Chronic obstructive pulmonary disease (COPD) is one of the leading causes of morbidity and mortality worldwide, affecting millions of people and placing an enormous burden on healthcare systems. In this comprehensive guide, we delve deep into the copd etiology and pathophysiology—unraveling the complex interplay between genetic predisposition, environmental exposures, immune responses, and molecular mechanisms that contribute to the development and progression of COPD. Whether you’re a patient, caregiver, or a curious reader, understanding these critical aspects can help you make informed decisions about your health and stay ahead in managing this chronic disease.
Introduction
Imagine a condition where your lungs gradually lose their ability to function, making every breath a struggle. For over 300 million people worldwide, this is a daily reality due to chronic obstructive pulmonary disease (COPD). Did you know that COPD is currently the third leading cause of death globally? The copd etiology and pathophysiology are as complex as they are critical to understand—not only for effective treatment but also for prevention and early detection.
In this blog post, we will cover:
- A clear definition of COPD and what distinguishes it from other respiratory conditions.
- A deep dive into the factors that contribute to COPD’s development, from genetic predisposition and environmental exposures to immune and molecular mechanisms.
- A historical overview of how our understanding of COPD has evolved over the decades.
- Real-world case studies and examples that illustrate these concepts in practice.
- The modern relevance of COPD research and emerging treatment trends.
By the end of this post, you’ll understand the full picture of copd etiology and pathophysiology, empowering you with the knowledge needed to make informed decisions about health management, treatment options, and lifestyle choices.
What Is COPD?
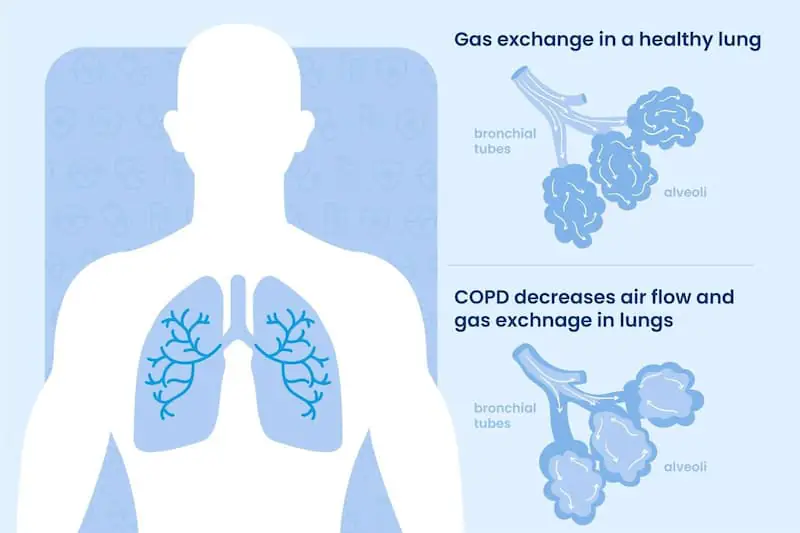
COPD is a progressive lung disease characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities. It primarily encompasses two conditions:
- Chronic Bronchitis: Inflammation and narrowing of the bronchial tubes with increased mucus production.
- Emphysema: Destruction of the alveoli, the tiny air sacs in the lungs where gas exchange occurs.
Key features of COPD include:
- Chronic Symptoms: Persistent cough, sputum production, and shortness of breath that worsen over time.
- Airflow Limitation: Irreversible obstruction in the airways, making breathing increasingly difficult.
- Progressive Nature: The disease typically worsens with age and continued exposure to risk factors.
For more detailed background information, reputable sources such as the Centers for Disease Control and Prevention (CDC) and Mayo Clinic provide comprehensive overviews.
Defining COPD Etiology and Pathophysiology
The copd etiology and pathophysiology refer to the underlying causes and the biological processes that lead to the development and progression of COPD. Unlike diseases caused by a single pathogen or environmental exposure, COPD arises from a complex interplay of factors:
- Genetic Factors: Variations in certain genes can predispose individuals to COPD.
- Environmental Exposures: Long-term exposure to noxious particles and gases, most notably from cigarette smoking, but also from air pollution and occupational hazards.
- Inflammatory Mechanisms: Chronic inflammation in the airways results in structural changes and impaired lung function.
- Oxidative Stress: An imbalance between oxidants and antioxidants in the lung tissues contributes to cellular damage.
- Protease-Antiprotease Imbalance: Disruption in the balance between enzymes that break down lung tissue (proteases) and their inhibitors leads to emphysema.
- Immune and Cellular Responses: Complex interactions among various immune cells and cytokines drive the inflammatory cascade and tissue remodeling.
Together, these elements shape the clinical manifestations and progression of COPD, affecting everything from lung architecture to overall respiratory function.
Historical and Contextual Background
Early Discoveries
The history of COPD dates back centuries, but it was only in the mid-20th century that it began to be recognized as a distinct disease entity. Early medical descriptions often grouped chronic cough and breathing difficulties under general respiratory ailments. Over time, however, clinical observations and research began to differentiate COPD from asthma and other obstructive lung diseases.
Smoking and Industrialization
A major turning point in understanding COPD came with the recognition of cigarette smoking as the principal risk factor. Studies from the 1960s and 1970s provided compelling evidence linking smoking to chronic bronchitis and emphysema. With industrialization and urbanization, additional environmental pollutants were identified as contributing factors.
Evolution of Pathophysiological Insights
In the latter part of the 20th century, researchers began to unravel the complex mechanisms underlying COPD:
- Inflammatory Processes: Detailed studies showed that chronic exposure to irritants led to persistent inflammation, with the release of cytokines and proteolytic enzymes.
- Structural Changes: Advances in imaging and histopathology revealed the destruction of alveolar walls (emphysema) and the remodeling of airways.
- Molecular Biology: The advent of molecular biology techniques allowed scientists to explore genetic predispositions and the role of oxidative stress, leading to the modern concept of protease-antiprotease imbalance.
These historical milestones set the stage for our current, multifaceted understanding of copd etiology and pathophysiology.
In-Depth Exploration of COPD Etiology and Pathophysiology
Understanding the origins and progression of COPD requires a detailed look at several interrelated components. Below, we explore each factor in depth.
Genetic Factors
Inherited Susceptibility
Genetics plays a significant role in determining who develops COPD. Although smoking is the most important risk factor, not all smokers develop COPD, suggesting that genetic predisposition is a key determinant:
- Family History: Studies show that individuals with a family history of COPD are more likely to develop the disease. Genetic factors account for an estimated 20% to 40% of the variance in susceptibility.
- Gene Variants: Research has identified several genetic polymorphisms associated with COPD risk. For example:
- Alpha-1 Antitrypsin Deficiency: A well-known genetic disorder where the lack of the alpha-1 antitrypsin protein leads to unopposed protease activity and emphysema.
- Other Candidate Genes: Variations in genes involved in inflammatory pathways, antioxidant defense, and lung development (such as SERPINE2 and GSTM1) have been implicated.
Example:
Consider two long-term smokers. One develops severe COPD by age 60, while the other remains relatively healthy. Genetic testing may reveal that the former carries a mutation in the alpha-1 antitrypsin gene, highlighting the role of genetic susceptibility in copd etiology and pathophysiology.
Gene–Environment Interactions
Genetics and environmental exposures work hand in hand:
- Synergistic Effects: Genetic predispositions (such as alpha-1 antitrypsin deficiency) can amplify the harmful effects of environmental exposures like cigarette smoke.
- Modifying Risk: Even among smokers, those with certain genetic markers are at a higher risk, underscoring the importance of gene–environment interactions in COPD development.
Environmental and Lifestyle Factors
Cigarette Smoking
Smoking remains the single most important risk factor for COPD:
- Toxic Chemicals: Cigarette smoke contains thousands of chemicals, many of which cause oxidative stress and inflammation in the lungs.
- Chronic Inflammation: Prolonged exposure leads to persistent inflammation, which gradually damages the airways and alveoli.
- Dose-Response Relationship: The risk of developing COPD increases with both the duration and intensity of smoking.
Air Pollution and Occupational Exposures
Beyond smoking, various environmental pollutants contribute to COPD:
- Ambient Air Pollution: Exposure to particulate matter (PM2.5 and PM10), nitrogen dioxide (NO₂), and sulfur dioxide (SO₂) has been linked to an increased risk of COPD.
- Occupational Hazards: Individuals working in industries with high exposure to dust, chemicals, and fumes (e.g., construction, mining, agriculture) are at a higher risk.
- Indoor Air Quality: Poor ventilation and exposure to biomass fuels for cooking and heating in poorly ventilated spaces also increase risk, especially in developing countries.
Lifestyle and Dietary Factors
- Diet: Emerging evidence suggests that diets high in processed foods and low in antioxidants may exacerbate oxidative stress in the lungs. Conversely, a diet rich in fruits and vegetables may offer some protection.
- Physical Activity: Sedentary lifestyles can compound the effects of lung damage, while regular exercise may help maintain respiratory function.
- Socioeconomic Factors: Lower socioeconomic status is often associated with higher exposure to pollutants, poorer nutrition, and reduced access to healthcare, all of which can increase COPD risk.
Bullet Points – Key Environmental Factors:
- Smoking: Main risk factor; duration and intensity are crucial.
- Air Pollution: Both outdoor (urban smog) and indoor (biomass fuel) pollution are implicated.
- Occupational Exposures: Dust, chemicals, and fumes can contribute significantly.
- Diet and Exercise: Nutritional status and physical activity levels modulate risk.
- Socioeconomic Status: Lower socioeconomic factors increase vulnerability.
Inflammatory Mechanisms and Immune Responses
Chronic Inflammation
Chronic inflammation is central to the pathophysiology of COPD:
- Inflammatory Cells: Exposure to irritants (e.g., cigarette smoke) leads to the recruitment of neutrophils, macrophages, and lymphocytes into the airways. These cells release inflammatory mediators that damage lung tissue.
- Cytokine Cascade: Key inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-8 (IL-8), and leukotrienes are elevated in COPD. These molecules perpetuate the inflammatory cycle, leading to further tissue injury.
- Proteolytic Enzymes: Enzymes such as elastase, released by neutrophils, break down the connective tissue of the lungs, contributing to the destruction seen in emphysema.
Immune Dysregulation
- Innate Immunity: The innate immune system, including alveolar macrophages and neutrophils, plays a crucial role in the initial response to inhaled irritants. In COPD, these cells become chronically activated.
- Adaptive Immunity: There is also evidence that adaptive immune responses, particularly involving CD8+ T cells, contribute to the ongoing inflammation and tissue damage.
- Autoimmunity: Some studies suggest that an autoimmune component may be involved in COPD, where immune cells mistakenly target lung tissue, further exacerbating inflammation.
Real-World Scenario:
A long-term smoker’s lungs gradually accumulate inflammatory cells due to repeated exposure to cigarette smoke. Over years, the chronic inflammation leads to the release of proteolytic enzymes that destroy alveolar walls, causing emphysema. This process, coupled with immune dysregulation, is at the heart of copd etiology and pathophysiology.
Oxidative Stress and Protease-Antiprotease Imbalance
Oxidative Stress
- Free Radicals: Inhaled irritants, particularly cigarette smoke, generate reactive oxygen species (ROS) that cause oxidative damage to lung tissues.
- Antioxidant Defenses: Normally, the lungs are equipped with antioxidant systems (e.g., superoxide dismutase, glutathione) to neutralize ROS. In COPD, these defenses are overwhelmed, leading to cellular damage.
- DNA and Protein Damage: Oxidative stress can damage DNA, proteins, and lipids, contributing to cell death and tissue destruction.
Protease-Antiprotease Imbalance
- Proteases: Neutrophils release proteolytic enzymes (like elastase) that break down the extracellular matrix and lung tissue.
- Antiproteases: Alpha-1 antitrypsin (AAT) is the body’s natural inhibitor of these proteases. In conditions like AAT deficiency or overwhelming protease activity due to smoking, this balance is disrupted.
- Tissue Destruction: The resulting imbalance leads to the breakdown of alveolar walls, which is the hallmark of emphysema, one of the main components of COPD.
Structural Changes: Airway Remodeling and Emphysema
Airway Remodeling
- Chronic Inflammation: Persistent inflammation leads to structural changes in the airways, including fibrosis, thickening of the airway walls, and narrowing of the lumen.
- Goblet Cell Hyperplasia: Increased mucus production from goblet cell hyperplasia further obstructs the airways.
- Smooth Muscle Contraction: Chronic exposure to irritants can lead to an increase in smooth muscle mass, contributing to airflow limitation.
Emphysema
- Alveolar Destruction: Emphysema is characterized by the irreversible destruction of alveolar walls, resulting in enlarged airspaces and reduced surface area for gas exchange.
- Loss of Elasticity: Damage to elastic fibers in the lung impairs the ability of the lungs to recoil, leading to air trapping and hyperinflation.
- Types of Emphysema: Centrilobular emphysema, often associated with smoking, affects the central portions of the acini, while panlobular emphysema, which can be seen in AAT deficiency, affects the entire acinus.
Molecular and Cellular Mechanisms
Cellular Signaling Pathways
- NF-κB Activation: In response to oxidative stress and inflammatory stimuli, the nuclear factor kappa B (NF-κB) pathway is activated, leading to the transcription of inflammatory genes.
- MAPK Pathways: Mitogen-activated protein kinase (MAPK) pathways also play a role in mediating inflammation and cell proliferation in COPD.
- Apoptosis and Senescence: Cellular damage from oxidative stress can induce apoptosis (programmed cell death) and senescence (cellular aging), contributing to the loss of functional lung cells.
Role of Cytokines and Chemokines
- Cytokines: TNF-α, IL-8, IL-6, and other cytokines are key mediators in the inflammatory cascade of COPD.
- Chemokines: These molecules recruit immune cells to the lungs, perpetuating the cycle of inflammation and tissue destruction.
Immune Cell Infiltration
- Neutrophils and Macrophages: Chronic exposure to irritants leads to the accumulation of neutrophils and macrophages in the airways and alveoli.
- CD8+ T Cells: These cells are frequently observed in the lung tissues of COPD patients and are associated with cytotoxic activity and further tissue damage.
Real-World Examples and Case Studies
Case Study 1: The Heavy Smoker
Consider Michael, a 65-year-old man with a 40-year history of cigarette smoking. Despite quitting 10 years ago, Michael was diagnosed with COPD after experiencing increasing shortness of breath and a chronic cough. Genetic testing revealed that he carries a mild deficiency in alpha-1 antitrypsin, making him more vulnerable to the protease-antiprotease imbalance triggered by smoking. His case illustrates how a combination of environmental exposures (smoking) and genetic susceptibility can lead to the onset of COPD.
Case Study 2: Occupational Exposure
Lisa, a 55-year-old construction worker, spent most of her career exposed to dust, chemicals, and other pollutants. Although she never smoked, she developed COPD symptoms, including persistent coughing and breathlessness. Her diagnosis highlights the role of occupational exposures as significant environmental risk factors, demonstrating that non-smokers can also develop COPD if they are exposed to high levels of respiratory irritants.
Case Study 3: The Role of Inflammation and Oxidative Stress
John, a 60-year-old former smoker, presented with emphysema characterized by severe dyspnea and reduced lung capacity. Laboratory tests revealed elevated markers of oxidative stress and increased levels of inflammatory cytokines, such as TNF-α and IL-8. John’s case underscores how chronic inflammation and oxidative damage—driven by decades of smoking—result in the structural destruction of lung tissue that defines emphysema.
Case Study 4: A Multidisciplinary Approach
Sarah, a 58-year-old woman diagnosed with COPD, benefited from a comprehensive treatment strategy that addressed multiple facets of her disease. In addition to pharmacologic therapy (including bronchodilators and inhaled corticosteroids), Sarah adopted lifestyle changes such as smoking cessation, regular exercise, and a diet rich in antioxidants. Pulmonary rehabilitation and stress management techniques further helped her manage her symptoms. Sarah’s improved quality of life illustrates how understanding the copd etiology and pathophysiology can lead to a holistic, patient-centered approach to treatment.
Importance and Applications
Clinical Relevance
Understanding the copd etiology and pathophysiology is critical for:
- Early Diagnosis: Identifying risk factors and early biomarkers can facilitate prompt intervention, potentially slowing disease progression.
- Targeted Treatments: Insights into molecular and cellular mechanisms have led to the development of targeted therapies—such as inhaled corticosteroids, long-acting bronchodilators, and newer biologic agents.
- Personalized Medicine: Genetic and molecular profiling allows clinicians to tailor treatment plans to individual patients, optimizing therapeutic efficacy and minimizing side effects.
Societal Impact
- Reducing Healthcare Burden: COPD is a leading cause of hospitalizations and healthcare expenditure. Effective management and early intervention can reduce these costs and improve patient outcomes.
- Quality of Life: Better understanding of disease mechanisms informs strategies to improve the quality of life for patients through pulmonary rehabilitation, nutritional support, and lifestyle modifications.
- Public Health Initiatives: Knowledge of environmental risk factors supports policies aimed at reducing air pollution and improving workplace safety.
Research and Innovation
- Biomarker Discovery: Continued research is identifying biomarkers related to inflammation, oxidative stress, and genetic predisposition, which can help in monitoring disease progression and treatment response.
- Novel Therapeutics: Advances in molecular biology have opened new avenues for therapy, including inhibitors targeting specific inflammatory pathways (e.g., NF-κB, MAPK) and antioxidants aimed at reducing oxidative stress.
- Interdisciplinary Collaboration: COPD research fosters collaboration among pulmonologists, geneticists, immunologists, and environmental scientists, driving innovation and improving patient care.
Common Misconceptions and FAQs
Common Misconceptions
Misconception 1: COPD only affects smokers.
Reality: While smoking is the primary risk factor, non-smokers can also develop COPD due to genetic predispositions, occupational exposures, and environmental pollutants.Misconception 2: COPD is just chronic bronchitis or emphysema.
Reality: COPD is an umbrella term encompassing both chronic bronchitis and emphysema. The disease is characterized by a combination of airway inflammation, airflow limitation, and alveolar destruction.Misconception 3: Once you quit smoking, COPD stops progressing.
Reality: Quitting smoking can slow the progression of COPD and improve symptoms, but it does not fully reverse the damage that has already occurred.Misconception 4: COPD is solely caused by lung infections.
Reality: Although infections can exacerbate COPD, the underlying etiology is multifactorial, involving chronic exposure to irritants, inflammation, oxidative stress, and genetic factors.
Frequently Asked Questions (FAQs)
Q1: What is the primary cause of COPD?
A: The most significant risk factor is long-term exposure to cigarette smoke. However, genetic factors (like alpha-1 antitrypsin deficiency), air pollution, and occupational exposures also contribute.
Q2: How does oxidative stress affect the lungs in COPD?
A: Oxidative stress results from an imbalance between reactive oxygen species (ROS) and antioxidants, leading to cellular damage, inflammation, and the destruction of alveolar walls, which are key features of emphysema.
Q3: What role do inflammatory cytokines play in COPD?
A: Inflammatory cytokines such as TNF-α, IL-8, and IL-6 drive chronic inflammation in the lungs, leading to tissue damage, airway remodeling, and reduced lung function.
Q4: Can COPD be reversed?
A: Currently, the damage caused by COPD is largely irreversible. However, early diagnosis, smoking cessation, and targeted therapies can slow progression and improve quality of life.
Q5: Are there any new treatments targeting the underlying causes of COPD?
A: Yes. Research is ongoing into novel therapies, including antioxidants, anti-inflammatory agents targeting specific molecular pathways (e.g., NF-κB inhibitors), and gene-based therapies aimed at correcting genetic predispositions.
Modern Relevance and Current Trends
Advances in Genetic Research
- Genomic Profiling: High-throughput sequencing and genome-wide association studies (GWAS) have identified genetic variants that increase susceptibility to COPD. This research is paving the way for personalized medicine approaches.
- Alpha-1 Antitrypsin Therapy: Advances in understanding alpha-1 antitrypsin deficiency have led to the development of augmentation therapies that help slow emphysema progression in affected individuals.
Innovations in Molecular and Cellular Mechanisms
- Targeting Inflammatory Pathways: Biologic therapies targeting TNF-α have been used in related inflammatory conditions, and research continues into novel inhibitors that can modulate the NF-κB and MAPK pathways.
- Oxidative Stress Interventions: Antioxidant therapies, including new molecules designed to boost the lung’s natural defenses, are being investigated as potential treatments for reducing cellular damage in COPD.
Role of the Microbiome
- Microbiome Research: Emerging studies are examining how the lung microbiome influences COPD. Changes in the microbial communities within the airways may contribute to exacerbations and chronic inflammation.
- Probiotics and Prebiotics: Research into modifying the lung and gut microbiome through dietary interventions, probiotics, and prebiotics offers promising avenues for adjunctive therapy in COPD.
Environmental and Lifestyle Interventions
- Air Quality Initiatives: Governments and public health organizations are increasingly focused on reducing air pollution, a key environmental risk factor for COPD.
- Smoking Cessation Programs: Ongoing public health campaigns and smoking cessation programs continue to be critical in preventing COPD and slowing its progression.
- Digital Health: Mobile apps, wearable devices, and telemedicine are transforming how patients monitor their lung function and manage COPD on a day-to-day basis.
Emerging Technologies and Research Directions
- Gene Editing: Advances in CRISPR and other gene-editing technologies offer hope for addressing genetic factors such as alpha-1 antitrypsin deficiency.
- Biomarker Discovery: Ongoing research is focused on identifying reliable biomarkers for early detection, disease progression, and response to therapy.
- Personalized Medicine: Integrating data from genomics, proteomics, and metabolomics is leading to more personalized treatment strategies that can be tailored to individual patient profiles.
Conclusion and Call to Action
The copd etiology and pathophysiology are complex and multifaceted, involving genetic predisposition, chronic exposure to environmental irritants, inflammatory and immune responses, oxidative stress, and structural changes in the lungs. This comprehensive understanding has evolved over decades of research—from early clinical observations linking smoking to lung damage, to modern genomic studies and molecular research that are now paving the way for innovative therapies.
Key Takeaways:
- Multifactorial Causes: COPD arises from the combined effects of genetic factors, environmental exposures, chronic inflammation, oxidative stress, and immune dysregulation.
- Irreversible Changes, but Manageable: Although the structural changes in the lungs are largely irreversible, early intervention, lifestyle modifications, and targeted therapies can slow progression and improve quality of life.
- Personalized Approaches: Advances in genetic and molecular research are enabling more personalized treatment plans that address the specific underlying causes in each patient.
- Prevention Is Critical: Reducing exposure to key risk factors—such as cigarette smoke and environmental pollutants—is essential for preventing COPD and mitigating its impact.
Call to Action
If you found this guide on copd etiology and pathophysiology informative, please share it with your family, friends, and anyone interested in learning more about this critical topic. Stay informed by exploring reputable sources such as the Centers for Disease Control and Prevention (CDC), Mayo Clinic’s COPD page, and American Lung Association. We encourage you to leave comments, ask questions, or share your personal experiences with COPD below.
Understanding the copd etiology and pathophysiology is not just an academic exercise—it’s a critical step toward improved treatment, better quality of life, and a future where lung health is preserved for all. Stay proactive about your respiratory health, and join us in spreading awareness about COPD.
Final Thoughts
The journey through the copd etiology and pathophysiology reveals a disease that is as complex as it is impactful. With every new research breakthrough—from genetic studies and molecular signaling insights to innovations in environmental health and microbiome science—we move closer to unlocking the mysteries of COPD. While the damage to the lungs may be irreversible, understanding these underlying mechanisms empowers us to develop strategies that slow disease progression, improve patient outcomes, and ultimately reduce the global burden of COPD.
Knowledge is power. By staying informed, embracing healthier lifestyles, and supporting ongoing research, we can make a significant difference in the fight against COPD. Let’s work together to breathe easier and build a healthier future.