Diabetic Retinopathy Overview
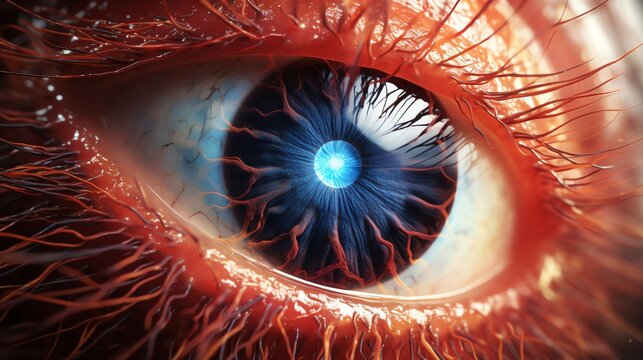
Diabetic retinopathy is a complication of diabetes that affects the eyes. High blood sugar levels associated with diabetes can lead to damage in the blood vessels of the retina, the light-sensitive tissue at the back of the eye. If not detected and managed, it can cause vision loss or blindness.
How Diabetes Affects the Eyes:
The retina requires a constant blood supply provided by tiny blood vessels. Persistently high blood sugar can damage these vessels through three stages:
Background Retinopathy:
- Tiny bulges (microaneurysms) develop in the blood vessels of the retina.
- These may leak small amounts of blood but typically do not impact vision at this stage.
Pre-Proliferative Retinopathy:
- Widespread and more severe changes occur in the blood vessels.
- This stage can involve more significant bleeding within the eye.
Proliferative Retinopathy:
- New, abnormal blood vessels form on the retina due to insufficient blood supply. These new vessels are fragile and prone to bleeding.
- Scar tissue may also develop, potentially leading to vision loss.
Timely detection and treatment can prevent or slow the progression of diabetic retinopathy.
Risk Factors for Diabetic Retinopathy:
Individuals with type 1 or type 2 diabetes are at risk, especially those who:
- Have had diabetes for a long time.
- Experience persistently high blood sugar (glucose) levels.
- Have high blood pressure or high cholesterol.
- Are pregnant.
- Are of Asian or Afro-Caribbean descent.
Controlling blood sugar, blood pressure, and cholesterol can significantly lower the risk.
Symptoms of Diabetic Retinopathy:
Early-stage diabetic retinopathy usually has no noticeable symptoms. As it progresses, symptoms may include:
- Gradually worsening vision.
- Sudden loss of vision.
- Floaters (shapes floating in your field of vision).
- Blurred or patchy vision.
- Eye pain or redness.
It is important to consult an eye care professional promptly if these symptoms occur.
Diabetic Eye Screening:
Annual eye screenings are recommended for individuals with diabetes who are 12 years or older. The screening involves examining the back of the eyes and taking photographs to detect early signs of retinopathy before symptoms arise. Early detection allows for timely intervention, reducing the risk of severe vision loss.
Reducing the Risk of Diabetic Retinopathy:
- Control Blood Sugar Levels: Consistently managing blood glucose levels helps protect against blood vessel damage in the eyes.
- Manage Blood Pressure and Cholesterol: High blood pressure and cholesterol can worsen retinopathy.
- Follow Medication Instructions: Take prescribed diabetes medications as directed.
- Attend Regular Screenings: Timely detection through screening is critical for prevention and management.
- Healthy Lifestyle Choices: Maintain a balanced diet, engage in regular exercise, and avoid smoking.
Treatments for Diabetic Retinopathy:
Treatment is necessary when diabetic retinopathy poses a threat to vision. Options include:
- Laser Treatment:
- Uses laser light to treat abnormal blood vessels, prevent new vessel growth, and reduce leakage.
- Injections:
- Medications injected directly into the eyes to reduce swelling and slow disease progression.
- Surgery (Vitrectomy):
- Involves removing blood or scar tissue from the eye to restore vision.
By managing diabetes effectively and attending regular screenings, individuals can minimize the impact of diabetic retinopathy and preserve their vision.
Stages of diabetic retinopathy
Diabetic retinopathy progresses through several stages, each indicating increasing damage to the blood vessels in the retina caused by high blood sugar levels. Timely diagnosis and intervention can help prevent further deterioration and vision loss. Here’s a detailed breakdown of the stages:
Stage One: Background Retinopathy
- Description: At this stage, tiny bulges known as microaneurysms develop in the blood vessels in the retina. These bulges may leak small amounts of blood, but they typically don’t cause noticeable vision problems.
- Impact on Vision: There is no immediate impact on sight at this stage. However, it indicates an increased risk of developing more serious eye problems later on.
- Management: Treatment is not required at this stage, but managing diabetes carefully, including controlling blood sugar, blood pressure, and cholesterol, is crucial to prevent progression.
- Monitoring: Regular eye screening is essential to detect any changes. The risk of progressing to more advanced stages within three years can be greater than 25% if both eyes are affected.
Stage Two: Pre-Proliferative Retinopathy
- Description: In this stage, there are more severe changes in the blood vessels of the retina, including more significant bleeding.
- Impact on Vision: Vision may not yet be affected, but there is a higher risk that it could become impaired.
- Management: You may be advised to have more frequent monitoring, typically every three to six months, to track any changes and prevent further complications.
Stage Three: Proliferative Retinopathy
- Description: This advanced stage involves the formation of new, fragile blood vessels and scar tissue on the retina. These new blood vessels are prone to bleeding, which can lead to retinal detachment (where the retina pulls away from the back of the eye).
- Impact on Vision: There is a very high risk of vision loss at this stage.
- Management and Treatment: Urgent treatment is necessary to stabilise vision. This may involve laser therapy, injections, or surgery to manage complications, but it cannot restore lost vision.
Diabetic Maculopathy
- Description: This occurs when blood vessels in the macula, the central part of the retina responsible for sharp vision, become leaky or blocked.
- Impact on Vision: The risk of vision impairment is significant as this area is crucial for tasks like reading and recognising faces.
- Management: Specialised testing and frequent monitoring may be needed. Referral to a hospital eye specialist may be recommended to discuss possible treatments such as laser therapy or injections to prevent further damage.
Prevention and Management
- Control of Diabetes: Managing blood sugar levels is crucial for preventing the progression of diabetic retinopathy.
- Regular Screenings: Attending diabetic eye screenings allows for early detection and intervention.
- Lifestyle Changes: Maintaining a healthy weight, regular exercise, a balanced diet, and managing cholesterol and blood pressure levels can reduce risks.
- Quick Action on Symptoms: If you experience symptoms such as vision changes, floaters, or eye pain, seek prompt medical advice.
By following these steps and seeking appropriate care, people with diabetic retinopathy can manage their condition and minimise the risk of vision loss.
Treating Diabetic Retinopathy
Overview: Diabetic retinopathy treatment is typically required when the condition progresses to an advanced stage, potentially threatening vision. Treatments aim to prevent further vision loss but may not restore sight already lost. The main treatments include laser therapy, eye injections, and surgery.
Managing Diabetes as a Key Treatment
The most crucial part of managing diabetic retinopathy at any stage is maintaining good control over blood sugar levels, blood pressure, and cholesterol. This helps slow down the progression of the disease and reduce further complications.
Treatments for Advanced Diabetic Retinopathy
1. Laser Treatment
- Purpose: Laser therapy is used to target and seal abnormal blood vessels in the retina, stabilising changes and preventing vision deterioration. It’s most commonly used for proliferative retinopathy and some cases of diabetic maculopathy.
- Procedure:
- Preparation: Local anaesthetic drops numb the eye, and eye drops widen the pupils. A special contact lens is placed over the eye to focus the laser.
- Duration: The procedure takes about 20-40 minutes and is usually done as an outpatient visit.
- Experience: While not painful, some patients may feel mild pricking sensations during treatment.
- Side Effects:
- Temporary blurred vision and light sensitivity post-treatment (sunglasses may help).
- Potential complications include reduced peripheral or night vision, seeing laser patterns in the eye temporarily, and, in rare cases, minor blind spots near the central vision.
- Advice: Notify a doctor if your sight worsens after the procedure.
2. Eye Injections (Anti-VEGF Therapy)
- Purpose: Used mainly for diabetic maculopathy to inhibit the growth of abnormal blood vessels in the eye and reduce fluid leakage.
- Medications: Anti-VEGF drugs like ranibizumab (Lucentis) and aflibercept (Eylea).
- Procedure:
- The eye area is cleaned and numbed.
- A fine needle administers the medication directly into the eye.
- Typically, injections are given monthly initially, then less frequently as vision stabilises.
- Alternative Options: Steroid injections may be used if anti-VEGF therapy isn’t effective.
- Risks and Side Effects:
- Possible discomfort, eye irritation, minor bleeding, and floaters.
- Rare risks include blood clot formation, leading to heart attack or stroke.
3. Eye Surgery (Vitreoretinal Surgery)
- Purpose: Used for severe cases involving significant bleeding or scar tissue that may cause retinal detachment.
- Procedure:
- The surgeon removes some vitreous humour (jelly-like substance) from the eye and removes scar tissue.
- Laser treatment may also be applied to stabilise the retina.
- Usually performed under local anaesthetic with sedation.
- Recovery:
- You may need to wear an eye patch temporarily and avoid strenuous activities.
- Vision improvement may take several months.
- Risks and Side Effects:
- Cataract formation, further bleeding, retinal detachment, corneal fluid buildup, and infection.
- Some patients may require additional surgery.
Preventing and Reducing the Progression of Diabetic Retinopathy
- Regular Monitoring: Attending routine diabetic eye screening appointments.
- Lifestyle Management: Controlling blood sugar, blood pressure, and cholesterol through diet, exercise, and prescribed medications.
- Quick Response to Symptoms: Reporting vision changes, floaters, or pain promptly.
Proper management, early detection, and timely treatment can significantly improve outcomes for individuals with diabetic retinopathy, preventing severe vision loss and complications.
Preventing Diabetic Retinopathy
Diabetic retinopathy is a serious complication of diabetes that affects the eyes, but it can often be prevented or its progression slowed down through effective management of diabetes and lifestyle adjustments.
Key Prevention Strategies
Control Blood Sugar Levels
- Lifestyle Choices: Maintaining balanced blood sugar levels is essential. Eating a balanced diet low in sugar and refined carbohydrates and exercising regularly helps to keep blood glucose in check.
- Monitoring: Regular blood sugar monitoring at home and through HbA1c tests helps to gauge your average blood glucose over the past weeks.
- HbA1c Target: For most people with diabetes, a target HbA1c of around 48 mmol/l (6.5%) is recommended.
- Medication: If lifestyle changes aren’t sufficient, you may need insulin or oral diabetes medications like metformin to regulate blood sugar.
Keep Blood Pressure and Cholesterol Under Control
- Blood Pressure Goals: The recommended target for people with diabetes is 140/80mmHg or lower. For those with complications like eye damage, a lower target (130/80mmHg) is advised.
- Cholesterol Levels: Aim for a total blood cholesterol level of no more than 4 mmol/l. Statins may be prescribed if needed.
Healthy Lifestyle Choices
- Balanced Diet: Focus on eating a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting salt, sugar, and saturated fat intake.
- Exercise Regularly: Aim for at least 150 minutes of moderate-intensity activity weekly, such as brisk walking or cycling.
- Quit Smoking: Smoking can worsen diabetes complications, including retinopathy. Seek support to quit smoking if needed.
- Limit Alcohol Consumption: Stick to recommended guidelines of no more than 14 alcohol units per week for both men and women.
Know and Monitor Your Levels
- Blood Sugar: Regular monitoring and working with your diabetes care team to set and achieve target levels.
- Blood Pressure: Check at home or at your GP surgery to ensure it stays within recommended limits.
- Cholesterol: Get routine blood tests and work with your GP to keep levels within recommended ranges.
Attend Regular Screening
- Annual Diabetic Eye Screening: Everyone with diabetes aged 12 and over should attend annual screenings. This can detect early signs of retinopathy before symptoms arise, allowing for timely treatment and prevention of further damage.
- Contact Your Optician: Report any sudden or gradual changes in vision, such as:
- Gradual vision loss
- Sudden vision loss
- Shapes or “floaters” in your vision
- Blurred vision
- Eye pain or redness These symptoms may not always indicate diabetic retinopathy but should be evaluated promptly.
Importance of Early Detection
- Early detection of diabetic retinopathy greatly increases the chances of preventing progression and preserving vision. Lifestyle modifications, medication, and regular monitoring are crucial tools to maintain eye health and overall well-being.