. Prevention & Precautionary Measures
How Can Heart Failure Symptoms Be Prevented?
- Lifestyle Changes:
- Adoption of a heart-healthy diet, regular physical activity, and weight management.
- Smoking cessation and moderation of alcohol consumption are crucial.
- Environmental Precautions:
- Reducing exposure to pollutants and managing stress can contribute to cardiovascular health.
Vaccines or Preventive Screenings
- While there are no vaccines for heart failure, routine screenings for hypertension, diabetes, and cholesterol levels—as well as regular cardiac evaluations—are essential for early detection and prevention.
10. Global & Regional Statistics
Incidence and Prevalence Rates Globally
- Global Trends: Heart failure is a leading cause of hospitalization and mortality worldwide, affecting millions of individuals, particularly in aging populations.
- Regional Variations:
- Developed countries with advanced healthcare systems tend to have better management and lower rates of severe heart failure, whereas developing regions face higher morbidity due to limited access to care.
Mortality and Survival Rates
- Outcomes: Despite advances in treatment, heart failure continues to have high mortality rates, particularly in advanced stages. Early intervention and proper management have been shown to improve survival and quality of life.
- Quality of Life: Effective treatment and rehabilitation programs can help patients manage symptoms and improve daily functioning.
Country-Wise Comparisons and Trends
- Countries with established preventive health programs and advanced medical care generally report lower rates of severe heart failure and better patient outcomes compared to regions with limited healthcare access.
11. Recent Research & Future Prospects
Latest Advancements in Treatment and Research
- New Pharmacologic Agents: Recent studies focus on drugs that more specifically target the molecular pathways of heart failure, aiming to improve cardiac remodeling and reduce hospitalizations.
- Device Improvements: Enhancements in ICDs, CRT, and remote monitoring technologies have further improved patient management and early detection of decompensation.
- Biomarker Discovery: Advances in biomarker research are enabling more precise risk stratification and personalized treatment strategies.
Ongoing Studies and Future Medical Possibilities
- Clinical Trials: Numerous trials are currently investigating novel therapies, including regenerative treatments such as stem cell therapy and gene therapy approaches, to restore cardiac function.
- Personalized Medicine: Ongoing research into genetic and proteomic profiling promises to tailor treatments more effectively, potentially revolutionizing heart failure management.
Potential Cures or Innovative Therapies Under Development
- Although a definitive cure for heart failure remains elusive, innovative therapies targeting myocardial regeneration and reverse remodeling are under investigation, offering hope for more effective long-term management.
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge and Myths
- Myths vs. Medical Facts:
- Myth: Heart failure is an inevitable part of aging.
- Fact: While age is a significant risk factor, heart failure is largely preventable and manageable with proper lifestyle modifications and early treatment.
- Lesser-Known Insights:
- Early heart failure may present with very subtle symptoms that are often mistaken for normal aging or deconditioning.
- Advances in telemedicine and remote monitoring have greatly enhanced the ability to manage heart failure symptoms before they lead to acute decompensation.
- Small improvements in diet (e.g., reducing salt intake) and physical activity can have a significant impact on delaying the progression of heart failure.
- The concept of “reverse remodeling” is a key focus in modern heart failure research, aiming to restore heart structure and function through targeted therapies.
References
- – Clinical guidelines, statistics, and management strategies for heart failure.
- – Research updates and clinical trial data on heart failure and its underlying mechanisms.
- – Global health statistics and trends related to cardiovascular diseases.
- – Recent studies on heart failure diagnostics, treatment advances, and emerging research.
This detailed report on heart failure symptoms is intended as a comprehensive resource that integrates historical perspectives with current clinical evidence and emerging research. The emphasis on early detection, risk management, and individualized treatment strategies underscores the critical importance of addressing heart failure to improve patient outcomes and quality of life.