Introduction
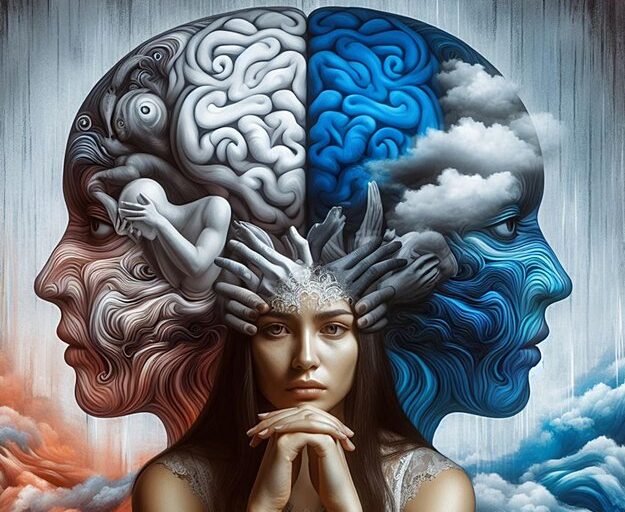
Bipolar disorder is a complex mental health condition characterized by extreme mood swings, including emotional highs (mania or hypomania) and lows (depression). These mood episodes are more severe and prolonged than typical mood fluctuations and can significantly impact daily functioning and overall quality of life.
Symptoms of Bipolar Disorder
1. Depression Episodes:
- Feelings of extreme sadness or hopelessness
- Loss of interest in activities once enjoyed
- Difficulty concentrating or making decisions
- Fatigue and lethargy
- Changes in appetite and weight (either loss or gain)
- Feelings of worthlessness or guilt
- Thoughts of death or suicide
2. Mania Episodes:
- Elevated mood, euphoria, or irritability
- Increased energy and activity levels
- Rapid speech and racing thoughts
- Decreased need for sleep without feeling tired
- Grandiose ideas and inflated self-esteem
- Impulsive or risky behavior (e.g., excessive spending, unwise investments)
- Hypersexuality
- Delusions or hallucinations (in more severe cases)
3. Hypomania:
- Milder form of mania that does not include psychotic features
- Increased energy and productivity, but symptoms do not disrupt daily life to the extent of mania
Living with Bipolar Disorder
People living with bipolar disorder often experience extreme disruptions to their personal and professional lives, but appropriate treatment and lifestyle adjustments can significantly reduce the impact of symptoms.
Treatment Options:
- Medication: Mood stabilizers (e.g., lithium), antipsychotic medications, and antidepressants tailored to individual needs
- Psychological Therapy: Cognitive behavioral therapy (CBT), psychoeducation, and family therapy can help individuals and their families understand the condition, recognize triggers, and learn coping strategies
- Lifestyle Modifications: Regular exercise, a balanced diet, good sleep hygiene, stress reduction techniques, and a stable daily routine
- Support Systems: Community groups, online forums, and support from mental health professionals or peers living with bipolar disorder can offer invaluable support
Causes and Risk Factors
Bipolar disorder has no singular cause. It is believed to be influenced by a combination of genetic, biochemical, and environmental factors:
- Genetics: A family history of bipolar disorder or other mental health conditions increases the likelihood of developing the disorder.
- Brain Chemistry: Imbalances in neurotransmitters, such as serotonin and dopamine, are thought to play a role.
- Life Events: Stressful or traumatic life experiences may trigger episodes in susceptible individuals.
Managing Bipolar Disorder
1. Medication Adherence:
- Taking prescribed medications as directed, even when feeling well, is crucial to maintaining stability and preventing relapses.
2. Recognizing Triggers:
- Identifying triggers, such as changes in sleep patterns, stress, or seasonal shifts, can help individuals preemptively manage episodes.
3. Building a Support Network:
- Friends, family, healthcare providers, and mental health professionals can offer essential emotional support and guidance.
4. Regular Monitoring:
- Keeping a mood diary or regularly checking in with a healthcare provider can help track symptoms and detect early signs of mood changes.
Pregnancy and Bipolar Disorder
Pregnancy can exacerbate symptoms of bipolar disorder due to hormonal fluctuations, changes in medication, and the stress of impending parenthood. Working closely with healthcare professionals is vital to managing the condition during this period.
Bipolar Disorder Statistics and Prevalence
- Bipolar disorder affects approximately 1% of the adult population.
- It typically emerges in late adolescence or early adulthood, though it can develop at any age.
- Men and women are equally affected by bipolar disorder, but patterns of symptoms may differ.
Bipolar Disorder in Different People
The course and pattern of bipolar disorder can vary widely:
- Some individuals experience rapid cycling, where four or more episodes of mania or depression occur within a year.
- Others may have long periods of stable mood between episodes.
Bipolar disorder is a lifelong condition, but with effective treatment, individuals can lead full and productive lives. For those affected, finding the right combination of medical, psychological, and social support is crucial for stability and well-being.
Symptoms
Bipolar disorder is characterized by episodes of extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). It can significantly impact daily life, relationships, and overall well-being. Here’s a closer look at the symptoms and their impact:
Symptoms of Bipolar Disorder
Depression Phase
During a depressive episode, a person with bipolar disorder may experience symptoms such as:
- Persistent feelings of sadness, hopelessness, or irritability: Often lasting for weeks or months.
- Low energy levels: Individuals may feel fatigued, lethargic, and unable to engage in everyday tasks.
- Difficulty concentrating or making decisions: Even simple tasks can become overwhelming, and it may be challenging to focus.
- Loss of interest or pleasure in activities: Hobbies, social interactions, and work may no longer hold any appeal.
- Feelings of worthlessness or excessive guilt: People may feel unworthy, regretful, or overwhelmed by guilt.
- Pessimism or negative thoughts: Constantly expecting the worst or believing things will never improve.
- Self-doubt and low self-esteem: Constantly questioning one’s abilities and doubting oneself.
- Changes in appetite: This can include loss of appetite, overeating, or changes in weight.
- Difficulty sleeping: This may involve insomnia, waking up early, or oversleeping.
- Thoughts of death or suicide: Suicidal ideation is a serious symptom that requires immediate medical attention.
- Delusions and hallucinations (psychotic symptoms): In severe cases, people may experience false beliefs (delusions) or see and hear things that aren’t there (hallucinations).
Mania Phase
During a manic episode, individuals may display symptoms such as:
- Extreme happiness, elation, or a sense of euphoria: Feeling overly joyous, confident, or on top of the world.
- Rapid speech and racing thoughts: The mind moves quickly from one idea to another, and speech may become pressured.
- Increased energy and reduced need for sleep: Often going without sleep for extended periods without feeling tired.
- Feelings of self-importance and grandiosity: Unrealistically high self-esteem, believing they have special abilities or important tasks to accomplish.
- Easily distracted and impulsive behavior: Struggling to focus on tasks and making impulsive decisions without considering consequences.
- Irritability and agitation: Becoming quickly annoyed or frustrated, even with minor issues.
- Psychotic symptoms: Experiencing delusions, such as having special powers, or hallucinations.
- Engaging in risky behavior: Excessive spending, impulsive sexual activity, substance misuse, or reckless activities.
Patterns and Variations
Bipolar disorder symptoms can vary from person to person, and the frequency and severity of episodes differ:
- Episodes may last for weeks or months and may occur infrequently or multiple times in a year.
- Periods of normal mood may be present between episodes, but some people may have rapid cycling, where they move quickly from mania to depression.
- Mixed states: It’s possible to have symptoms of both mania and depression at the same time, such as feeling sad but having high energy levels.
Types of Bipolar Disorder
- Bipolar I Disorder: Characterized by manic episodes that last at least seven days or severe symptoms that require hospitalization. Depressive episodes often occur as well, typically lasting at least two weeks.
- Bipolar II Disorder: Defined by a pattern of depressive episodes and hypomanic episodes (a less severe form of mania), but not the full-blown manic episodes that are typical of Bipolar I.
- Cyclothymic Disorder: Periods of hypomanic symptoms and periods of depressive symptoms lasting for at least two years (one year in children and adolescents) but not meeting the diagnostic criteria for a manic episode or major depressive episode.
Living with Bipolar Disorder
Bipolar disorder can be highly disruptive, affecting relationships, employment, and self-care. During episodes, individuals may:
- Struggle to recognize their behavior as abnormal during manic episodes, leading to denial of the problem or rejection of help.
- Feel regret or shame after manic episodes due to impulsive decisions or risky behavior.
- Experience psychotic symptoms during severe episodes, requiring specialized treatment.
Treatment and Management
Treatment for bipolar disorder focuses on stabilizing mood and includes:
- Medication: Mood stabilizers, antipsychotic medications, antidepressants, and medications to manage sleep and anxiety.
- Psychotherapy: Cognitive-behavioral therapy (CBT) and psychoeducation can help individuals understand and manage their condition.
- Lifestyle changes: Regular exercise, consistent sleep schedules, stress management, and avoiding drugs or alcohol are crucial for stability.
- Support networks: Friends, family, and support groups can play an essential role in providing encouragement and understanding.
Bipolar disorder is a lifelong condition that can be managed effectively with the right combination of treatments and support systems, enabling people to lead fulfilling lives.
Causes
The causes of bipolar disorder are not completely understood, but research suggests that a combination of factors, including biological, genetic, and environmental elements, contributes to the development of the condition. Here is a detailed overview of what is believed to cause bipolar disorder:
Chemical Imbalance in the Brain
One of the primary theories about the causes of bipolar disorder is that it involves chemical imbalances in the brain. These chemical messengers, known as neurotransmitters, are responsible for regulating mood and other important functions. The main neurotransmitters implicated in bipolar disorder are:
- Noradrenaline (norepinephrine): Elevated levels of noradrenaline are thought to contribute to manic episodes, while low levels may lead to depression.
- Serotonin: Imbalances in serotonin are believed to influence mood swings and are often linked to depression and other mood disorders.
- Dopamine: Variations in dopamine levels may play a role in mood regulation, potentially leading to symptoms of mania and depression.
Research has found that the function and interaction of these neurotransmitters may be altered in people with bipolar disorder. Although the precise mechanisms remain unclear, this imbalance may contribute to the extreme mood swings experienced in the disorder.
Genetic Factors
There is strong evidence suggesting that genetics play a role in the development of bipolar disorder. The condition tends to run in families, with first-degree relatives (such as parents or siblings) of a person with bipolar disorder being at higher risk of developing the condition themselves. However, it is not caused by a single gene but likely involves multiple genetic factors interacting with one another and with environmental factors.
Studies have identified certain genes that may be linked to bipolar disorder, but no single gene has been proven to directly cause the condition. This suggests that genetic susceptibility, combined with other factors, may be a key component in its development.
Environmental and Social Triggers
Environmental factors and life events can act as triggers for bipolar episodes, particularly in individuals who are predisposed to the condition due to genetic or biological factors. Some common triggers include:
- Stressful life events: Significant stressors such as the loss of a loved one, the end of a relationship, or significant changes in life circumstances can precipitate episodes of mania or depression.
- Trauma: Experiencing physical, sexual, or emotional abuse, particularly in childhood, has been associated with an increased risk of developing bipolar disorder.
- Major life changes: Events such as moving to a new place, starting a new job, or having a baby may act as triggers, particularly if they cause significant stress or disruption to normal routines.
- Sleep disturbances: Disruption of normal sleep patterns, such as insomnia or changes in routine, is a known trigger for mood episodes in people with bipolar disorder.
- Physical illness: Certain physical health conditions and chronic illnesses may increase the likelihood of developing bipolar symptoms.
- Substance misuse: Alcohol or drug use can worsen the symptoms of bipolar disorder and may trigger episodes of mania or depression.
Complex Interactions and Triggers
The interplay of biological predisposition, genetic risk, and environmental factors creates a complex picture of the causes of bipolar disorder. No single factor is thought to be solely responsible for causing the disorder, and different people may have different contributing factors or triggers.
Stress-Vulnerability Model
One commonly accepted framework for understanding bipolar disorder is the stress-vulnerability model, which suggests that individuals have varying levels of genetic or biological vulnerability to developing the condition. When combined with environmental stressors or significant life events, this vulnerability may lead to the onset or worsening of symptoms.
In conclusion, while the precise cause of bipolar disorder is not fully understood, it is widely believed to result from a combination of biological, genetic, and environmental factors that interact in complex ways. Treatment approaches often consider these various influences to help individuals manage and cope with the disorder effectively.
Diagnosis
Diagnosing bipolar disorder involves a careful and comprehensive evaluation by a medical professional, usually a psychiatrist. The goal of diagnosis is to determine whether the symptoms being experienced are consistent with bipolar disorder and to rule out other possible causes. Here is an overview of what to expect during the diagnosis process:
GP Assessment and Referral
- If you suspect you have bipolar disorder, your first step is usually to visit your GP (general practitioner).
- Your GP will ask you about your symptoms, including when they started, how long they last, and their impact on your daily life.
- If your symptoms suggest a possible diagnosis of bipolar disorder, your GP will refer you to a psychiatrist, a doctor who specializes in mental health disorders.
- In cases where there is a risk of self-harm or harm to others, the GP may arrange for urgent intervention and an immediate appointment with a specialist.
Specialist Psychiatric Assessment
- Psychiatric Evaluation: The psychiatrist will conduct a thorough assessment, asking about your symptoms of mania, hypomania, and depression. They will ask you to describe your experiences in detail, including mood swings, changes in energy levels, behavior, and thoughts during episodes.
- Symptom History: They will ask about when you first started experiencing symptoms, how severe they were, and how often they occur. They may also inquire about how long each episode lasts.
- Risk Assessment: The psychiatrist will assess whether you have ever had thoughts of self-harm or suicidal thoughts. They may also ask whether you have experienced any psychotic symptoms, such as hallucinations or delusions.
- Family History: The psychiatrist will ask whether any of your family members have been diagnosed with bipolar disorder or other mental health conditions. If there is a family history, they may request your permission to speak with them to gain a better understanding of your condition.
- Medical History: Information about your overall health, other medical conditions, medications you are taking, and substance use will be gathered as part of your evaluation.
Diagnostic Criteria
- The psychiatrist will evaluate your symptoms against the criteria outlined in diagnostic manuals such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or the International Classification of Diseases (ICD).
- To be diagnosed with bipolar disorder, you typically need to have experienced at least one episode of mania or hypomania, along with periods of depression.
- They will also determine the type of bipolar disorder you have (e.g., Bipolar I, Bipolar II, or Cyclothymic Disorder) based on the frequency and intensity of your mood episodes.
Other Tests to Rule Out Physical Causes
- The psychiatrist may request tests to rule out other potential causes of your symptoms. For example, blood tests may be done to check for conditions like thyroid dysfunction (either underactive thyroid [hypothyroidism] or overactive thyroid [hyperthyroidism]), as hormonal imbalances can cause symptoms similar to those of bipolar disorder.
- Brain scans or other medical tests may be performed if there is any concern about underlying neurological conditions or other physical health problems contributing to the symptoms.
Ongoing Monitoring and Physical Health Checks
- If diagnosed with bipolar disorder, you will need to see your GP or psychiatrist regularly for ongoing care and physical health monitoring.
- Regular health checks ensure that any physical health issues related to bipolar disorder or its treatments (such as weight gain, cardiovascular risk, or thyroid issues) are managed effectively.
Diagnosis Challenges and Special Considerations
- Differentiating from Other Disorders: The symptoms of bipolar disorder can overlap with those of other mental health conditions, such as depression, anxiety disorders, and personality disorders. Careful assessment is needed to differentiate between these conditions.
- Comorbidity: It is common for people with bipolar disorder to have other mental health conditions, such as anxiety disorders or substance use disorders. The psychiatrist will evaluate for these conditions during the assessment process.
By undergoing this comprehensive diagnostic process, individuals with bipolar disorder can receive an accurate diagnosis, which is essential for developing an effective treatment plan and managing their condition effectively over the long term.
Treatment
The primary goal of treatment for bipolar disorder is to manage the intensity, frequency, and duration of manic and depressive episodes, enabling individuals to lead a more stable and fulfilling life. Effective treatment can reduce mood swings and prevent relapse in most cases. The treatment plan typically includes a combination of medication, psychotherapy, lifestyle adjustments, and education to help individuals manage their condition.
Treatment Options for Bipolar Disorder
Medication
- Mood Stabilizers: These medications help prevent extreme highs (mania) and lows (depression) and are usually taken long-term. Commonly used mood stabilizers include:
- Lithium Carbonate: One of the oldest and most effective mood stabilizers, lithium helps reduce the frequency and severity of mania and can help prevent depression.
- Anticonvulsant Medicines: These are often used as mood stabilizers, such as valproate (Depakote), lamotrigine, and carbamazepine.
- Antipsychotic Medicines: These may be used to control mania or as a secondary treatment for depression in people with bipolar disorder. Examples include olanzapine, risperidone, quetiapine, and aripiprazole.
- Medications for Specific Episodes:
- Antidepressants: These may be used cautiously to treat depression but are often combined with a mood stabilizer or antipsychotic to avoid triggering mania.
- Benzodiazepines: Sometimes used short-term for severe anxiety, insomnia, or agitation.
Important Note: Medication regimens should be regularly monitored and adjusted by a healthcare professional, as individuals with bipolar disorder respond differently to various treatments.
- Mood Stabilizers: These medications help prevent extreme highs (mania) and lows (depression) and are usually taken long-term. Commonly used mood stabilizers include:
Psychological Treatment
- Cognitive Behavioral Therapy (CBT): This form of therapy helps people identify and change negative thinking patterns and behaviors. It also helps individuals develop coping strategies to manage stress, recognize triggers, and avoid relapses.
- Psychoeducation: Educating patients and their families about bipolar disorder, its symptoms, and its treatment options can empower individuals to manage their condition and seek help early if symptoms worsen.
- Interpersonal and Social Rhythm Therapy (IPSRT): This therapy focuses on stabilizing daily routines and sleep patterns, as maintaining a regular schedule is often helpful in managing bipolar disorder.
- Family Therapy: Family-focused therapy can help improve communication and problem-solving skills within the family unit, which can provide a supportive environment for the individual with bipolar disorder.
Learning to Recognize Triggers and Early Warning Signs
- Recognizing triggers for mania or depression is essential for individuals with bipolar disorder. Common triggers include stress, lack of sleep, substance use, and significant life changes.
- Mental Health Professionals, such as psychiatric nurses or social workers, can assist in creating an individualized plan to recognize and respond to these triggers early.
- Keeping a Mood Diary: This can help track mood changes and identify triggers or warning signs of impending episodes.
Lifestyle Changes
- Regular Exercise: Engaging in regular physical activity can improve mood, reduce stress, and promote better sleep.
- Sleep Hygiene: Maintaining a consistent sleep schedule is crucial, as disruptions in sleep can trigger mood episodes.
- Healthy Diet: A balanced diet, rich in nutrients, can support overall well-being and may help stabilize mood swings.
- Stress Reduction Techniques: Meditation, mindfulness, and other stress-relief methods can help manage triggers and reduce the risk of mood episodes.
Pregnancy and Bipolar Disorder
- Planning and Monitoring: Women with bipolar disorder should work closely with their healthcare team when planning a pregnancy or if they become pregnant. Medication adjustments may be necessary to minimize risks to the baby while managing symptoms.
- Specialist Care: Collaboration with maternity services, including obstetricians, midwives, GPs, and mental health professionals, is recommended to create a comprehensive treatment plan tailored to the individual’s needs during pregnancy and postpartum.
- Breastfeeding Considerations: Some medications used to treat bipolar disorder may affect a mother’s ability to breastfeed. Healthcare professionals can help weigh the benefits and potential risks.
Living with Bipolar Disorder
Living with bipolar disorder can be challenging, but with a well-structured treatment plan and support system, many individuals can manage their symptoms effectively. Support groups, educational resources, and self-management strategies can also help individuals build resilience and lead a stable, meaningful life.
Crisis and Emergency Care
If you or someone you know is experiencing a severe manic or depressive episode or having suicidal thoughts, immediate help should be sought by contacting a healthcare provider, crisis service, or emergency services. The Samaritans and other support lines are available for confidential support and assistance.
Living with bipolar disorder
Living with Bipolar Disorder
Living with bipolar disorder can be challenging due to the extreme mood swings, but with effective treatment, self-help strategies, and support, individuals can manage the condition and lead fulfilling lives. Here is an in-depth look at managing and living with bipolar disorder.
Staying Active and Eating Well
Maintaining a balanced diet and staying physically active is beneficial for everyone but especially important for individuals with bipolar disorder. Regular exercise can help improve mood, reduce anxiety, and combat depressive symptoms. Activities like walking, running, swimming, or yoga can be incorporated into your routine to enhance your physical and mental well-being. Here are key strategies:
- Routine Exercise: Aim for at least 30 minutes of moderate activity most days of the week.
- Healthy Eating: Focus on a nutritious diet that includes fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit processed foods, sugary drinks, and excessive caffeine intake.
- Weight Management: Some medications for bipolar disorder can lead to weight gain or increase the risk of diabetes. Monitoring your weight, eating healthy, and staying active can mitigate these risks.
Self-Care and Self-Management
Self-care involves taking responsibility for your physical and mental health. It is an essential component of managing bipolar disorder, allowing you to become more aware of your moods and triggers. Key aspects include:
- Recognizing Early Warning Signs: Learn to recognize signs of an impending episode, such as changes in sleep patterns, increased irritability, or a sudden burst of energy.
- Stress Reduction: Incorporate stress-relief techniques like mindfulness meditation, deep breathing exercises, or hobbies that you enjoy.
- Sleep Hygiene: Aim for consistent sleep patterns, as disruptions in sleep can trigger episodes.
Self-Management Programs:
- Bipolar UK’s Self-Management Courses: These courses help you understand your triggers, create action plans, and develop coping strategies.
- Coping Strategies: Developing a toolbox of coping mechanisms, such as journaling, connecting with trusted friends, or participating in support groups, can empower you to manage symptoms effectively.
Support Networks and Talking Therapies
- Support Groups: Connecting with others who have similar experiences can reduce feelings of isolation. Many organizations offer online forums and support groups.
- Talking Therapies: Therapies like cognitive behavioral therapy (CBT) can help you develop healthy thought patterns, build coping skills, and manage episodes effectively.
Key Support Organizations:
- Bipolar UK
- Mind
- Rethink Mental Illness
- Samaritans
- SANE
Accessing Mental Health Services
Various services may be available to help you manage bipolar disorder:
- Community Mental Health Teams (CMHTs): Provide ongoing care, assessment, and support.
- Crisis Services: Offer immediate care for acute episodes to prevent hospitalization.
- Early Intervention Teams: Focus on the early stages of psychosis and bipolar disorder to reduce long-term impact.
- Assertive Outreach Teams: Provide intensive support to help individuals maintain their independence.
Avoiding Alcohol and Drugs
Alcohol and drugs can exacerbate symptoms of bipolar disorder. Avoiding these substances is crucial for managing the condition and maintaining stability. Substance use may offer temporary relief but often leads to a worsening of symptoms and impedes effective treatment.
Managing Work and Stress
- Flexible Working Hours: You may need adjustments in your work schedule, such as shorter hours or flexible timing, especially if stress triggers symptoms.
- Know Your Rights: In many countries, laws like the Equality Act protect individuals with mental health conditions from discrimination in the workplace.
Financial Support
- Benefits and Support: You may be eligible for financial support if you’re unable to work due to your condition. Check with your local government agencies for assistance programs, including disability payments.
Caring for Someone with Bipolar Disorder
Caring for a person with bipolar disorder can be challenging. Carers and family members should:
- Seek Support: Join support groups or contact services that provide information and coping strategies for carers.
- Understand Rights: Know the legal rights that apply to mental health care, such as making decisions during crises.
Dealing with Suicidal Thoughts
If you experience suicidal thoughts:
- Seek Immediate Help: Contact your GP, care coordinator, or a mental health crisis service.
- Reach Out to Support Services: Contact the Samaritans or a trusted helpline.
- Talk to Someone: Sharing your feelings can provide immediate relief and open the door to professional help.
Online Communities and Forums
Connecting with others through online communities can be empowering. Examples include:
- SANE Support Forum
- Bipolar UK eCommunity
Living with bipolar disorder requires a multifaceted approach that combines medication, therapy, lifestyle changes, and support from healthcare professionals, family, and peers. With dedication and proper care, individuals with bipolar disorder can achieve stability and lead fulfilling lives.