About chronic kidney disease
What is Chronic Kidney Disease (CKD)?
Chronic kidney disease is a long-term condition characterized by the kidneys’ reduced ability to perform their essential functions effectively. The condition progresses over time and, in most cases, is detected through routine blood and urine tests before any noticeable symptoms occur.
Symptoms of Advanced CKD
CKD often does not present symptoms until it reaches a more advanced stage. Key signs of advanced kidney disease may include:
- Tiredness and Fatigue: Persistent exhaustion not alleviated by rest.
- Swelling: Fluid retention leading to swollen ankles, feet, or hands.
- Shortness of Breath: Caused by fluid build-up in the lungs.
- Nausea: Feelings of sickness and discomfort in the stomach.
- Blood in the Urine: A visible symptom of kidney dysfunction.
Diagnosing CKD
CKD is typically diagnosed through blood and urine tests. Testing is often recommended annually for individuals at higher risk, including those with:
- High Blood Pressure (Hypertension)
- Diabetes
- Family History of CKD
How Kidneys Work
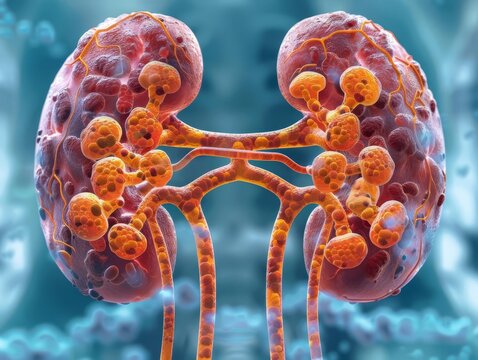
The kidneys, two bean-shaped organs located below the ribcage, have crucial roles in:
- Filtering Blood: Removing waste products and converting them into urine.
- Regulating Blood Pressure: Maintaining balance in fluid and electrolyte levels.
- Vitamin D Production: Assisting in bone health.
- Red Blood Cell Production: Releasing erythropoietin to stimulate red blood cell production.
Causes of CKD
CKD is often due to damage from underlying conditions such as:
- Diabetes: High blood sugar levels can harm kidney structures over time.
- High Blood Pressure: Consistently high blood pressure can strain the kidneys, affecting their efficiency.
Who is Affected by CKD?
CKD is common among older adults and is associated with age-related changes. Specific demographics, such as people of South Asian and African or Caribbean descent, are at higher risk due to a greater prevalence of diabetes and hypertension in these populations. In people aged 65 to 74, about 1 in 5 men and 1 in 4 women have some degree of CKD.
Treatment for CKD
While there is no cure for CKD, treatments can slow or stop the disease’s progression and help manage associated health risks. These include:
- Managing Blood Pressure and Diabetes: Controlling these conditions helps protect kidney health.
- Lifestyle Changes: Adopting a healthy diet, staying physically active, limiting alcohol intake, and avoiding nephrotoxic medications.
- Dialysis and Transplants: In cases where CKD progresses to end-stage renal failure, patients may require dialysis or a kidney transplant.
Living with CKD
CKD can be challenging, but resources and support systems are available to help patients manage the condition, including dietary counseling, mental health support, and practical guidance for daily life adjustments.
Preventing CKD
Preventive measures to reduce CKD risk involve:
- Managing Chronic Conditions: Keeping diabetes and blood pressure in check.
- Healthy Lifestyle: Eating well, exercising, avoiding excessive alcohol consumption, and being cautious with medications that may affect kidney health.
Living with CKD requires ongoing medical attention and lifestyle adjustments, but effective management can slow disease progression and improve the quality of life for individuals affected by this chronic condition.
Symptoms of chronic kidney disease
Chronic kidney disease (CKD) often presents few to no symptoms in its early stages, making routine testing crucial for detection. This is because the body can often tolerate a significant reduction in kidney function without immediate signs of distress. This resilience is why individuals can live well with just one functioning kidney.
Symptoms of Advanced CKD and Kidney Failure
When CKD progresses and kidney function declines significantly, a variety of symptoms may emerge, signaling a need for medical attention and ongoing management. These symptoms include:
Common Symptoms
- Weight Loss and Poor Appetite: A reduction in body weight and changes in appetite are often early signs of worsening kidney function.
- Swelling (Edema): Fluid retention can lead to swollen ankles, feet, or hands, indicating an imbalance in the body’s ability to remove excess fluid.
- Shortness of Breath: Fluid accumulation in the lungs, a condition known as pulmonary edema, may cause difficulty breathing.
- Changes in Urination: An increased need to urinate, especially at night, or the presence of blood or protein in urine (proteinuria). Note that protein in urine can only be detected through testing.
- Insomnia: Difficulty sleeping may arise due to itching, discomfort, or other systemic effects of impaired kidney function.
- Itchy Skin: Persistent itching can be linked to a buildup of waste products in the bloodstream, which the kidneys can no longer effectively filter out.
- Muscle Cramps: Electrolyte imbalances, including low calcium and high phosphorus levels, can lead to muscle cramps.
- High Blood Pressure (Hypertension): The kidneys play a critical role in regulating blood pressure; damaged kidneys may lead to elevated blood pressure levels.
- Nausea: The buildup of toxins that the kidneys fail to filter may cause nausea and vomiting.
- Erectile Dysfunction in Men: Men with CKD may experience difficulties in maintaining or achieving an erection due to hormonal changes and circulatory issues.
Why Symptoms May Go Unnoticed
Many symptoms of CKD are general and can be attributed to other, less severe conditions. Because of this, regular monitoring and testing are critical to catching CKD early, often before symptoms even appear.
Monitoring and Treatment
Routine blood and urine tests are essential for individuals diagnosed with CKD to monitor kidney function and detect any progression toward kidney failure (also known as established renal failure or ERF). Early detection and treatment can help minimize symptoms, slow disease progression, and improve overall quality of life.
If you experience any of these symptoms, it’s important to consult with your GP or healthcare provider to rule out CKD or other potential conditions and receive appropriate care.
Causes of chronic kidney disease
Chronic kidney disease (CKD) is caused by various conditions that place excessive strain on the kidneys, leading to gradual deterioration of their function over time. Here are the primary and additional causes of CKD:
1. High Blood Pressure (Hypertension)
- Overview: High blood pressure is a major cause of kidney disease. It refers to the force exerted by the blood against the walls of the arteries. When this pressure is consistently too high, it can damage the delicate blood vessels in the kidneys, impairing their ability to filter waste from the blood.
- Risk Factors for High Blood Pressure:
- Age: The risk of developing hypertension increases with age.
- Family History: Hypertension often runs in families.
- Ethnicity: Individuals of African-Caribbean or South Asian descent are at higher risk.
- Lifestyle Factors: Obesity, smoking, lack of exercise, excessive alcohol intake, high salt consumption, a high-fat diet, and stress are all known contributors to high blood pressure.
- Kidney Impact: Hypertension can damage the small blood vessels in the kidneys, hindering the filtering process and causing further decline in kidney function.
2. Diabetes
- Overview: Diabetes, characterized by high blood glucose levels, is another leading cause of CKD. It is classified into two types:
- Type 1 Diabetes: The body produces little or no insulin.
- Type 2 Diabetes: The body becomes resistant to insulin or doesn’t produce enough insulin.
- Impact on the Kidneys: When blood glucose levels remain uncontrolled, excess glucose can damage the kidneys’ tiny filtering units (glomeruli), causing a decline in their ability to filter waste and excess fluids from the body.
- Statistics:
- Up to 40% of people with type 1 diabetes will develop kidney disease before the age of 50.
- Approximately 30% of those with type 2 diabetes are at risk of developing kidney damage.
- Early Detection: The first sign of diabetic kidney disease is the presence of low levels of protein in the urine (proteinuria). Regular annual kidney function checks are essential for people with diabetes to detect and manage any signs of kidney disease early.
3. Other Causes of CKD
- Glomerulonephritis: Inflammation of the kidney’s filtering units (glomeruli).
- Pyelonephritis: Kidney infection that can cause scarring and damage to the kidneys over time.
- Polycystic Kidney Disease: An inherited condition in which multiple cysts grow in the kidneys, gradually enlarging them and impairing their function.
- Congenital Malformations: Abnormal kidney development in the womb may lead to reduced kidney function from birth.
- Systemic Lupus Erythematosus (Lupus): An autoimmune disease in which the body’s immune system attacks its own tissues, including the kidneys.
- Long-Term Medication Use:
- Lithium: Used to treat certain psychiatric disorders, which may cause kidney damage with long-term use.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Regular use of pain relievers like aspirin and ibuprofen can potentially harm the kidneys, particularly when used long-term.
- Obstructions: Conditions like kidney stones or prostate disease can block urine flow and lead to kidney damage.
Prevention and Management
- Control of Underlying Conditions: Proper management of diabetes and hypertension is critical to reducing the risk and progression of CKD.
- Lifestyle Changes: Eating a balanced diet, exercising regularly, maintaining a healthy weight, limiting salt and alcohol intake, and avoiding smoking can help protect the kidneys.
- Medication Monitoring: Avoiding excessive use of nephrotoxic drugs and working with healthcare professionals to manage existing conditions can help reduce kidney disease progression.
Addressing the root causes and managing risk factors is key to slowing or preventing the progression of chronic kidney disease and maintaining overall kidney health.
Diagnosis of chronic kidney disease
Diagnosing chronic kidney disease (CKD) involves various tests and assessments to determine the functioning of the kidneys. Here is a detailed overview of how CKD is diagnosed and the different tests involved:
Screening for CKD
Routine screening is recommended for individuals who are at a higher risk of developing CKD. Regular screening may include annual blood and urine tests. High-risk groups include:
- People with high blood pressure (hypertension)
- People with diabetes
- Individuals with a history of acute kidney injury (caused by medications such as lithium or NSAIDs, kidney stones, or an enlarged prostate)
- People with cardiovascular diseases (like coronary heart disease or heart failure)
- Family history of stage 5 CKD or inherited kidney diseases
- Individuals with systemic diseases that may affect the kidneys (e.g., systemic lupus erythematosus)
- Patients with unexplained blood (haematuria) or protein (proteinuria) in their urine
Glomerular Filtration Rate (GFR)
The glomerular filtration rate (GFR) measures how well the kidneys are filtering waste products from the blood. An effective way to assess kidney function, the GFR measures the amount of fluid the kidneys filter per minute (ml/min). A healthy pair of kidneys typically filters more than 90 ml/min.
- eGFR (Estimated GFR): Calculated using a blood sample to measure creatinine levels, along with age, gender, and ethnic background. The eGFR is expressed as a percentage of normal kidney function. For example, an eGFR of 50 ml/min indicates 50% kidney function.
Urine Tests
- General urine tests: These detect blood or protein in the urine.
- Albumin-Creatinine Ratio (ACR): This test measures the ratio of albumin (a type of protein) to creatinine in the urine. Combined with eGFR results, the ACR helps doctors evaluate kidney function more accurately.
Staging of CKD
CKD is categorized into six stages based on eGFR levels. The higher the stage, the more severe the disease:
- Stage 1 (G1): eGFR of 90 or higher. Kidneys are functioning normally, but there is evidence of damage. Annual eGFR tests are recommended.
- Stage 2 (G2): eGFR of 60 to 89. Kidney function is slightly reduced but still within normal ranges for younger adults. Annual monitoring is suggested.
- Stage 3a (G3a): eGFR of 45 to 59. This indicates mild to moderate reduction in function, requiring annual checks.
- Stage 3b (G3b): eGFR of 30 to 44. This suggests a moderate to severe reduction in function, necessitating testing every six months.
- Stage 4 (G4): eGFR of 15 to 29. There is severe reduction in kidney function. Symptoms of CKD may be present. Monitoring every six months is recommended.
- Stage 5 (G5): eGFR below 15. This stage, known as established renal failure, involves frequent testing every three months.
Note: GFR can fluctuate, so a single abnormal result doesn’t necessarily confirm CKD. Diagnosis requires repeated tests over at least three months showing consistently low eGFR.
Additional Tests
- Kidney Imaging:
- Ultrasound, MRI, or CT scans: Used to detect any blockages in urine flow or abnormal kidney shapes, particularly in advanced cases.
- Kidney Size: Advanced CKD often leads to shrinkage and an uneven shape of the kidneys.
- Kidney Biopsy: A small tissue sample from the kidney is examined under a microscope to assess cellular damage and identify the cause of kidney dysfunction.
Monitoring and Follow-Up
- Blood Pressure Management: Regular monitoring of blood pressure is crucial as hypertension can exacerbate kidney damage.
- Routine Blood Tests: Ongoing blood tests to monitor creatinine levels, electrolyte balance, and overall kidney function.
- Monitoring Urinary Changes: Any changes in urinary protein levels, blood presence, or other abnormalities are noted for further evaluation.
Importance of Early Detection
Early diagnosis of CKD is vital for effective management and prevention of further kidney damage. It allows for interventions that can slow disease progression, manage symptoms, and reduce the risk of complications, such as cardiovascular disease. If you are at risk or have concerns, speaking with a healthcare provider for appropriate testing and diagnosis is essential.
Treating chronic kidney disease
Treatment for chronic kidney disease (CKD) focuses on slowing the progression of the disease, managing symptoms, and reducing the risk of complications. Here is a detailed overview of treatment strategies:
Lifestyle Changes
Adopting healthy lifestyle habits can significantly reduce blood pressure, improve kidney function, and help manage CKD symptoms. These changes include:
- Stop Smoking: Smoking can damage blood vessels and reduce kidney function. Quitting smoking helps improve overall health.
- Healthy Diet: Follow a low-fat, balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Salt Restriction: Limit salt intake to less than 6g per day (about one teaspoon) to control blood pressure.
- Limit NSAIDs: Avoid over-the-counter NSAIDs like ibuprofen unless advised by a healthcare professional, as they can worsen kidney function.
- Moderate Alcohol Intake: Limit alcohol consumption to recommended levels.
- Weight Management: Losing excess weight helps lower blood pressure and reduce the strain on kidneys.
- Regular Exercise: Aim for at least 30 minutes of moderate exercise five times per week to improve overall health and reduce blood pressure.
Medications for High Blood Pressure
Controlling blood pressure is critical for slowing the progression of CKD. Target blood pressure goals are:
- Below 140/90 mmHg for people with CKD.
- Below 130/80 mmHg for individuals with CKD and diabetes.
Angiotensin-Converting Enzyme (ACE) Inhibitors are commonly prescribed to manage blood pressure and offer additional kidney protection. Examples include:
- Ramipril
- Enalapril
- Lisinopril
- Perindopril
Side Effects of ACE Inhibitors: These may include dry cough, dizziness, fatigue, and headaches. If side effects are problematic, an alternative medication, Angiotensin-II Receptor Blockers (ARBs), may be used, such as:
- Candesartan
- Losartan
- Valsartan
Monitoring: Blood tests are necessary to monitor kidney function and potassium levels during treatment.
Medication to Reduce Cholesterol
People with CKD are at increased risk for cardiovascular diseases. Statins may be prescribed to lower cholesterol levels, reducing the risk of heart attacks and strokes. Common statins include:
- Simvastatin
- Atorvastatin
Side Effects of Statins: These may include constipation, diarrhoea, headaches, and occasional muscle pain.
Fluid and Salt Management
Depending on kidney function, some individuals may need to:
- Limit fluid intake to prevent fluid buildup.
- Use diuretics (water tablets), such as furosemide, to reduce fluid retention if necessary.
Managing Anaemia
Anaemia is common in advanced CKD due to a lack of red blood cells. Treatment may include:
- Iron Supplements: Taken as tablets or given through intravenous infusions.
- Erythropoietin Injections: These stimulate red blood cell production.
Correcting Phosphate Balance
In stages 4 and 5 CKD, excess phosphate can build up, leading to bone and cardiovascular problems. Management options include:
- Dietary Phosphate Restriction: Limit red meat, dairy, eggs, and fish intake.
- Phosphate Binders: Medicines like calcium carbonate are taken before meals to reduce phosphate absorption.
Side Effects of Phosphate Binders: These may include nausea, stomach pain, constipation, diarrhoea, and itchy skin.
Vitamin D Supplements
People with CKD may need vitamin D supplements to support bone health, as their kidneys cannot activate vitamin D properly.
Treatment for Kidney Failure: Dialysis or Transplant
When kidney function declines to a life-threatening level (end-stage renal failure), options include:
- Dialysis: A process that removes waste and excess fluid from the blood. It can be done through:
- Haemodialysis (using a machine to filter the blood)
- Peritoneal Dialysis (using the lining of the abdomen to filter the blood)
- Kidney Transplant: A healthy kidney from a donor is surgically placed into the patient. It can come from a living or deceased donor.
Supportive Treatment
For those who choose not to pursue dialysis or transplantation, supportive (palliative) care focuses on symptom management and quality of life. This includes:
- Medicines for symptom relief (e.g., breathlessness, itching)
- Emotional and practical support for both patients and families
- Planning for end-of-life care if necessary
Care Planning and Regular Reviews
Treatment and care plans should be regularly reviewed to adapt to changing needs. Discussing and creating a care plan with healthcare professionals, including kidney disease specialist nurses, can help you manage day-to-day health.
Effective management of CKD often involves a combination of lifestyle changes, medication, and ongoing monitoring to slow disease progression and improve quality of life. If you are diagnosed with CKD, working closely with your healthcare team is essential to manage your condition effectively.
Preventing chronic kidney disease
Preventing chronic kidney disease (CKD) focuses on adopting healthy lifestyle habits and managing any existing conditions that could lead to kidney problems. Here are detailed strategies to reduce the risk of CKD:
1. Managing Chronic Conditions
If you have a long-term condition like diabetes or high blood pressure, it’s vital to manage it carefully. Effective control of these conditions can prevent kidney damage. You can do this by:
- Following Medical Advice: Keep all medical appointments and follow your GP’s recommendations for medications and lifestyle adjustments.
- Annual Kidney Function Testing for Diabetes Patients: People with diabetes are advised to have their kidney function tested every year to monitor for signs of kidney damage.
2. Stop Smoking
Smoking can worsen existing kidney problems and increase the risk of cardiovascular disease, which contributes to kidney damage. Quitting smoking offers a range of health benefits:
- Reduces Risk: Lowers the chances of heart attacks, strokes, and kidney disease progression.
- Access Help: Contact the NHS smoking helpline for support, or call Quit Your Way Scotland at 0800 84 84 84 for encouragement and advice on quitting.
3. Healthy Diet
Eating a balanced diet helps maintain overall health and supports kidney function. Follow these dietary tips:
- Eat a Variety of Foods: Include fresh fruits, vegetables (aim for 5 servings a day), and whole grains.
- Limit Salt Intake: Consuming more than 6g (0.2oz) of salt per day can raise blood pressure. Avoid adding extra salt to meals and check food labels for hidden sodium.
- Reduce Saturated Fat: High levels of cholesterol can harm the heart and kidneys. Limit foods like:
- Meat pies, sausages, and fatty cuts of meat
- Butter, ghee, and lard
- Cream and hard cheese
- Cakes, biscuits, and foods containing coconut or palm oil
- Eat Unsaturated Fats: Healthy fats can reduce cholesterol. Include foods like:
- Oily fish (such as salmon or mackerel)
- Avocados
- Nuts and seeds
- Sunflower, rapeseed, and olive oils
4. Limit Alcohol Consumption
Excessive alcohol can lead to high blood pressure and increased cholesterol levels, both of which negatively impact the kidneys. Stick to recommended limits:
- Moderation is Key: The NHS recommends no more than 14 units of alcohol per week for adults, spread across several days.
5. Exercise Regularly
Physical activity helps lower blood pressure and improve heart and kidney health. Aim for:
- 150 Minutes Weekly: Engage in at least 2 hours and 30 minutes of moderate-intensity aerobic exercise (e.g., brisk walking or cycling) every week.
6. Proper Use of Painkillers
Some non-steroidal anti-inflammatory drugs (NSAIDs), like ibuprofen and aspirin, can harm the kidneys if used improperly.
- Follow Instructions Carefully: Use NSAIDs only as directed and avoid prolonged use unless prescribed by a healthcare provider.
Additional Tips for Prevention
- Maintain a Healthy Weight: Being overweight increases the risk of diabetes and high blood pressure, both of which can lead to CKD.
- Stay Hydrated: Drinking adequate water supports kidney function, but avoid excessive fluid intake unless recommended.
- Regular Check-Ups: If you have a family history of kidney disease, high blood pressure, or other risk factors, routine screening and early detection are essential.
By making these lifestyle changes and managing any underlying conditions, you can significantly lower your risk of developing chronic kidney disease and improve overall health.
Living with Chronic Kidney Disease (CKD)
Relationships and Support
Dealing with a chronic condition like CKD can have a significant emotional impact on you, your family, and friends. It may be challenging to open up about your condition, even with those close to you. Educating yourself and your loved ones about CKD can be empowering, helping everyone feel more in control and less overwhelmed by the disease’s demands.
- Communicate Openly: Sharing your thoughts and feelings with your family and friends can strengthen relationships and help them understand how best to support you.
- Seek Support: Consider reaching out to your GP, nurse, or a trained counselor for guidance. You may also find comfort in joining local support groups or online forums where you can connect with others facing similar challenges.
Managing Finances
CKD can sometimes impact your ability to work full-time, creating financial stress. Fortunately, there are various types of financial support you may be eligible for:
- Statutory Sick Pay: If you’re employed but unable to work due to illness.
- Employment and Support Allowance: If you’re not employed and can’t work.
- Disability Living Allowance or Attendance Allowance: If you have mobility or personal care needs.
- Carer’s Allowance: If you are caring for someone with CKD.
Sex and Pregnancy
CKD and its associated stress can sometimes affect sexual relationships. Communicating with your partner about your feelings and seeking advice from a counselor or sex therapist can help maintain intimacy. Dialysis patients may experience specific sexual difficulties, such as decreased libido and erectile dysfunction, which can be addressed with appropriate treatment.
- Pregnancy Considerations: Women with CKD should consult their healthcare team before trying to conceive, as CKD can pose risks to both the mother and baby. Men with advanced CKD may also experience reduced fertility. Effective contraception is recommended unless pregnancy is planned.
Traveling and Insurance
Travel is possible with CKD, but it may require additional planning:
- Dialysis Patients: Arrange for dialysis treatments in advance if traveling. Your renal unit can help with planning.
- Insurance: Make sure to declare CKD as a pre-existing condition when applying for travel insurance to ensure you’re properly covered.
Using Over-the-Counter Medicines
Certain over-the-counter (OTC) medications can be harmful to people with CKD. Always check with your healthcare provider before taking any new medication.
- Headaches: Paracetamol is generally safe, but avoid soluble versions (high in sodium) and NSAIDs like ibuprofen or aspirin if kidney function is impaired.
- Coughs and Colds: Many cold remedies contain ingredients that may not be suitable for people with CKD. Opt for simple linctuses or steam inhalation.
- Muscle and Joint Pain: Topical treatments are safer than NSAIDs taken orally.
Kidney Failure and Treatment Options
About 1% of people with stage 3 CKD may develop kidney failure, also known as established renal failure (ERF). Options for managing ERF include:
- Dialysis: This treatment filters waste and excess fluid from the blood. There are two main types of dialysis:
- Peritoneal Dialysis: Performed at home using the lining of the abdomen to filter the blood.
- Haemodialysis: Blood is filtered through a machine, usually performed in a hospital or at home.
- Kidney Transplant: Offers the best long-term outcome for many patients but is only suitable for some.
- Supportive Care: Focuses on managing symptoms without dialysis or transplantation.
Your healthcare team will work closely with you to decide the best treatment plan.
Quality of Life Considerations
Living with CKD involves making lifestyle adjustments and managing symptoms effectively to maintain your quality of life. Supportive care, ongoing communication with healthcare professionals, and a proactive approach to managing CKD can help you lead a fulfilling life.