Bipolar disorder is one of the most fascinating—and challenging—mental health conditions out there. Its unpredictable mood swings and episodes of depression and mania affect millions of people worldwide. In this in-depth post, we’re diving into the etiology of bipolar disorder, exploring everything from genetics and brain chemistry to environmental triggers and even metabolic factors. Whether you’re a student, clinician, or a curious reader looking to understand the roots of this condition, this article will guide you through the key concepts, historical milestones, modern research, and practical implications.
Introduction: Why Understanding the Etiology of Bipolar Disorder Matters
Imagine living with intense mood swings that can range from devastating lows of depression to unbridled highs of mania. For many individuals with bipolar disorder, this is a daily reality. Research shows that nearly 2–3% of the global population is affected by this disorder, yet its roots remain as complex as the symptoms themselves.
Did you know? Recent studies suggest that the cause of bipolar disorder isn’t confined to one single factor. Instead, a perfect storm of genetic predisposition, brain chemistry imbalances, environmental stressors, and even metabolic disruptions converge to trigger its onset.
In this article, we’ll:
- Define the etiology of bipolar disorder and explain its essential components.
- Explore the historical evolution of theories and research on bipolar disorder.
- Break down the major contributing factors—genetic, neurobiological, environmental, and metabolic.
- Address common misconceptions and answer frequently asked questions.
- Highlight modern research trends and discuss how these findings can guide future treatments.
Understanding the etiology is not only vital for clinicians seeking better treatments but also for anyone trying to grasp the complexities behind bipolar disorder. So, let’s embark on this journey of discovery together!
Defining Bipolar Disorder and Its Etiology
What Is Bipolar Disorder?
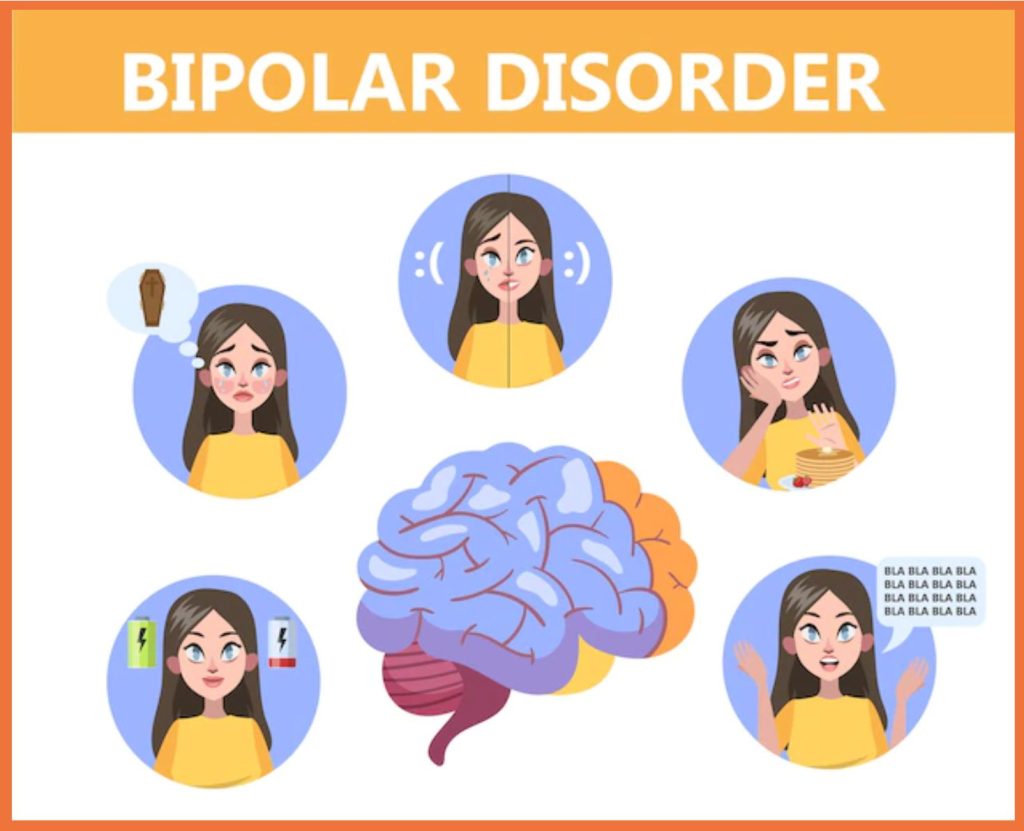
Bipolar disorder, often referred to as manic-depressive illness, is a chronic mental health condition characterized by significant fluctuations in mood, energy, and activity levels. People with bipolar disorder typically experience episodes of:
- Mania or Hypomania: Elevated mood, increased energy, rapid speech, and impulsive behaviors.
- Depression: Deep sadness, hopelessness, loss of interest in activities, and difficulty concentrating.
While both bipolar I and bipolar II disorders fall under the bipolar spectrum, they differ mainly in the severity and duration of manic episodes. Bipolar I involves full-blown manic episodes, whereas bipolar II is marked by hypomania combined with severe depressive episodes.
What Does “Etiology” Mean?
The term etiology of bipolar disorder refers to the study of its origins and causes. Unlike conditions caused by a single factor, bipolar disorder arises from a multifactorial interplay:
- Genetics: Family history and specific genetic variants can predispose an individual.
- Neurobiology: Imbalances in brain neurotransmitters (such as dopamine, serotonin, and glutamate) and structural abnormalities in brain regions are key players.
- Environmental and Psychosocial Factors: Stressful life events, trauma, and even childhood adversity can trigger episodes.
- Metabolic Factors: Emerging research suggests that energy regulation and metabolism—such as those influenced by diet and circadian rhythms—also contribute.
By understanding these components, researchers and clinicians hope to develop more targeted interventions that not only treat the symptoms but address the root causes of the disorder.
Historical Perspectives on Bipolar Disorder
Early Theories and Misconceptions
Historically, bipolar disorder was often misunderstood. Early theories frequently attributed the condition to flawed family dynamics or personal weaknesses. Terms like “manic depression” were widely used without a nuanced understanding of the underlying causes. In the mid-20th century, however, the pendulum swung toward biological explanations:
- Psychoanalytic Theories: Initially, psychoanalytic approaches suggested that unresolved childhood conflicts could lead to bipolar symptoms. Over time, these ideas gave way to more scientifically grounded models.
- Biological Breakthroughs: The discovery of neurotransmitters and the development of mood-stabilizing medications such as lithium marked a turning point. Studies began to reveal the strong hereditary component of the disorder, sparking interest in genetic research.
The Evolution of Research
In the decades since, the field has seen an explosion of research:
- Twin and Adoption Studies: Research revealed that bipolar disorder is highly heritable, with twin studies showing significantly higher concordance rates among identical twins.
- Neuroimaging Advances: Technologies like MRI and fMRI have allowed scientists to observe structural and functional abnormalities in the brains of individuals with bipolar disorder.
- Metabolic and Circadian Studies: More recently, research from institutions like Edinburgh University has begun to view bipolar depression through the lens of metabolic dysregulation, linking diet, sleep patterns, and energy metabolism to mood stability.
These milestones have collectively reshaped our understanding, emphasizing that the etiology of bipolar disorder is a dynamic interplay of multiple factors.
In-Depth Exploration of the Etiology of Bipolar Disorder
Understanding bipolar disorder requires breaking down its complex etiology into several key components. In this section, we’ll examine each factor in detail.
Genetic Factors
The Role of Heredity
Genetic studies have consistently shown that bipolar disorder runs in families. Here’s what we know:
- Twin Studies: Identical twins share nearly 100% of their genes, and studies have found that if one twin has bipolar disorder, the other is at a much higher risk—even though the rate is not 100%. This strongly supports a genetic link.
- Family History: Individuals with a first-degree relative (parent or sibling) diagnosed with bipolar disorder have a significantly increased risk compared to the general population.
- Genome-Wide Association Studies (GWAS): These studies have identified numerous genetic variants—each contributing a small amount—to overall susceptibility. Key genes implicated include CACNA1C, ODZ4, and ANK3, among others. Although no single gene can predict bipolar disorder, the cumulative effect of many genes appears to play a major role.
Gene-Environment Interactions
Importantly, having a genetic predisposition does not guarantee the development of bipolar disorder. Instead, genetic vulnerability often interacts with environmental stressors:
- Epigenetics: Environmental factors such as stress and trauma can alter gene expression without changing the DNA sequence. This means that even if you have susceptibility genes, how they are expressed can depend on your life experiences.
- Threshold Models: The “kindling hypothesis” suggests that initial episodes may require significant stress, but subsequent episodes can occur with lower levels of stress as the brain becomes more sensitized.
Neurobiological Mechanisms
Neurotransmitter Imbalances
One of the most studied aspects of bipolar disorder is the role of neurotransmitters:
- Dopamine: Often linked to the high-energy, risk-taking behaviors of mania, dopamine dysregulation is considered central to bipolar disorder. An overactive dopaminergic system during mania may lead to the impulsivity and grandiosity seen in many patients.
- Serotonin: This neurotransmitter is crucial in regulating mood. Lower levels of serotonin and its metabolite (5-HIAA) have been associated with depressive states in bipolar disorder.
- Glutamate: Emerging research suggests that glutamatergic dysfunction may also play a role. Increased glutamate levels in certain brain regions have been observed during manic episodes, hinting at its potential role in the mood swings characteristic of bipolar disorder.
Brain Structure and Function
Neuroimaging studies have provided a window into the brain’s architecture in bipolar disorder:
- Structural Abnormalities: MRI studies have shown alterations in brain regions responsible for mood regulation, including the prefrontal cortex, amygdala, and hippocampus. For instance, reductions in the volume of the prefrontal cortex may contribute to impaired decision-making and emotional regulation.
- Functional Changes: Functional MRI (fMRI) studies reveal that during mood episodes, the brain’s activity patterns change significantly. Manic episodes are often associated with hyperactivity in the limbic system (which processes emotions) and hypoactivity in the prefrontal cortex (which regulates emotions).
- White Matter Integrity: Changes in white matter—responsible for communication between brain regions—have been noted, which may disrupt the networks involved in mood regulation.
Intracellular Signaling and Neuroplasticity
Beyond neurotransmitters, the intracellular processes within brain cells also contribute:
- G-Protein Signaling: Abnormal coupling of neurotransmitter receptors to G proteins has been observed, which could alter the cell’s response to neurotransmitters.
- Neurotrophic Factors: Reduced levels of brain-derived neurotrophic factor (BDNF) have been found during depressive episodes, suggesting that impaired neuroplasticity might underlie the brain’s inability to recover between episodes.
- Apoptosis and Cellular Health: Some studies indicate that increased cellular stress and early apoptosis (programmed cell death) in brain regions may contribute to the progression of bipolar disorder.
Environmental and Psychosocial Factors
Stress and Trauma
Environmental stressors are among the most critical external triggers:
- Life Events: Traumatic events, such as the death of a loved one, divorce, or severe financial problems, can precipitate mood episodes. Studies suggest that a significant percentage of bipolar patients experience a stressful life event in the months preceding an episode.
- Childhood Adversity: Early-life trauma, including abuse or neglect, has been linked to an earlier onset of bipolar disorder and may worsen its course.
- Social Environment: Chronic stress from ongoing interpersonal conflicts or socio-economic challenges can exacerbate symptoms.
Substance Use and Lifestyle
Substance use and lifestyle choices also interact with genetic and neurobiological factors:
- Drug and Alcohol Use: Use of substances like cannabis or cocaine can trigger manic episodes, especially in genetically predisposed individuals.
- Sleep Disruptions: Bipolar disorder is closely linked with disturbances in sleep patterns. Changes in sleep, whether due to stress or lifestyle, can act as both a trigger and a symptom of mood episodes.
- Diet and Metabolism: Emerging research suggests that metabolic factors—such as the impact of a ketogenic diet or metabolic syndrome—may influence mood stability. These findings are leading to the idea that bipolar depression might be viewed partly as a metabolic disorder.
Metabolic and Circadian Contributions
Metabolic Dysfunction
Recent studies, including groundbreaking research from Edinburgh University, propose that bipolar depression may be tied to metabolic dysfunction:
- Energy Regulation: Just as our bodies need to regulate energy properly, disturbances in metabolic processes may contribute to mood instability.
- Dietary Interventions: Diets like the ketogenic diet have shown promising results in stabilizing mood by altering the way the body uses energy. Research indicates that some individuals with bipolar disorder experience improved mood stability when they adopt a diet that modifies their metabolic pathways.
Circadian Rhythms and Sleep
The body’s internal clock plays a crucial role in regulating mood:
- Light Sensitivity and Seasonal Patterns: Many people with bipolar disorder report that their mood fluctuates with the seasons. Disruptions in circadian rhythms—the natural sleep-wake cycle—are thought to be a key factor.
- Sleep Patterns: Abnormal sleep patterns are not only a symptom but also a potential trigger for mood episodes. Technologies that monitor sleep patterns, such as radar sleep devices, are being explored as tools to predict upcoming mood changes.
- Melatonin and Hormonal Regulation: Hormones like melatonin, which are regulated by light exposure and sleep, are also implicated. Dysregulation in melatonin secretion can disturb circadian rhythms, potentially leading to mood instability.
Real-World Examples and Case Studies
Case Study 1: The Genetic Puzzle
Consider a family where one parent and a sibling have been diagnosed with bipolar disorder. Despite sharing many of the same genes, not every family member develops the disorder. This scenario highlights the role of gene-environment interactions. For instance, if a child with a genetic predisposition experiences significant early-life stress or trauma, they may be more likely to develop bipolar disorder compared to a sibling who grew up in a less stressful environment.
Case Study 2: Neuroimaging Insights
In a groundbreaking study using functional MRI, researchers observed that individuals experiencing manic episodes exhibited hyperactivity in their amygdala (the brain’s emotional center) and hypoactivity in their prefrontal cortex (the rational decision-making center). These findings not only support the dopamine hypothesis of mania but also underscore how imbalances in brain circuits contribute to the symptoms of bipolar disorder.
Case Study 3: Metabolic Interventions
A recent study conducted by researchers at Edinburgh University involved 27 individuals with bipolar depression who adopted a ketogenic diet for eight weeks. Approximately one-third of participants experienced more stable moods and reduced depressive symptoms. This case study opens up promising avenues for metabolic interventions as part of a comprehensive treatment strategy.
Case Study 4: Predicting Episodes Through Sleep Patterns
Another innovative study involved using radar sleep devices to monitor sleep patterns in individuals with bipolar disorder over an 18-month period. Researchers discovered that subtle changes in sleep patterns could predict the onset of manic or depressive episodes. These findings suggest that real-time monitoring could someday help in the early intervention and prevention of mood episodes.
Importance and Applications of Understanding the Etiology
Clinical Implications
Understanding the etiology of bipolar disorder has immense clinical value:
- Targeted Treatments: By identifying the specific genetic, neurobiological, and metabolic factors involved, treatments can be tailored to individual needs. For example, patients with pronounced metabolic dysregulation might benefit from dietary modifications alongside traditional therapies.
- Early Intervention: Recognizing early signs—whether genetic markers or changes in sleep patterns—can lead to earlier diagnosis and intervention, potentially mitigating the severity of future episodes.
- Personalized Medicine: As we uncover more about the interplay between genes and the environment, personalized treatment plans can be developed. Pharmacogenomics, which tailors drug treatments based on an individual’s genetic makeup, is a promising area in this regard.
Societal and Economic Benefits
Beyond clinical settings, understanding the etiology has broader implications:
- Reducing Stigma: When bipolar disorder is understood as a multifactorial biological condition rather than a character flaw, stigma can be reduced. Public education can foster empathy and support for affected individuals.
- Improved Quality of Life: Tailored treatment and early intervention can lead to better management of symptoms, improved social and occupational functioning, and overall enhanced quality of life.
- Economic Savings: Effective management of bipolar disorder can reduce hospitalizations, improve work productivity, and lessen the financial burden on healthcare systems.
Research and Innovation
In the research domain, this comprehensive understanding opens new doors:
- Biomarker Discovery: Identifying biomarkers—whether in blood, brain imaging, or genetic profiles—can help in developing diagnostic tests and monitoring treatment responses.
- Novel Therapeutic Targets: Insights into intracellular signaling, neuroplasticity, and metabolic pathways can lead to the development of new medications that address the root causes rather than just alleviating symptoms.
- Integration of Multidisciplinary Approaches: The convergence of genetics, neuroimaging, immunology, and metabolism creates an integrated model of bipolar disorder, paving the way for innovative research collaborations.
Common Misconceptions and FAQs
Common Misconceptions
Misconception 1: Bipolar Disorder Is Just Mood Swings
- Reality: Bipolar disorder involves severe and sustained mood changes that go far beyond the normal ups and downs everyone experiences. These episodes can significantly impair daily functioning.
Misconception 2: It’s Caused by Poor Parenting or Weak Willpower
- Reality: Research overwhelmingly supports that bipolar disorder is a complex interplay of genetic, neurobiological, and environmental factors. Blaming poor parenting or personal weakness is both inaccurate and stigmatizing.
Misconception 3: Only One Factor Causes Bipolar Disorder
- Reality: The etiology of bipolar disorder is multifactorial. No single cause exists; instead, various factors—including genetics, brain chemistry, environment, and metabolism—contribute to its development.
Frequently Asked Questions (FAQs)
Q: Is bipolar disorder hereditary?
A: Yes. Family, twin, and adoption studies suggest that genetics play a significant role in bipolar disorder, although environmental factors also contribute.
Q: Can lifestyle changes help manage bipolar disorder?
A: Absolutely. Managing stress, improving sleep hygiene, and even dietary interventions such as the ketogenic diet can help stabilize mood and reduce episode frequency.
Q: Are there any early warning signs of bipolar disorder?
A: Early signs can include subtle changes in sleep patterns, increased sensitivity to light, or minor shifts in mood. Monitoring these changes with modern technology (e.g., sleep trackers) is an active area of research.
Q: How is bipolar disorder diagnosed?
A: Diagnosis is based on clinical interviews, symptom history, and sometimes neuroimaging and genetic studies. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides criteria for diagnosis.
Q: Is bipolar disorder curable?
A: Currently, bipolar disorder is considered a lifelong condition. However, with effective management—including medication, psychotherapy, and lifestyle modifications—many individuals lead fulfilling lives.
Modern Relevance and Current Trends
Precision Medicine and Biomarker Research
Researchers are working toward the development of biomarkers that can predict the onset of bipolar episodes. Advances in genetic testing, neuroimaging, and metabolic profiling are all converging to provide a more accurate and personalized approach to treatment.
Metabolic Psychiatry: A New Frontier
Recent work, including studies highlighted by Edinburgh University, suggests that viewing bipolar depression as a metabolic disorder could revolutionize treatment. Diet, particularly the ketogenic diet, is being investigated as a potential adjunct therapy for stabilizing mood.
Technological Innovations in Monitoring
Wearable devices and radar sleep technology are being used to monitor sleep patterns and predict mood changes. These tools promise to give clinicians a heads-up on when an episode might occur, allowing for timely intervention.
Integrated Models of Treatment
Modern treatment approaches increasingly emphasize an integrated model—combining medications, psychotherapy, and lifestyle modifications. By addressing the multifactorial etiology of bipolar disorder, these models aim for a more holistic and effective management plan.
Ongoing Challenges and Future Directions
Despite significant advances, challenges remain:
- Heterogeneity of the Disorder: The varied presentation of bipolar disorder means that what works for one individual may not work for another.
- Stigma and Awareness: Continued efforts are needed to educate the public and reduce stigma.
- Longitudinal Research: More long-term studies are required to understand how early interventions can change the course of the disorder.
Conclusion and Call to Action
The etiology of bipolar disorder is as complex as it is fascinating. From genetic predispositions and neurotransmitter imbalances to environmental triggers and metabolic dysfunction, many factors contribute to this challenging condition. Understanding these factors not only aids in developing better treatments but also helps reduce the stigma that so often surrounds mental illness.
Key Takeaways:
- Bipolar disorder is a multifactorial condition with genetic, neurobiological, environmental, and metabolic contributors.
- Early identification and personalized treatment can greatly improve quality of life.
- Ongoing research into biomarkers, metabolic interventions, and advanced monitoring technologies promises a future of more targeted and effective treatments.
Call to Action:
If you or someone you know is affected by bipolar disorder, consider sharing this article to spread awareness about its complex causes and emerging treatment approaches. We encourage you to stay informed, seek professional guidance when needed, and support ongoing research efforts. Your engagement can help transform lives and advance our understanding of bipolar disorder.
For more information, check out reputable sources such as the National Institute of Mental Health and Mayo Clinic. We’d love to hear your thoughts—please leave a comment below or share this post on social media!
This post is intended for educational purposes and should not replace professional medical advice. If you or someone you know is struggling, please seek help from a qualified healthcare provider.